Abstract
Biological interactions between the bone and the blood vessels are gradually being clarified. To investigate the relationship between bone mineral density and atherosclerosis in hemodialysis patients, we examined the bone mineral density and the intima-media thickness of the carotid artery in 83 dialysis patients with non-diabetic nephropathy (44 men and 39 women) aged from 23 to 83 years. The duration of hemodialysis ranged from 2 to 344 months. The bone mineral density of the radius was measured by dual-energy X-ray adsorptiometry, and the ratio of this value to the standard value for the same age and gender was calculated (Z-score). As an index of atherosclerosis, the intima-media thickness of the carotid artery was measured by high resolution B-mode ultrasonography. Then the relationship between the Z-score and various factors was examined using Spearman's rank correlation analysis and multiple regression analysis. The Z-score showed a negative correlation with the duration of hemodialysis, the carotid intima-media thickness, and the levels of alkaline phosphatase, intact parathyroid hormone, and low-density lipoprotein cholesterol by Spearman's rank correlation analysis. In addition, the Z-score showed a positive correlation with the lipoprotein (a) level and a negative correlation with the duration of hemodialysis, intima-media thickness, intact parathyroid hormone, and low-density lipoprotein cholesterol by multiple regression analysis. These findings suggest that the decrease of bone mineral density in hemodialysis patients is correlated with secondary hyperparathyroidism and hyperlipidemia, which are factors known to promote atherosclerosis, and thus bone density changes might be related to the progression of atherosclerosis, or vice versa.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A significant decrease in bone mineral density (BMD) has been reported in hemodialysis patients when compared with the general population, and this decline of BMD becomes more marked as the duration of dialysis increases [1]. There is also a significant increase in atherosclerosis in dialysis patients when compared with the general population [2, 3].
Recently, it has been recognized that there is a close relationship between bone abnormalities and vasculopathy, with changes of the bone and the blood vessels being regulated by common factors. In postmenopausal women, it has been shown that a decrease of BMD is associated with the progression of atherosclerosis [4]. In addition, a correlation has been found between the BMD and the age-adjusted mortality rate or the death rate from heart failure [5]. However, the relationship between BMD and atherosclerosis has not yet been clarified in hemodialysis patients.
High-resolution B-mode ultrasonography has been widely used to non-invasively assess atherosclerosis of the carotid artery in epidemiologic and clinical studies performed in hemodialysis patients [2, 3], and it is thought that carotid artery changes mirror the progression of systemic atherosclerosis not only in the general population, but also in hemodialysis patients [6].
The present study was performed to investigate the relationship between BMD and atherosclerosis in hemodialysis patients. The radial BMD was measured as an index of osteoporosis and the intima-media thickness (IMT) of the carotid artery was measured as an index of atherosclerosis. Then the correlation between radial BMD and IMT was examined.
Materials and methods
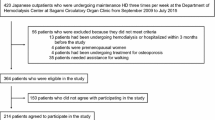
Subjects
We enrolled 83 patients who were on hemodialysis at Harada Hospital (Hiroshima, Japan). We excluded patients with diabetic nephropathy because diabetes mellitus is a major independent risk factor for atherosclerosis. All of the patients were clinically stable and had no acute infection. We also excluded patients who had undergone parathyroidectomy or had a history of heavy aluminum exposure. All of the patients were taking calcium-containing binders and 12 patients who had secondary hyperparathyroidism were receiving treatment with active vitamin D metabolites. The underlying renal disease was chronic glomerulonephritis in 67 patients, nephrosclerosis in ten patients, polycystic kidney disease in two patients, and other conditions in four patients. The patients participated in this study after giving informed consent.
Measurement of radial BMD
We measured the BMD of the distal one-third of the radius by dual-energy X-ray adsorptiometry (DXA) (DOS-600; Aloka, Tokyo, Japan). DXA measurements of the distal radius predominantly reflect cortical bone and the values obtained indicate the bone mass and not the volumetric bone density. In dialysis patients, the potential confounding effect of concurrent soft-tissue calcification on DXA values should be smaller at this site. In addition, the decrease in BMD is significantly greater for cortical bone than for cancellous bone in hemodialysis patients with secondary hyperparathyroidism [7]. The ratio of the actual BMD value measured by DXA to the standard BMD for the same age and gender was calculated to give the normalized value (BMD Z-score) [1]. We used the BMD Z-score to adjust BMD data, in order to compensate for the effect of menopause in postmenopausal female patients [4].
Carotid ultrasonography
Ultrasonography of the carotid artery was performed using a high resolution real-time scanner with a 7.5 MHz transducer (SSA-350; Toshiba, Tokyo, Japan). All subjects were examined by a single trained physician, who was blinded with regard to their clinical characteristics. Examination was performed in the supine position, and the carotid bifurcation and common carotid artery were scanned on both sides.
Scanning was done in three different longitudinal projections as well as the transverse projection. As defined by Wendelhag et al. [8], the IMT was measured at the site of greatest thickness (including plaque) and three measurements made at each site were averaged. Then the highest value among the six average IMT values (three from the left side and three from the right side) was used as the representative value for each patient [9]. To determine the intraobserver variability of IMT measurement, a total of 30 subjects were examined on two different occasions at an interval of 7–14 days. The coefficient of variation was only 2.0%.
Blood pressure
After enrollment in the study, four predialysis blood pressure readings were obtained from each patient. Then the mean arterial pressure was calculated as the diastolic blood pressure plus one-third of the difference between the systolic and diastolic blood pressures, and the average of the four mean values was determined.
Biochemical parameters
Venous blood samples were collected after an overnight fast for measurement of the serum concentrations of alkaline phosphatase, intact parathyroid hormone (intact PTH), calcium, phosphate, total cholesterol, triglycerides, high-density lipoprotein cholesterol (HDL cholesterol), and lipoprotein (a). Intact PTH was measured using the Nichols IRMA kit (Nichols Institute, San Juan Capistrano, Calif., USA). The adjusted calcium level was calculated using Payne's formula and the low-density lipoprotein cholesterol (LDL cholesterol) level was calculated using Friedewald's formula [10].
Statistical analysis
All results are shown as the mean±SD and statistical analysis was performed by the Mann-Whitney U-test. We used Pearson's correlation coefficient analysis to examine the relationship between the radial BMD Z-score and the IMT, as well as between the BMD Z-score and intact PTH. We also examined the relationship between the radial BMD Z-score and the following factors using Spearman's rank correlation analysis: duration of hemodialysis, body mass index, IMT value, systolic blood pressure, diastolic blood pressure, mean arterial pressure, and levels of alkaline phosphatase, intact PTH, adjusted calcium, serum phosphate, total cholesterol, triglycerides, HDL cholesterol, LDL cholesterol, and lipoprotein (a). Furthermore, multiple regression analysis was performed to evaluate possible predictors of the radial BMD Z-score. The variables tested were duration of hemodialysis, body mass index, IMT value, mean arterial pressure, and levels of PTH, adjusted calcium, serum phosphate, LDL cholesterol, and lipoprotein (a). Finally, multiple regression analysis was performed to evaluate possible predictors of the IMT value, which included age, gender (male), duration of hemodialysis, and intact PTH level. Analyses were performed with StatView 5 software (Abacus Concepts, Inc., Calif., USA) and P<0.05 was considered to indicate a significant difference.
Results
Table 1 summarizes the clinical and biochemical parameters of the subjects. There were 44 men and 39 women aged from 23 to 83 years, with a mean age of 54.0±13.0 years. The duration of hemodialysis ranged from 2 to 344 months, with a mean of 89.7±80.7 months. A significant difference was observed between men and women with respect to radial BMD (P<0.0001), total cholesterol level (P=0.0432), and lipoprotein (a) level (P=0.0248).
The radial BMD Z-score showed a negative correlation with the IMT value according to Pearson's correlation coefficient analysis (R 2=0.113, P=0.0019, Fig. 1). The BMD Z-score was also negatively correlated with the intact PTH level (Pearson's R 2=0.168, P=0.0001, Fig. 2). The factors assessed for a relationship with the radial BMD Z-score by Spearman's rank correlation analysis are shown in Table 2. There was a negative correlation with the duration of hemodialysis, the IMT value, the alkaline phosphatase level, the intact PTH level, and the LDL cholesterol level. Positive correlations were seen with the body mass index and the lipoprotein (a) level, but these did not reach significance.
The results of multiple regression analysis of predictors of the radial BMD Z-score are summarized in Table 3. The BMD Z-score showed a positive correlation with lipoprotein (a) level, while there were negative correlations with duration of hemodialysis, IMT value, intact PTH level, and LDL-cholesterol level.
In addition, the results of multiple regression analysis of predictors of the IMT are summarized in Table 4. The IMT value showed a positive correlation with age and intact PTH level, but there was no correlation with gender or with duration of hemodialysis.
Discussion
In the present study, the radial BMD Z-score showed a positive correlation with the lipoprotein (a) level, while there was a negative correlation with duration of hemodialysis, IMT value, and levels of alkaline phosphatase, intact PTH, and LDL cholesterol.
It was previously reported that the BMD measured at the femoral neck and lumbar spine showed a positive correlation with the serum phosphate level, while showing a negative correlation with the duration of hemodialysis, PTH level, and alkaline phosphatase level [11]. Although there was no correlation with serum phosphate in the present study, our findings confirmed the other relationships. Furthermore, our study showed that the radial BMD Z-score was correlated with IMT value, LDL cholesterol level, and lipoprotein (a) level.
An increased lipoprotein (a) level is a major risk factor for cardiovascular disease. In a young and healthy population, Thorsen et al. [12] found a positive correlation between femoral neck BMD and lipoprotein (a) level. Lipoprotein (a) is thought to be involved in tissue maintenance or repair, but its relationship with BMD has not been confirmed in adults. In the present study, there was a positive correlation between radial BMD Z-score and lipoprotein (a) level, suggesting that lipoprotein (a) may play a role in strengthening the bones of hemodialysis patients.
Parhami et al. [13] reported that lipid peroxidation products have opposing effects on vascular cells and bone cells, showing that oxidized LDL caused an increase of arterial calcification, but decreased bone mineralization in vitro. Similarly, our study showed a negative correlation between the radial BMD Z-score and LDL cholesterol level. Accordingly, a high LDL cholesterol level might not only be a risk factor for the formation of atherosclerotic plaque, but also for a decrease in BMD.
In the present study, the intact PTH level was significantly correlated with the radial BMD Z-score and with the carotid IMT value. In hemodialysis patients, the IMT was previously reported to show a positive correlation with age, smoking, serum phosphorus, and PTH [2]. On the other hand, the decrease in radial BMD in hemodialysis patients has been ascribed to secondary hyperparathyroidism leading to bone demineralization [7]. Therefore, secondary hyperparathyroidism may be a shared risk factor for the progression of atherosclerosis and for the decrease of BMD. Because atherosclerosis increases in hemodialysis patients at the same time as they develop osteoporosis, it seems possible that the two conditions may be more closely related than has been realized so far.
In hemodialysis patients, vascular abnormalities are due to both atherosclerosis and Mönckeberg's medial calcific sclerosis. With regard to calcification in the media wall of arteries, Nishizawa et al. [14] have suggested a relationship between the calcification of arterial plaque and decrease of BMD in hemodialysis patients. In addition, there is a correlation between calcification of arterial plaque and non-HDL cholesterol level. Ectopic calcification of the arteries might lead to ischemia of various organs. In young hemodialysis patients, a strong association between coronary artery calcification and a high calcium×phosphate product was detected by a study using electron-beam computed tomography [15]. These studies indicate that the treatment of abnormal mineral metabolism is necessary to prevent vascular abnormalities.
There are several factors that seem to be common to the development of osteoporosis and vascular abnormalities. Both bone and atherosclerotic arteries contain osteopontin, bone morphogenetic protein, matrix Gla protein, type I collagen, and osteonectin. Asou et al. [16] prepared osteopontin knockout mice, and showed that osteopontin is required for angiogenesis, osteoclast recruitment, and subsequent resorption of bone. Min et al. [17] studied osteoprotegerin knockout mice, and found that osteoprotegerin reverses osteoporosis by inhibiting the activity of endosteal osteoclasts and also prevents arterial calcification. In addition, it has been shown that PTH, PTH-related peptide, and tumor growth factor-β can regulate the calcification of vascular cells in vitro.
In hemodialysis patients, vitamin K may be the most interesting factor. Vitamin K is also an essential cofactor for the site-specific carboxylation of matrix Gla protein and osteocalcin [18]. Luo et al. [19] created matrix Gla protein knockout mice. These mice showed the phenotype of warfarin-induced bone abnormalities. In addition, all of the animals developed severe calcification of the major arteries and died within 6–8 weeks after birth due to rupture of the thoracic or abdominal aorta. This study clearly showed the vital importance of matrix Gla protein for preventing vascular calcification. The fact that matrix Gla protein expression is strongly induced in both atherosclerosis and Mönckeberg's medial calcific sclerosis suggests that contact between tissues and calcium salt crystals is a common trigger in both processes. Vitamin K2 increases bone formation and decreases bone resorption, and the vitamin K level is significantly reduced in dialysis patients [20]. Moreover, it has been reported that the fracture rate increases as the vitamin K level declines in hemodialysis patients [21]. Vitamin K1 is found in green-yellow vegetables, while vitamin K2 is found in fermented foods such as cheese. In hemodialysis patients, it is thought that intake of vitamin K is insufficient because of restrictions on the dietary intake of potassium and phosphate. Therefore, there is a possibility that arterial calcification and bone loss (a decrease in BMD) may show simultaneous progression in dialysis patients, and these observations suggest that osteoporosis and atherosclerosis may share some common mechanisms.
In conclusion, the present study revealed that the decrease of BMD in hemodialysis patients is correlated with secondary hyperparathyroidism and hyperlipidemia, which have been proven to promote atherosclerosis, and thus might be related to atherosclerosis.
References
Fontain MA, Albert A, Dubois B et al. (2000) Fracture and bone mineral density in hemodialysis patients. Clin Nephrol 54:218–226
Kawagishi T, Nishizawa Y, Konishi T et al. (1995) High-resolution B-mode ultrasonography in evaluation of atherosclerosis in uremia. Kidney Int 48:820–826
Kennedy R, Case C, Fathi R et al. (2001) Does renal failure cause an atherosclerotic milieu in patients with end-stage renal disease? Am J Med 110:198–204
Uyama O, Yoshimoto Y, Yamamoto Y et al. (1997) Bone changes and carotid atherosclerosis in postmenopausal women. Stroke 28:1730–1732
von der Recke P, Hansen MA, Hassager C (1999) The association between low bone mass at the menopause and cardiovascular mortality. Am J Med 106:273–278
Benedetto FA, Mallamaci F, Tripepi G et al. (2001) Prognostic value of ultrasonographic measurement of carotid intima media thickness in dialysis patients. J Am Soc Nephrol 12:2458–2464
Katagiri M, Takahiro O, Harada T et al. (1994) Bone loss and bone metabolic markers in hyperparathyroidism. J Bone Miner Metab Suppl 12:81–85
Wendelhag I, Wiklund O, Wikstrand J (1993) Atherosclerotic changes in femoral and carotid arteries in familial hypercholesterolemia: ultrasonographic assessment of intima-media thickness and plaque occurrence. Arterioscler Thromb 13:1404–1411
Yamasaki Y, Kodama M, Nishizawa H et al. (2000) Carotid intima-media thickness in Japanese type 2 diabetic subjects: predictors of progression and relationship with incident coronary heart disease. Diabetes Care 23:1310–1315
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Taal MW, Masud T, Green D et al. (1999) Risk factors for reduced bone density in haemodialysis patients. Nephrol Dial Transplant 14:1922–1928
Torsen K, Nordstrom P, Lorentzon R et al. (1999) The relation between bone mineral density, insulin-like growth factor 1, lipoprotein (a), body composition, and muscle strength in adolescent males. J Clin Endocrinol Metab 84:3025–3029
Parhami F, Morrow AD, Balucan J et al. (1997) Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation. Arterioscler Thromb Vasc Biol 17:680–687
Nishizawa Y, Morii H (1997) Osteoporosis and atherosclerosis in chronic renal failure. Osteoporosis Int Suppl 7:188–192
Goodman WG, Goldin J, Kuizon BD et al. (2000) Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 342:1478–1483
Asou Y, Rittling SR, Yoshitake H et al. (2001) Osteopontin facilitates angiogenesis, accumulation of osteoclasts, and resorption in ectopic bone. Endocrinology 142:1325–1332
Min H, Morony S, Sarosi I et al. (2000) Osteoprotegerin reverses osteoporosis by inhibiting endosteal osteoclasts and prevents vascular calcification by blocking a process resembling osteoclastogenesis. J Exp Med 192:463–474
Shearer MJ (1995) Vitamin K. Lancet 345:229–234
Luo G, Ducy P, McKee MD et al. (1997) Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature 386:78–81
Shino M (1988) Determination of endogenous vitamin K (phylloquinone and menaquinone-n) in plasma by high-performance liquid chromatography using platinum oxide catalyst reduction and fluorescence detection. Analyst 113: 393–397
Kohlmeier M, Saupe J, Shearer MJ et al. (1997) Bone health of adult hemodialysis patients is related to vitamin K status. Kidney Int 51:1218–1221
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakashima, A., Yorioka, N., Tanji, C. et al. Bone mineral density may be related to atherosclerosis in hemodialysis patients. Osteoporos Int 14, 369–373 (2003). https://doi.org/10.1007/s00198-002-1361-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-002-1361-4