Abstract
Introduction and hypothesis
The purpose of our study was to identify the most common reasons why postoperative urogynecology patients called their surgeon within the first 6 weeks of surgery. We hypothesize that implementing a follow-up postoperative call (FPC) policy would decrease the number of patient-initiated calls within this postoperative period.
Methods
This is a prospective before-and-after cohort study that was conducted in two phases. The initial phase identified the most common reasons why patients call within 6 weeks of their inpatient or outpatient urogynecological surgery. In the second phase, an intervention was implemented where each postoperative patient was called within 48 to 72 h of discharge: the intervention group. The primary outcome was the number of phone calls initiated by patients during the 6-week postoperative period.
Results
There were 226 patients in the control group and 233 patients in the intervention group. Significantly fewer calls were initiated by patients in the intervention group, both groups having a median of 1 call per person, range 0–8 in the control group and 0–10 in the intervention group (p = 0.04). The five most common complaints were as follows: pain (20.4%), medication management (17.4%), disability paperwork (15.5%), and laboratory results (11.5%). There was a significant reduction in calls concerning constipation, laboratory/pathology results, and disability insurance claims after implementing the FPC policy.
Conclusions
The implementation of the FPC policy resulted in fewer patient-initiated calls. As such, there were significant reductions in postoperative complaints of constipation, vaginal bleeding, incomplete bladder emptying, and inquiries into laboratory results and disability paperwork.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorders in the form of urinary incontinence, fecal incontinence, and pelvic organ prolapse affect approximately 25% of the female population of the USA in one form or another, and are ultimately surgically managed in 10–11% [1]. Postoperative complications arising from urogynecological surgery range from a reoperation incidence of 0.9% and readmission rates as high as 4.6% to uncomplicated urinary tract infections at a rate of 31.2% [2, 3].
To minimize or identify complications earlier in the postoperative course, other disciplines such as anesthesia, general surgery, and cardiothoracic surgery have implemented telephone follow-up for same-day procedures. Previous studies show conflicting data on the appropriate time to call patients and whether there is any benefit to making follow-up calls [4,5,6,7,8].
The purpose of our study was to identify the most common reasons for postoperative calls within the first 6 weeks of urogynecological surgery. Once these reasons have been identified, we hypothesize that implementing a follow-up postoperative call (FPC) policy would decrease the number of complaints and patient-initiated calls within this postoperative period.
Materials and methods
This was an Institutional Review Board-exempt (HRP-216) prospective before-and-after cohort study of postoperative complaints conducted in two phases. The initial phase identified the most common reasons why patients called within 6 weeks of their inpatient or outpatient urogynecological surgery; this was the control group. In the second phase, an intervention was implemented where each postoperative patient was called after the surgery; this was the intervention group. Both phases of the study were conducted from 1 July 2015 to 30 April 2017. All surgeries were performed within the Division of Urogynecology at the Atlantic Health System, Morristown, and Summit, NJ, USA. One of four fellowship-trained urogynecological surgeons and a fellow performed each surgery.
Our electronic medical record (EMR) system, Epic©, was used to identify all surgical patient phone calls and the reasons prompting the calls. Information collected included age, parity, comorbidities, preoperative diagnoses, procedures performed, the date, and reasons for calls and interventions. If a single call referenced multiple complaints, each complaint was categorized separately, but the call was counted as one phone call. Study data were collected and managed using REDCap electronic data capture tools hosted at the Atlantic Health System.
After the initial phase of the study, the reasons for postoperative calls were identified and the FPC policy was implemented. Each surgical patient was called by one of the operating fellows within 48 to 72 h of discharge based on previous studies in cardiothoracic orthopedic and general surgery [5, 7, 9]. The purpose of the call was to evaluate whether the patient had adequate pain control, adequate bowel and bladder function, and questions concerning postoperative restrictions and expectations. In addition, each patient was asked about systemic symptoms such as fevers, chills, nausea, vomiting, signs of infection or bleeding. If there were pathology results, they were relayed to the patient during the call.
A call was defined as talking to the person on the telephone within 72 h of being discharged from the hospital. If the patient called the office before being called by the operating fellow, this was considered a postoperative complaint call, but was also considered to have had appropriate contact with the practice within 48–72 h of discharge. Each encounter was documented in the EMR. All data collection was performed and recorded in the exact same fashion as previously described during the initial phase of the study.
There were no changes in patient care or office procedures before or after the implementation of this policy. Upon the scheduling of their surgery, each surgical patient is given preoperative and postoperative instructions that cover a range of frequently asked questions; from pain control and constipation to postoperative activity restrictions. This is not a deviation in our usual practice. There were no changes in preoperative counseling, instructions or hospital postoperative care. As such, the Institutional Review Board deemed this research to be a quality improvement project that met exemption criteria (HRP-216).
The primary outcome was the number of postoperative calls initiated by the patient within 6 weeks of their surgery. Secondary outcomes were the type of complaints reported and the number of patients who had called with a complaint.
The first month of the study served as a pilot study to estimate the frequency of calls pertaining to postoperative complaints. The pilot study determined a frequency of 20% of the patient-initiated calls pertaining to postoperative pain management. Therefore, the sample size calculation was based on the anticipated frequency of 18 ± 5% for a postoperative call about pain. To detect a 50% difference in the number of patient-initiated postoperative calls between the groups using a two-tailed confidence interval (CI) of 95% with a power of 0.8, a total of 227 patients were needed in each group. Continuous variables were represented as means with standard deviations and compared using Student’s t test. Ordinal data were reported as medians with a range and compared using the Mann–Whitney U test. Categorical variables were represented as proportions and calculated using Fisher’s exact test. Logistic regression was used to determine whether there were any associations with major versus minor surgeries or preoperative comorbidities with the number of calls a patient made in the postoperative period. All statistical analyses were performed using Minitab version 17.
Results
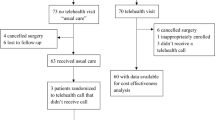
There were 226 patients in the control group, those who did not receive an FPC, and 233 patients in the intervention group for whom an FPC was intended.
Table 1 outlines the patient baseline characteristics, comorbidities, preoperative diagnosis, and surgeries performed. There were no significant differences in age or parity. There were no significant differences in preoperative diagnoses with the exception of post-hysterectomy vaginal vault prolapse. There were no significant differences in comorbidities with the exception of obesity. Similarly, there were no significant differences in surgeries between the two groups. The most common surgical procedure was a midurethral sling followed by robotic sacral colpopexy.
As to the primary outcome, there were significantly fewer patient-initiated calls made by the intervention group, with both groups having a median of 1 call per person, range 0–8 in the initial group and 0–10 in the FPC group (p = 0.04) over the 6-week postoperative period. Before implementing the policy, 325 calls were made by 103 patients, whereas in the intervention group 256 calls were made by significantly fewer patients, 82 (calls, p = 0.04, and the number of patients who called, p = 0.02; Table 2). This includes those patients who contacted our office before being called by the operating fellow, but does not include the calls made by the fellow.
Table 3 compares the frequency of postoperative complaints. The top five reasons for postoperative calls were as follows: pain, followed by questions concerning their medications, their disability paperwork, constipation, and laboratory/pathology results. After implementing the FPC intervention, we saw a significant decrease in calls concerning disability paperwork, constipation, incomplete bladder emptying, and vaginal bleeding. However, pain and medication management remained the leading complaints.
Patients who had a major surgery requiring an overnight stay, were 1.5 times (95% CI 1.2, 2.1) more likely to call with a postoperative complaint. As to comorbidities, a reverse logistic regression demonstrated that those with a history of fecal incontinence were twice as likely to call (95% CI 1.24, 3.23) than those without fecal incontinence. There were no other significant associations with the remaining comorbidities, including obesity.
The most frequently prescribed treatment as a result of the postoperative contact was reassurance and observation, 28.3 vs 27.9% (p > 0.999). However, there were significantly more office visits in the intervention group, 28.8 vs 18.6% (p = 0.014). There were no differences between groups for those who were treated for infection, pain, constipation or urinary retention (Table 4).
Discussion
In this study of postoperative complaints, we found that the implementation of the follow-up postoperative call (FPC) policy resulted in fewer patient-initiated postoperative calls. Furthermore, when examining the top 5 reasons why patients called within the defined postoperative period, we observed a statistically significant reduction in calls concerning constipation, vaginal bleeding, incomplete bladder emptying, and inquiries into disability paperwork, laboratory or pathology results. These reductions in calls may be considered a surrogate for a reduction in some of these common postoperative events. We also observed fewer calls, although not statistically significant, concerning pain, activity restrictions or medication management. We attribute these reductions to the follow-up calls, which are in addition to the extensive preoperative and postoperative counseling, with dispensed written educational materials [9, 10].
We did observe significantly more office visits as a result of the FPC. However, there were no differences in invasive treatments between the two groups. The FPC did not result in more adverse events, which is consistent with the 2006 Cochrane review of telephone follow-up initiated by hospital-based health professionals [8].
One of the limitations of this study is that the secondary outcomes are not adequately powered and we would caution the reader about interpreting these various results. Similarly, despite having a significant reduction in various postoperative complaints, we would not suggest using these results as a surrogate for a higher level of satisfaction. This would not be a reasonable conclusion without the supporting objective outcome measures. Furthermore, this was conducted as a before-and-after cohort study. Patients were not randomized to either group and potential biases may not be accounted for. Finally, the reported surgeries are performed within a fellowship training program and are elective. As such, these results may not be generalizable to other surgical practices, with or without trainees who routinely deal with emergency surgeries such as gynecological oncology or trauma surgery.
The main strength of the study is its prospective nature. Despite its before-and-after study design, this is a prospective study that was adequately powered for its primary outcome. In addition, this study minimized the potential for selection or recall biases. The before-and-after structure of this study included all surgical patients and the primary outcome was an objective dichotomous data point: “was a patient initiated call made?” Finally, this intervention has already had a positive impact on patient postoperative care in our practice. As a result, new practice policies in handling disability claims and return-to-work documentation have further improved postoperative care.
In this study of postoperative follow-up calls, we observed significantly fewer patient-initiated calls and a reduction in some of the most common postoperative complaints. With a significant decrease in postoperative complaints, there could potentially be an improvement in patient satisfaction. Future randomized control trials exploring patient satisfaction and other practice types would shed more light on this important issue.
References
Wu JM, Vaughn CP, Goode PS, et al. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstet Gynecol. 2014;123:141–7.
Turner LC, Kantartzis K, Lowder JL, Shepherd JP. The effect of age on complications in women undergoing minimally invasive sacral colpopexy. Int Urogynecol J. 2014;25(9):1251–6.
Unger CA, Walters MD, Ridgeway B, Jelovsek JE, Barber MD, MFR P. Incidence of adverse events after uterosacral colpopexy for uterovaginal and posthysterectomy vault prolapse. Am J Obstet Gynecol. 2015;212(5):603.e1–7.
Godden B. Postoperative phone calls: is there another way? J Perianesth Nurs. 2010;25(6):405–8.
Lushaj EB, Nelson K, Amond K, Kenny E, Badami A, Anagnostopoulos PV. Timely post-discharge telephone follow-up is a useful tool in identifying post-discharge complications patients after congenital heart surgery. Pediatr Cardiol. 2016;37(6):1106–10.
Flanagan J. Postoperative telephone calls: timing is everything. AORN J. 2009;90(1):41–51.
Young JM, Butow PN, Walsh J, et al. Multicenter randomized trial of centralized nurse-led telephone-based care coordination to improve outcomes after surgical resection for colorectal cancer: the CONNECT intervention. J Clin Oncol. 2013;31(28):3585–91.
Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev 2006(4):CD004510.
Dewar A, Scott J, Muir J. Telephone nursing follow-up for day surgery patients: patient perceptions and nurses’ experiences. J Perianesth Nurs. 2004;19(4):234–41.
Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–87.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Iwanoff, C., Giannopoulos, M. & Salamon, C. Follow-up postoperative calls to reduce common postoperative complaints among urogynecology patients. Int Urogynecol J 30, 1667–1672 (2019). https://doi.org/10.1007/s00192-018-3809-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3809-x