Abstract
Introduction and hypothesis
Faecal incontinence can be a devastating outcome with social, psychological and physical repercussions, and it occurs in 10–61% following obstetric anal sphincter injury (OASIS). The aim of our study was to determine the contributing factors in the development of severity of OASIS and to correlate anal sphincter tone with the extent of anal sphincter injury.
Methods
A prospective cohort study was performed of all patients attending the postnatal perineal clinic at 4–12 months postpartum, from January 2016 until October 2017. Women were categorised into minor tears (3a and 3b) and major tears (3c and 4th degree).
Results
The mean age was 33.9 years (4.2); the mean parity was 1.6 (range 1–5). A total of 75 women (17%) were reviewed following a major tear (4th degree, n = 28, 3c, n = 47) and 362 (83%) were reviewed following a minor tear (3a n = 188, 3b, n = 174). Following analysis of numerous obstetric variables, it was shown that women who had an instrumental delivery were more likely to have a major tear compared with those who had a spontaneous vaginal delivery (p = 0.05). A significant difference was found in the distributions of symptom score between groups (p < 0.001). Women with combined defects were most likely to have reduced anal tone (p < 0.001) compared with any other group.
Conclusions
The perineal clinic provides a valuable resource for investigation and treatment of OASIS, providing a targeted pathway for management. We suggest that endoanal ultrasound and digital rectal examination are complimentary investigations which correlate well with each other.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstetric anal sphincter injury (OASIS) occurs in 3% of primiparous women and 0.8% of multiparous women [1]. Faecal incontinence can be a devastating outcome for women following OASIS and has a significant impact on social, psychological and physical well-being. It occurs in 10–61% following OASIS [2, 3]. Faecal incontinence is more likely to occur following fourth degree tear (31%) than following third degree tear (15%) [4]. Other effects of OASIS include dyspareunia and perineal pain [5, 6]. Subsequent vaginal deliveries can have a deleterious effect on sphincter function, resulting in both subjective and objective anal function deteriorating further over time [7]. Worsening faecal symptoms occur in 17–24% of women following a second vaginal delivery [8]. These difficulties along with the problems posed in managing subsequent deliveries make this relatively small group of patients a complex one.
One would assume that women with an increased grade of tear would have a greater severity of incontinence and reduction in anal tone. There is however conflicting evidence in the literature supporting this. Some studies have shown worse incontinence in women with an increased grade of tear [9,10,11]; however, these studies compared fourth and third degree tears and did not differentiate between grade of third degree tear (3a vs. 3b vs. 3c). Other studies have not shown this relationship [12, 13]. The aim of our study was to determine the contributing factors in the development of the severity of OASIS and to use endo-anal ultrasound (EAUS) and digital rectal tone examination to correlate anal sphincter tone with the extent of anal sphincter injury.
Methods
This was a prospective study of women who sustained OASIS and underwent immediate surgical repair and were followed up in the perineal clinic of the National Maternity Hospital in Dublin at 4–12 months postpartum from January 2016 until October 2017. Severity of tear was defined using the accepted classification of OASIS as is described by Sultan (1999) [14]. This categorises OASIS into four grades: grade 3a, which has < 50% external anal sphincter (EAS) damage, grade 3b, which has > 50% EAS damage, and 3c, which has internal anal sphincter (IAS) and EAS damage. Fourth degree tears involve the anal sphincter as well as the anorectal epithelium.
Women who attended the Perineal Clinic completed the St. Mark Questionnaire (MHQ). This questionnaire scores symptoms of flatus, solid and liquid stool incontinence from 0 (never) to 4 (always). Other factors accounted for in the score are alteration in lifestyle, the need for constipating agents and, very importantly, the degree of faecal urgency, if present. A score of 0 implies complete continence and a score of 24 complete incontinence [15].
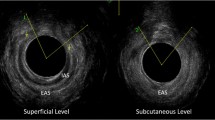
Women underwent endoanal ultrasound (EAUS) examination and assessment of tone using digital rectal examination (DRE); both examinations were carried out with the patients in the left lateral position. These assessments were carried out by and interpreted by a single physician with long-standing experience in follow-up of OASIS. Two- and three-dimensional images were collected and reviewed at three levels: the deep, superficial and subcutaneous layers of the sphincter mechanism. A defect of the IAS or EAS was defined as a defect > 1 h of a 12-h clock. Defects were categorised into < 1 quadrant, 1–2 quadrants, intact or scar only (defect < 1 h of a 12-h clock). Digital examination categorised tone as normal, reduced, increased or poor technique. Women were further categorised into minor tears involving damage to EAS only (3a and 3b) and major tears involving damage to IAS and EAS (3c and 4th degree).
Medical records were used to assess demographic data including maternal age, parity at time of delivery, mode of delivery, use of mediolateral episiotomy (MLE), induction, epidural anaesthesia, length of second stage of labour, occipito-posterior presentation, shoulder dystocia and neonatal birth weight.
Ethics
This study was conducted according to ethical guidelines and was approved by the Research Ethics Committee in the National Maternity Hospital.
Statistical analysis
Data were analysed using SPSS v.24. Descriptive statistics appropriate to the variable type and distribution are presented. For comparison between groups the two-sample t-test, Wilcoxon rank sum test and chi-square test were used as appropriate. A p value < 0.05 indicates a finding of significance. Multivariable analysis using logistic regression was considered, but deemed unnecessary in view of the results of bivariate analysis.
Results
A total of 437 women were referred with a mean age of 33.9 years (4.2), parity of 1.6 (range 1–5). Thirty-seven per cent of these women were referred from another unit. These women were followed up at 4–12 months. A total of 75 women (17%) were reviewed following a major tear (4th degree, n = 28, 3c, n = 47) and 362 (83%) were reviewed following a minor tear (3a n = 188, 3b, n = 174). Of the 437 women, 54% had an SVD (spontaneous vaginal delivery); 16% had a forceps delivery; 18% had a ventouse delivery; 12% had a combined forceps/ventouse delivery; 5% had a VBAC (vaginal birth after caesarean section); 21% were induced; 62% had an epidural; 40.7% underwent a mediolateral episiotomy (MLE); 15% had a rapid labour; 13% had an occipito-posterior presentation and 3% had a shoulder dystocia.
There was no significant difference between the above variables as shown in Table 1 regarding the difference in grade of tear (minor vs. major) with the exception of SVD versus instrumental delivery. There was a trend towards having a major tear in women with an instrumental delivery compared with those who had a spontaneous vaginal delivery (p = 0.05) using a one-sided two-sample t-test. Table 2 compares the postpartum outcomes between major and minor tears. A significant difference was found in the distributions of symptom score between groups (p < 0.001). Women with less severe tears had a median symptom score of 0 (median 0–2) and women with more severe tears had a median symptom score of 2 (median 0–5). Reassuringly the level of continence difficulties in our cohort was low. There was also a significant difference between anal tone in women with minor and major tears. Women with major tears had lower anal tone on DRE (p < 0.01).
One hundred nine women (25%) had apareunia or dyspareunia. Of those 109 women, 55 had dyspareunia, 12 had apareunia and 42 (9%) of the women had not attempted intercourse at the time of attending the clinic. Seventy-nine (18%) of the women had symptoms of urinary incontinence, of which 55 (70%) had stress urinary incontinence (SUI), 15 (19%) had urge urinary incontinence (UUI) and 9 (11%) had mixed urinary incontinence (MUI).
Table 3 compares mode of delivery with or without MLE. In women with a major tear who had a forceps delivery, those who did not have an MLE were 1.7 times more likely to have a major tear compared with those who did have an MLE. In women with a major tear who had a ventouse delivery, those who did not have an MLE were 2.7 times more likely to have a major tear compared with those who did have an MLE.
EAUS was used to assess the severity of sphincter damage. Table 4 shows the relationship between severity of tear and sphincter defect found on EAUS. A total of 437 women were referred to the clinic. EAUS was carried out in 367 women (the remainder had had scans prior to referral). Interestingly, 61 (20%) women classed as having a minor tear also had an IAS defect on EAUS. This suggests an unidentified IAS tear in this group and therefore a misclassification into a milder tear category. Nineteen (33%) women classed as having major tears had an intact IAS on EAUS, suggesting a misclassification into a more severe tear category. EAS findings largely reflect what one would expect to find according to the grade of tear as the EAS is easier to assess because of its larger size. The number of completely intact EAS (n = 25, 8%) in the minor tear group suggests an overcall of an OASIS.
The relationship between severity of sphincter defect on EAUS and tone on DRE is shown in Table 5. The extent of EAS or IAS damage was directly correlated to anal tone, with women sustaining combined defects being more likely to have reduced tone (p < 0.001). This table categorises women according to severity of tear on IAS and EAS based on EAUS findings: intact, scar/< 1 quadrant defect, 1–2 quadrant defects. Women with larger quadrant defects on IAS and EAS were more likely to have reduced tone on DRE (p < 0.001). Women with a combined IAS and EAS defect of 1–2 quadrants each are 3.8 times more likely to have reduced tone than women with an intact IAS and EAS with scar or < 1 quadrant defect. Women with combined defects were most likely to have reduced anal tone (p < 0.001) than any other group.
Discussion
In our study we found there was a trend towards women undergoing instrumental delivery being more likely to have a major (3c/ fourth degree) tear than those who had an SVD (p = 0.05). There was no significant difference in any other variables in respect to severity of tear. Significant risk factors for OASIS include operative vaginal delivery, persistent occiput-posterior position and foetal macrosomia [14, 16, 17]. A study by Smith [17] showed that a longer duration of the second stage of labour was associated with a 40% increase in the odds of OASIS for each minute (log) increased in the second stage of labour, and each 100-g increase in birthweight was also associated with a 10% increase in odds of OASIS (p < 0.05). A study by Laine et al. [18] showed that perineal body length < 3.5 cm and second stage of labour > 99 min were the most predictive of OASIS. Epidural anaesthesia has been shown to be associated with a reduced risk of OASIS [17, 19]. Head control by slowing down the delivery of the head through instruction of women not to push at crowning has also been shown to reduce the incidence of OASIS [18, 20].
Studies have shown that MLE is protective against OASIS when ventouse or forceps delivery is performed but there was no significant difference in women with a spontaneous vaginal delivery (Jangö, 2014). A study by de Vogel [21] showed a six-fold reduction in incidence of OASIS when MLE is performed at the time of operative vaginal delivery.
The risk of pelvic organ prolapse, stress urinary incontinence and sexual dysfunction is higher in women who sustain OASIS [22]. A study by O’Shea et al. [23] reported that up to half of women reported sexual dysfunction at 3 years post OASIS using the Female Sexual Functioning Index. In our study, 18.2% reported urinary incontinence, and 25% had sexual dysfunction. These are issues that may not always be addressed postnatally. In our group it was seen that 9.4% of women had not attempted sexual intercourse at the time of attending the perineal clinic for a variety of psychological and physical reasons. The level of dyspareunia and apareunia in this group of women is high and certainly under-reported. Having a dedicated perineal clinic allows time for debriefing and discussion regarding sexual intimacy and appropriate referral for psychosexual counselling can be arranged. The clinic provides an opportunity to address this issue and deals with it before it becomes a debilitating problem. Future studies addressing this are needed to investigate the role OASIS may play in the development of long-term sexual dysfunction.
Endoanal ultrasound (EAUS) is considered the gold standard for evaluation of anal sphincter defects in women with faecal incontinence, and it is a simple, inexpensive tool which is well tolerated and easily reproducible [24]. However it is important to take a detailed history of symptoms from the woman to include obstetric history, category of incontinence (faecal vs. flatal) and type of incontinence (urge vs. passive). This should be combined with DRE to determine resting pressure and squeeze pressure. Discriminating different types of faecal incontinence may point towards the site of damage although often it is a mixed picture. Faecal urge incontinence is often associated with EAS damage and reduced squeeze pressures or reduced rectal capacity. Passive faecal incontinence on the other hand is associated with IAS damage and low resting pressure [25]. This information can predict the expected sphincter damage even before the EAUS is performed.
Different scoring systems have been developed to categorise the severity of sphincter injury. Starck et al. [26] graded tears from 0 to 16, with 0 indicating no defect and 16 indicating an 180-degree defect of the whole length of both IAS and EAS. A simpler grading system was developed by Norderval et al. [27] whereby a maximum score of 7 was assigned to a defect of both the EAS and IAS exceeding 90 degrees in the axial plane and involving more than half of the length of each sphincter. Women with combined defects of the IAS and EAS were at a higher risk of faecal incontinence [9]. In our study, the extent of EAS or IAS damage was directly correlated to anal tone, with women having combined defects being more likely to have reduced tone (p < 0.001). Women with major tears were significantly more likely to have endosonographic IAS defects or combined IAS and EAS defects (p < 0.001).
There are mixed views on the sensitivity and correlation between digital rectal examination (DRE) and manometry. However studies have shown increased correlation between DRE and EAUS based on the size of the sphincter defect. DRE sensitivity increases linearly from small to extensive EAS defects (p = 0.001) [28]. In our study a single physician with long-standing experience in EAUS and DRE carried out all assessments of anal tone. Despite its usefulness for research and academic purposes, it is the experience and opinion of the authors that manometry can demoralise patients. They may have significant symptomatic improvement but only marginal increases on pressure readings. For this reason it is not routinely performed in our clinic.
In our study 20% of women with a minor tear also had an IAS defect, suggesting an unidentified IAS tear and suboptimal repair. No matter how good a repair of the IAS is undertaken, there will always be some sonographic evidence of a scar. These results show the practical difficulty in accurately assessing the IAS in the immediate postpartum period. In addition to this, a number of women with major tears had an intact IAS, suggesting a misclassification into a more severe tear category. A metanalysis by Oberwalder [29] found an incidence of occult sphincter injury in 26.9% of primiparous women and 8.5% of multiparous women. One third of these women were symptomatic. The peak incidence of faecal incontinence is in the 5th and 6th decades, which may be as a result of the cumulative effects of menopause and cumulative effects of deliveries and ageing [30]. It is important to identify the full magnitude of the injury at the time of primary repair and identify and repair IAS defects as competently as possible. While levels of incontinence were small in this study, the better the repair at the time of sphincter injury was, the more likely the prevention of development of symptoms in the future.
Strengths of this study include the use of a validated incontinence questionnaire (St. Marks Incontinence Score), which allows differentiation of incontinence type based on patients' self-reporting. Furthermore, it allows subdivision based on severity of symptoms: (0–4, 5–8, > 8) with mean quality of life domain scores being higher with increasing scores. The St. Mark’s Incontinence Score (SMIS) has shown the highest correlation with the physician’s clinical impression of the severity of anal incontinence (Roos, 2009, Vaizey, 1999). Another strength of our study is the numbers enrolled and the length of follow-up. All patients were reviewed at each visit by a single consultant gynaecologist showing a consistent work-up and uniformity of EAUS assessments and digital rectal examination for rectal tone. Weaknesses of the study include the presentation at birth not being documented in 51% of cases. Some women were referred from other hospitals and the position at the time of delivery; the length of labour and length of second stage were not available.
Conclusion
The perineal clinic provides a valuable resource for investigation and treatment of postpartum perineal injury, providing a targeted pathway for management. Instrumental delivery was a significant risk factor compared with SVD for severity of tear, with women who had an instrumental delivery being significantly more likely to have a major tear than those who had an SVD (p = 0.05). The overall level of faecal incontinence symptoms in our population was low, which is reassuring and perhaps reflective of the emphasis placed on the management of these tears in our unit. However, the level of sexual dysfunction in this group of women was high and certainly under-reported. The clinic provides an opportunity to address this issue and deal with it before it becomes a debilitating problem. The extent of EAS and IAS damage evident on ultrasound was directly related to severity of tear. However, there is evidence of misclassification of tears regarding the IAS sphincter, reflecting the difficulty in identifying this small muscle. It is important to identify the full magnitude of the injury at the time of primary repair and identify and repair IAS defects as competently as possible. While levels of incontinence were small in this study, the better the repair in the present, the more likely the prevention of development of symptoms in the future. Women who had large defects on EAUS had poorer anal tone than those who had smaller defects or scar only and women with combined defects were more likely to have reduced anal tone. We suggest that EAUS and DRE are complimentary investigations which correlate well with each other.
References
Harkin R, Fitzpatrick M, O'Connell PR, O'Herlihy C. Anal sphincter disruption at vaginal delivery: is recurrence predictable? Eur J Obstet Gynecol Reprod Biol. 2003;109:149–52.
Reid AJ, Beggs AD, Sultan AH, Roos A-M, Thakar R. Outcome of repair of obstetric anal sphincter injuries after three years. Int J Gynaecol Obstet. 2014;127(1):47–50.
Sultan AH, Thakar R. Third and fourth degree tears. In: Sultan AH, Thakar R, Fenner DE, editors. Perineal and anal sphincter trauma: diagnosis and clinical management. London: Springer; 2007. p. 33–51.
Jangö H, Langhoff-Roos J, Rosthøj S, Saske A. Long-term anal incontinence after obstetric anal sphincter injury-does grade of tear matter? Am J Obstet Gynecol. 2018;218(2):232.e1–232.e10.
Brubaker L, Handa VL, Bradley CS, Connolly A, Moalli P, Brown MB, et al. Sexual function 6 months after first delivery. Obstet Gynecol. 2008;111:1040–4.
Signorello LB, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: a retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184:881–8.
Fornell EU, Matthiesen L, Sjödahl R, Berg G. Obstetric anal sphincter injury ten years after: subjective and objective long term effects. BJOG. 2005;112(3):312–6.
Royal College of Obstetricians and Gynaecologists (RCOG). The management of third- and fourth-degree perineal tears. RCOG guideline 2015 (revised). RCOG Press; 2015.
Nichols CM, Lamb EH, Ramakrishnan V. Differences in outcomes after third- versus fourth-degree perineal laceration repair: a prospective study. Am J Obstet Gynecol. 2005;193(2):530–6.
Sangalli MR, Floris L, Falting D, Weil A. Anal incontinence in women with third or fourth degree perineal tears and subsequent vaginal deliveries. Aust N Z J Obstet Gynaecol. 2005;193:530–6.
De Leeuw JW, Vierhout ME, Struijk PC, Hop WC, Wallenburg HC. Anal sphincter damage after vaginal delivery: functional outcome and risk factors for fecal incontinence. Acta Obstet Gynecol Scand. 2001;80(9):830–4.
Norderval S, Nsubuga D, Bjelke C, Frasunek J, Myklebust I, Vonen B. Anal incontinence after obstetric sphincter tears: incidence in a Norwegian county. Acta Obstet Gynecol Scand. 2004;83:989–94.
Starck M, Bohe M, Valentin L. The extent of endosonographic anal sphincter defects after primary repair of obstetric sphincter tears increases over time and is related to anal incontinence. Ultrasound Obstet Gynecol. 2006;27:188–97.
Sultan AH. Obstetrical perineal injury and anal incontinence. Clin Risk. 1999;5:193–6.
Vaizey CJ, Caraped E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut. 1999;44(1):77–80.
Christianson LM, Bovbierg VE, McDavitt EC, Hullfish KL. Risk factors for perineal injury during delivery. Am J Obstet Gynecol. 2003;189(1):255–60.
Smith LA, Price N, Simonite V, Burns EE. Incidence of and risk factors for perineal trauma: a prospective observational study. BMC Pregnancy Childbirth. 2013;13:59.
Laine K, Pirhonen T, Rolland R, Pirhonene J. Decreasing the incidence of anal sphincter tears during delivery. Obstet Gynecol. 2008;111:1053–7.
Jangö H, Langhoff-Roos J, Rosthøj S, Sakse A. Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population-based cohort study. Am J Obstet Gynecol. 2014;210:59.
Hals E, Oian P, Pirhonen T, Gissler M, Hjelle S, Nilsen EB, et al. A multicenter interventional program to reduce the incidence of anal sphincter tears. Obstet Gynecol. 2010;116:901–8.
De Vogel J, van der Leeuw-van Beek A, Gietelink D, Vuijkovic M, de Leeuw JW, van Bavel J. The effect of a mediolateral episiotomy during operative vaginal delivery on the risk of developing obstetrical anal sphincter injuries. Am J Obstet Gynecol. 2012;206(5):404.
Borello-France D, Burgio KL, Richter HE, Zyczynski H, Fitzgerald MP, Whitehead W, et al. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108(4):863–72.
O’Shea MS, Lewicky-Gaupp C, Gossett DR. Long-term sexual function after obstetric anal sphincter injuries. Female Pelvic Med Reconstr Surg. 2018;24(2):82–6.
Albuquerque A. Endoanal ultrasonography in fecal incontinence: current and future perspectives. World J Gastrointest Endosc. 2015;7(6):575–81.
Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109:1141–57.
Starck M, Bohe M, Valentin L. Results of endosonographic imaging of the anal sphincter 2–7 days after primary repair of third- or fourth-degree obstetric sphincter tears. Ultrasound Obstet Gynecol. 2003;22:609–15.
Norderval S, Mækskog A, Røssaak K, Vonen B. Correlation between anal sphincter defects and anal incontinence following obstetric sphincter tears assessment using scoring systems for sonographic classification of defects. Ultrasound Obstet Gynecol. 2008;31:78–84.
Dobben AC, Terra MP, Deutekom M, Gerhards MF, Bijnen AB, Felt-Bersma RJ, et al. Anal inspection and digital rectal examination compared to anorectal physiology tests and endoanal ultrasonography in evaluating fecal incontinence. Int J Color Dis. 2007;22:783–90.
Oberwalder M, Connor J, Wexner SD. Metanalysis to determine the incidence of obstetric anal sphincter damage. Br J Surg. 2003;90:1333–7.
Johnson JK, Lindow SW, Duthie GS. The prevalence of occult obstetric anal sphincter injury following childbirth—literature review. J Matern Fetal Neonatal Med. 2009:547–54.
Acknowledgements
This study describes original work and has not been submitted for consideration by any other journal. All authors have approved the manuscript and its submission. All authors have contributed substantially to obtaining and analysing data obtained for this study. All authors have had input both drafting and revision of the article and final approval of the version published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anglim, B., Kelly, L. & Fitzpatrick, M. Risk factors and outcome of repair of obstetric anal sphincter injuries as followed up in a dedicated perineal clinic. Int Urogynecol J 30, 1649–1655 (2019). https://doi.org/10.1007/s00192-019-03960-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03960-7


