Abstract
Introduction and hypothesis
Levator ani muscle (LAM) and anal sphincter tears are common after vaginal birth and are associated with female pelvic organ prolapse and anal incontinence. The impact of subsequent births on LAM and external anal sphincter (EAS) integrity is less well defined. The objective of this study was to determine the prevalence of LAM and EAS trauma in primiparous (VP1) and multiparous (VP2+) women who had delivered vaginally to assess if there were differences between the two groups. The null hypothesis was: there is no significant difference in the prevalence of LAM and EAS trauma between the two groups.
Methods
This was a cross-sectional study involving 195 women, participants of the Dunedin arm of the ProLong study (PROlapse and incontinence LONG-term research study) seen 20 years after their index birth. Assessment included a standardized questionnaire, ICS POP-Q and 4D translabial ultrasound. Post-imaging analysis of LAM and EAS integrity was undertaken blinded against other data. Statistical analysis was performed using Fisher’s exact test and results were expressed as odds ratios (OR).
Results
LAM avulsion and EAS defects were diagnosed in 31 (16%) and 24 (12.4%) women respectively. No significant difference in the prevalence of levator avulsion and EAS defects between primiparous (VP1) and multiparous (VP2+) women who had delivered vaginally (OR 1.9, 95% CI 0.72–5.01, p = 0.26) and (OR 1.2, 95% CI 0.4–3.8, p = 0.76) respectively.
Conclusions
Most LAM avulsions and EAS defects seem to be caused by the first vaginal birth. Subsequent vaginal deliveries after the first were unlikely to cause further LAM trauma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In this era of increased women’s life expectancy, maternal birth trauma such as levator ani muscle (LAM) avulsion and obstetric anal sphincter injury (OASIS) is seen as increasingly relevant. This may be attributed to the association with long-term morbidity including pelvic organ prolapse (POP), pelvic floor and sexual dysfunction, fecal and/ or anal incontinence (AI), affecting women’s quality of life (QoL) and utilization of healthcare resources [1,2,3,4,5]. Pelvic organ prolapse affects 3–50% [6, 7] of the female population, involving a 10–20% lifetime risk of having prolapse surgery at a cost of over one billion USD annually (in the USA) [4, 5]. The long-term cost associated with AI secondary to OASIS was reported to be USD17,166 per patient in 1996 [8].
Levator trauma following vaginal delivery may be in the form of an avulsion (macrotrauma) and/ or irreversible overdistension (microtrauma). LAM avulsion, i.e., a traumatic detachment of the puborectalis muscle off its insertion on the inferior pubic rami [9, 10] is not an uncommon observation, with a reported incidence and prevalence of 14–36% [9,10,11]. Its association with POP and its recurrence after reconstructive surgery has been well documented [3, 12]. Levator trauma at vaginal birth has therefore been postulated as the “missing link” between vaginal childbirth and POP. Previous studies have suggested that the effect of vaginal birth on the hiatal biometry and pelvic organ support seemed to be associated mainly with the first birth [13, 14].
OASIS, with a reported incidence of 0.5–5.0% [15, 16] may result in fecal and/or anal incontinence in 9–39%, postpartum perineal pain, bladder and sexual dysfunction [17]. The recurrence rate with a repeat vaginal delivery is reported to range between 3.2 and 9.5% [18, 19].
Understanding disease etiology and behavior is crucial to developing preventive strategies. Although the effect of subsequent vaginal births on hiatal dimensions, pelvic organ support and anal sphincter function has been investigated [13, 14, 20], the impact on LAM and external anal sphincter (EAS) integrity is less well defined. The objective of this study was to determine the prevalence of LAM avulsion and EAS trauma in primiparous and multiparous women delivered vaginally approximately 20 years ago, with the null hypothesis being: there is no significant difference in the prevalence of levator and EAS trauma between vaginally primiparous and multiparous women.
Materials and methods
This was a cross-sectional study involving 195 women, participants of the Dunedin arm of the ProLong study (PROlapse and incontinence LONG-term research study) [21] seen in March–April 2014, for a 20-year review after their index birth in 1993/4. These women were identified in the parent study database of 1,228 women who delivered at Queen Mary Maternity Centre, Dunedin, New Zealand, between October 1993 and December 1994. Deceased women and those who declined further contact were excluded from the study (Fig. 1). Participants were sent patient-administered questionnaires (by post) which involved enquiries regarding symptoms of pelvic floor and sexual dysfunction, and details of subsequent pregnancies and deliveries after the index birth. Information on the index pregnancy and delivery were obtained from the hospital database.
Respondents were invited for a clinical assessment, which involved an examination for prolapse using the International Continence Society (ICS) Pelvic Organ Prolapse Quantification System (POP-Q) [22] and 4D translabial ultrasound (TLUS). TLUS was performed in the supine position, after voiding, using a GE Voluson E8 System (GE Medical Systems, Zipf, Austria), with an 8-4-MHz curved array volume transducer. Volumes were acquired at rest, on maximum pelvic floor muscle contraction (PFMC), and on Valsalva maneuver at an acquisition angle set to the system maximum of 85°, as previously described [23]. At least three volumes on Valsalva maneuver were acquired. TLUS was performed by a single operator, i.e., the first author, a urogynecologist who has performed and interpreted more than 1,000 TLUS. Clinical examination was performed before TLUS by the second author who is a gynecologist. Physical examination and TLUS were performed blinded against all clinical data. TLUS was performed blinded against the examination findings. Post-imaging analysis of LAM and EAS integrity was undertaken by the first author at a later date, using proprietary software, blinded against all other data.
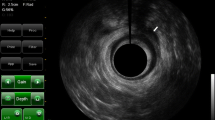
Avulsion of LAM was diagnosed on tomographic ultrasound imaging (TUI) on a volume acquired on PFMC, at a 2.5-mm inter-slice interval, from 5 mm below to 12.5 mm above the plane of minimal hiatal dimensions, encompassing the entire puborectalis muscle. The plane of minimal hiatal dimensions was identified in the midsagittal orthogonal plane where the distance between the hyperechogenic posterior aspect of the symphysis pubis and hyperechogenic anterior border of the LAM is shortest. LAM avulsion was diagnosed in the presence of discontinuity between the puborectalis muscle insertion and the pelvic sidewall in at least three central TUI slices (reference slice and the slices 2.5 to 5 mm cranially, i.e., slices 3–5 in Fig. 2a, b) as previously described and validated [24].
a Tomographic ultrasound imaging (TUI) of a normal pelvic floor and b a complete left-sided levator avulsion, marked with an asterisk, in slices 3–8. c TUI of an intact/normal EAS and d significant residual defect of the EAS involving 5 out of 6 slices, i.e., slices 2–6. Angled lines demonstrate defect location and size
Integrity of EAS was assessed utilizing TUI involving 8 slices, at an inter-slice interval tailored to individual sphincter length, encompassing the sphincter from the level of the puborectalis muscle to the subcutaneous part of the EAS, as previously described. “Significant defects of the EAS” were defined as the presence of a gap of at least 30° in its circumference, in at least 4 out of 6 slices on TUI (Fig. 2c, d) [25].
Statistical analysis was performed using SPSS 20 (SPSS, Chicago, IL, USA) and Minitab 16 (Minitab, State College, PA, USA). Categorical data were expressed as n (%) and compared using Fisher’s exact test and a p of <0.05 of was considered statistically significant. This study was approved by the New Zealand Health and Disability Ethics Committee (LRS/05/04/009/AM01).
Results
Of 1,228 women who delivered in Queen Mary Maternity Centre between October 1993 and December 1994, a total of 57 were excluded (deceased or declined further contact), leaving 1,171 to whom the questionnaires were sent. Questionnaire response rate was 39% (n = 453), of which 195 women consented and returned for clinical assessment (Fig. 1). Two were excluded as one declined the TLUS examination and another had missing data on parity, leaving 193 to whom these results pertain. They were seen on average 23 years (SD 3.6, range 19.4–46.2) after their first birth. Mean age was 50.1 (SD 5.1, range 36.9–62.8) years with a mean body mass index of 27.6 (SD 5.8, range 18.3–54.3) kg/m2. Median parity was 3 (IQR 2–3, range 1–14) with a mean age at first delivery of 27.1 (SD 4.8, range 16.3–38.3) years. One hundred and seventy-five (91%) were parous women who had delivered vaginally with a median parity of 2 (IQR 2–3, range 1–6). Eighteen (9.3%) were delivered exclusively by Cesarean section and 27 (15%) were primiparous women who had delivered vaginally. Fifty-seven (29.5%) and 12 (6%) gave a history of instrumental delivery and prolapse surgery respectively. One hundred and twenty-one (65%) and 80 (41%) complained of urinary incontinence and prolapse symptoms respectively. Forty (21%) had fecal incontinence.
On examination, 35% (n = 68) had significant POP (ICS stage > = 2 in the anterior and posterior compartment, and stage> = 1 centrally) [26]: in 23% (n = 45) this was a cystocele, in 12% (n = 23) uterine/vault descent, and in 20% (n = 39) a rectocele. Eleven percent (n = 22) had POP to the hymen and beyond. Mean Ba, C and Bp was −1.7 (SD 0.9, range − 3 to +1.5) cm, −5.4 (SD 1.5, range − 10 to +6.5) cm and −1.8 (SD 0.8, range − 3 to +1.5) cm respectively. Mean GH + Pb was 6.7 (SD 1.1, range 4.0–10.5) cm.
On imaging, levator avulsion was diagnosed in 30 (16%), being bilateral in 9 out of 193 (5%) and unilateral in 21 out of 193 (11%) with most being right sided (17 out of 21; 81%). Forty-seven percent (n = 91) had sonographically significant POP affecting the bladder in 21% (n = 41), the uterus in 36% (n = 64), the rectal ampulla in 26% (n = 51), and an enterocele in 1% (n = 2). On average, the bladder descended to 0.3 (SD 13.8, range − 47.5 to +24.6) mm above the symphysis pubis (SP). Mean uterine descent was to 19.7 (SD 17.9, −34.1 to +61.1) mm above the SP and mean descent of the rectal ampulla to 2.4 (SD 16.9, range −34.3 to 36.1) mm below the SP. Mean levator hiatal area on Valsalva was 22.8 (SD 7.6, range 8.2–48.0) cm2. Twenty-four (12.4%) had residual EAS defects on TUI. All such trauma was observed in parous women delivered vaginally except for one EAS defect seen after three Cesarean sections.
On univariate analysis, there was no significant difference in the prevalence of LAM avulsion and EAS defects between the primiparous (VP1) and multiparous (VP2+) women who delivered vaginally, P = 0.26 and 0.76 respectively (Table 1). On examining groups in more detail, there was no significant difference between parity groups delivered vaginally (VP1, VP2, VP3, and VP4+) with P = 0.08 and P = 0.72 for LAM avulsion and EAS defects respectively (Table 2). Clinical characteristics by parity groups delivered vaginally are presented in Table 3.
Discussion
Main findings
The overall prevalence of levator avulsion in our study was 16%, unilateral in 11%, and most of which were right-sided. This is comparable with a 13–14% population prevalence reported in earlier studies [9, 27]. However, it is lower than the 19% prevalence reported in a Norwegian study with a similar population [28]. This may be explained by the large proportion of women with a history of forceps-assisted first delivery (26.2%) in the latter study [28], as a result of the selection criteria of its parent study [29]. In our study, the rate of forceps delivery in the first or index delivery was lower at 23%. Forceps delivery is strongly associated with LAM avulsion. Similar to previous studies, we found a right-sided preponderance of LAM avulsion [9, 11, 30]. The cause of a higher prevalence of right-sided trauma is unclear. We also found a 12.4% prevalence of sonographically diagnosed EAS defects, which is comparable with earlier studies that reported a 12–13% prevalence in a primiparous cohort [27, 31]. Most reported data in the current literature on EAS defects involved either symptomatic cohorts or women with repaired OASIS. The limited data on asymptomatic cohorts in the long term following childbirth call for further studies.
The main finding of this study is that there is no difference in the prevalence of LAM avulsion and EAS defects between the primiparous and multiparous or among the different parity groups delivered vaginally. This suggests that it might be the first vaginal delivery that is most likely to cause such trauma, which is in support of previous studies on LAM avulsion and function, levator hiatal biometry and pelvic organ support [14]. Horak et al., in their study of women after a second birth, reported that a second pregnancy and delivery do not seem to have a major effect on bladder support and/or levator function. Apart from one LAM avulsion following a vaginal birth after cesarean (VBAC), no new cases of avulsion were diagnosed after a second birth [14]. Our findings are also in agreement with another study that reported that most of the effect of vaginal childbirth on hiatal dimensions seemed to be associated with the first vaginal delivery, with subsequent vaginal birth not having major additional effects [13].
Avulsion of the LAM has been shown to be an independent predictor of POP and its recurrence after a reconstructive surgery [3, 9, 12]. Likewise, EAS trauma is associated with anal incontinence [17]. These injuries may also result in other forms of chronic morbidity, such as perineal pain, dyspareunia, and sexual dysfunction, impairing women’s quality of life (QoL) and often involving long latency between trauma and subsequent morbidity [1, 2, 17]. To this date, attempts at repairing LAM avulsion have had limited success [32]. Understanding disease pattern and pathophysiology is important for the development of preventative strategies. From this current study, it appears probably that the first delivery is by far the most likely to cause trauma; thus, any form of prevention should focus on the first delivery. This includes avoiding forceps delivery. A prolonged second stage of labor and advanced maternal age at first delivery are also established risk factors for such injuries [32]. Antenatal use of a birth trainer to reduce intrapartum pelvic floor trauma has been shown to be of unlikely clinical benefit [27].
Mesh use in pelvic floor reconstructive surgery has been a debatable issue in recent years owing to mesh-related complications, mainly chronic pain and dyspareunia. However, mesh-augmented POP repair in women with LAM avulsion has been shown to reduce the likelihood or recurrence [33]. Pelvic floor imaging plays a major role in diagnosing these injuries and quantification of functional impairment. Diagnosis of LAM avulsion should be a routine part of pre-operative assessment for POP surgery; thus, the option of a mesh-augmented surgery can be offered to women with LAM avulsion.
Other findings
It is intriguing that there was a trend toward lower avulsion rates in multiparas. This may be due to a negative effect of traumatic childbirth on reproductive behavior, explained either by conscious decisions affecting reproduction, or by post-traumatic stress disorder (PTSD), dyspareunia and/or infrequent intercourse [1, 2, 34]. The difference in delivery mode for the first baby as shown in Table 3 seems to support this conclusion: women with only one vaginal birth were much less likely to have had a normal vaginal delivery rather than if they had had a forceps delivery or Cesarean section with their first birth.
Another unexpected finding was a significant EAS defect in a woman who had had only Cesarean deliveries. She was delivered exclusively via three Cesarean sections (CS): one first-stage CS for poor progress, followed by two elective CS. A possible explanation could be a concealed previous vaginal delivery, although POPQ findings were consistent with her having had only Cesarean deliveries. Non-obstetric causes of anal sphincter disruption are uncommon and include open pelvic perineal trauma, traumatic anal coitus, and some form of anorectal surgery such as sphincterotomy or hemorrhoidectomy. However, injuries from anorectal surgery rarely involve the ventral aspect of the EAS [35]. Hence, we have to conclude that we have no explanation for this particular finding.
Strengths and limitations
The strength of this study lies in the design and long follow-up interval. To our knowledge, this is the first study looking at a general population, i.e., a cohort, at least 20 years after their first childbirth. Most studies in the literature involve symptomatic patients or report on much shorter follow-up intervals. We utilized the ultrasound diagnosis of LAM and EAS trauma, a more objective and repeatable form of assessment. Although these traumata may be diagnosed clinically, they are commonly either occult or missed on clinical examination [25]. An unbiased and comprehensive detection of maternal birth trauma requires postnatal imaging.
Our study is not without limitations. Our research question would ideally be addressed by longitudinally assessing women prospectively for LAM and EAS integrity after each birth. However, such a research design would be logistically difficult as a larger sample size and extended follow-up would be required. The relatively high prevalence of women with symptoms of pelvic floor dysfunction (65% urinary incontinence and 41% POP symptoms) in addition to clinically (35%) and sonographically (47%) significant POP in our study may reflect that most respondents who agreed to the clinical assessment chose to be examined because they were symptomatic. This may result in a degree of selection bias, which needs to be acknowledged as a limitation. Another limitation is the fact that our study population was mainly Caucasian. Our result may not be applicable to other ethnic backgrounds.
Conclusions
Most LAM avulsions and EAS defects seem to be caused by the first vaginal birth. Subsequent vaginal deliveries seem unlikely to cause further LAM trauma.
References
Signorello LB, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: a retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184(5):881–90.
Thompson JF, Roberts CL, Currie M, Ellwood DA. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002;29(2):83–94.
Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. Br J Obstet Gynaecol. 2008;115:979–84.
Smith FJ, Holman CDAJ, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100.
Subak LL, Waetjen LE, Van Den ES, Thorm ES, et al. Cost of pelvic organ surgery in the United States. Obstet Gynecol. 2001;98:646–51.
Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL. Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol. 2007;109(6):1396–403.
Gyhagen M, Bullarbo M, Nielsen T, Milsom I. Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. Br J Obstet Gynaecol. 2013;120(2):152–60.
Mellgren A, Jensen LL, Zetterström JP, Wong WD, Hofmeister JH, Lowry AC. Long-term cost of fecal incontinence secondary to obstetric injuries. Dis Colon Rectum. 1999;42(7):857–65.
Shek KL, Dietz HP. Can levator avulsion be predicted antenatally? Am J Obstet Gynecol. 2010;202(6):586.e1–6.
Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106:707–12.
Dietz HP, Steensma AB. The prevalence of major abnormalities of the levator ani in urogynaecological patients. Br J Obstet Gynaecol. 2006;113(2):225–30.
Model AN, Shek KL, Dietz HP. Levator defects are associated with prolapse after pelvic floor surgery. Eur J Obstet Gynecol Reprod Biol. 2010;153(2):220–3.
Kamisan Atan I, Gerges B, Shek K, Dietz H. The association between vaginal parity and hiatal dimensions: a retrospective observational study in a tertiary urogynaecological centre. Br J Obstet Gynaecol. 2015;122(6):867–72.
Horak TA, Guzman-Rojas R, Shek KLL, Dietz HP. Pelvic floor trauma: does the second baby matter? Ultrasound Obstet Gynecol. 2014;44(1):90–4.
Rojas RG, Atan IK, Shek KL, Dietz HP. The prevalence of abnormal posterior compartment anatomy and its association with obstructed defecation symptoms in urogynecological patients. Int Urogynecol J. 2016;27:(6):939–944.
Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries—myth or reality? Br J Obstet Gynaecol. 2006;113(2):195–200.
Marsh F, Lynne R, Christine L, Alison W. Obstetric anal sphincter injury in the UK and its effect on bowel, bladder and sexual function. Eur J Obstet Gynaecol Reprod Biol. 2011;154(2):223–7.
Baghestan E, Irgens L, Børdahl P, Rasmussen S. Risk of recurrence and subsequent delivery after obstetric anal sphincter injuries. Br J Obstet Gynaecol. 2012;119(1):62–9.
Basham E, Stock L, Lewicky-Gaupp C, Mitchell C, Gossett DR. Subsequent pregnancy outcomes after obstetric anal sphincter injuries (OASIS). Female Pelvic Med Reconstr Surg. 2013;19(6):328–32.
Jangö H, Langhoff-Roos J, Rosthøj S, Sakse A. Mode of delivery after obstetric anal sphincter injury and the risk of long-term anal incontinence. Am J Obstet Gynecol. 2016;214(6):733.e1–e13.
Glazener C, Elders A, Macarthur C, Lancashire R, Herbison P, Hagen S, et al. Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. Br J Obstet Gynaecol. 2013;120(2):161–8.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Dietz HP. Ultrasound imaging of the pelvic floor. II. Three-dimensional or volume imaging. Ultrasound Obstet Gynecol. 2004;23(6):615–25.
Dietz H, Shek K. Tomographic ultrasound imaging of the pelvic floor: which levels matter most? Ultrasound Obstet Gynecol. 2009;33(6):698–703.
Guzman Rojas R, Shek K, Langer S, Dietz H. Prevalence of anal sphincter injury in primiparous women. Ultrasound Obstet Gynecol. 2013;42(4):461–6.
Dietz HP, Mann KP. What is clinically relevant prolapse? An attempt at defining cutoffs for the clinical assessment of pelvic organ descent. Int Urogynecol J. 2014;25(4):451–5.
Kamisan Atan I, Shek K, Langer S, Guzman Rojas R, Caudwell-Hall J, Daly J, et al. Does the Epi-No® birth trainer prevent vaginal birth-related pelvic floor trauma? A multicentre prospective randomised controlled trial. Br J Obstet Gynaecol. 2016;123:995–1003.
Volløyhaug I, Mørkved S, Salvesen KÅ. Association between pelvic floor muscle trauma and pelvic organ prolapse 20 years after delivery. Int Urogynecol J. 2016;27(1):39–45.
Volløyhaug I, Mørkved S, Salvesen Ø, Salvesen K. Pelvic organ prolapse and incontinence 15–23 years after first delivery: a cross-sectional study. Br J Obstet Gynaecol. 2015;122(7):964–71.
Gainey HL. Post-partum observation of pelvic tissue damage. Am J Obstet Gynecol. 1943;46:457–66.
Corton MM, McIntire DD, Twickler DM, Atnip S, Schaffer JI, Leveno KJ. Endoanal ultrasound for detection of sphincter defects following childbirth. Int Urogynecol J. 2013;24(4):627–35.
Dietz HP. Pelvic floor trauma in childbirth. Aust N Z J Obstet Gynecol. 2013;53(3):220–30.
Rodrigo N, Wong V, Shek KL, Martin A, Dietz HP. The use of 3-dimensional ultrasound of the pelvic floor to predict recurrence risk after pelvic reconstructive surgery. Aust N Z J Obstet Gynecol. 2014;54(3):206–11.
Skinner EM, Dietz HP. Psychological and somatic sequelae of traumatic vaginal delivery: a literature review. Aust N Z J Obstet Gynecol. 2015;55(4):309–14.
Brill SA, Margolin DA. Anal sphincter trauma. Semin Colon Rectal Surg. 2004;15(2):90–4.
Acknowledgements
The authors would like to thank the women who participated in this study, and Gaye Ellis, the Research Coordinator in Women’s and Children’s Health, Department of Obstetrics & Gynecology, Dunedin School of Medicine & Health Sciences, University of Otago, for her involvement in the follow-up administration. We also acknowledge the loaned ultrasound equipment from GE Medical for this study.
Funding
This study was funded by The University of Otago Research Grant, without having any influence or conflicts of interest in the results of the study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Details of ethics approval
This study was approved by the New Zealand Health and Disability Ethics Committee (LRS/05/04/009/AM01).
Conflicts of interest
HP Dietz has received honoraria from GE Medical. None of the other authors has any conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Kamisan Atan, I., Lin, S., Dietz, H.P. et al. It is the first birth that does the damage: a cross-sectional study 20 years after delivery. Int Urogynecol J 29, 1637–1643 (2018). https://doi.org/10.1007/s00192-018-3616-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3616-4