Abstract
Introduction and hypothesis
Pregnant women benefit from completing pelvic floor muscle exercises (PFMEs). The aims of the study were to evaluate pregnant women’s levels of awareness, knowledge, and beliefs about the pelvic floor muscles (PFMs) and PFMEs.
Methods
A cross-sectional survey was conducted. Respondents were pregnant women over the age of 18 years who attended antenatal clinics in Western Australia (WA). Questionnaire items measured awareness and knowledge about PFMs, confidence and beliefs about engaging in PFMEs, and attendance at antenatal education (ANE) classes. Chi-squared tests examined potential associations between questionnaire items and respondent characteristics.
Results
Mean gestation of respondents (n = 633 out of 850; 74% response rate) was 28.7 (+7.8) weeks and 50% were giving birth for the first time. Although 76% of respondents knew that PFMs can prevent urinary incontinence, only 27% knew that they prevented faecal incontinence and 41% thought it was normal to leak urine when pregnant. Only n = 72 (11%) were practicing PFMEs. Respondents who had attended ANE (28%) were significantly more knowledgeable about pelvic floor function (p < .001) and significantly less likely to believe that leaking urine during pregnancy was normal (p = 0.02), compared with those who had not attended ANE. Respondents who did not speak English at home (18%) were significantly less knowledgeable about PFMs and PFMEs, and significantly less likely to have attended, or planned to attend, ANE classes.
Conclusion
Pregnant women require more health education regarding PFMs. Education should be provided using diverse modes, especially for women from migrant backgrounds and women who do not plan to attend formal ANE classes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence (UI) is one of the most common and embarrassing problems encountered during pregnancy [1–3] and is known to have a serious negative impact on quality of life, with adverse social, physical and psychological consequences [4]. It is important to identify and treat this problem, as pregnancy and birth are major risk factors for developing UI [4, 5]. There is strong evidence that providing education and training for pelvic floor muscle exercises (PFMEs) during the antenatal period is a means of reducing and preventing UI in the postnatal period, in either women who are dry or those who already have UI [6, 7].
However, health behaviour change theory demonstrates that individuals need to be sufficiently capable (both aware of the potential health problem and knowledgeable about how to engage in the desired health behaviour of PFMEs) and motivated to engage in preventive health behaviours such as PFMEs [8, 9]. They also require the social (both physical and psychological) opportunity to engage in PFMEs and any barriers or enablers to the desired behaviours should be addressed [8, 10]. There have been limited studies in antenatal populations that have assessed knowledge and awareness about the structure and function of the PFMs, particularly its role in preventing UI and levels of motivation to engage in PFMEs [1, 11–13]. A recent survey of 212 nulliparous women, assessing levels of knowledge about the structure and function of the pelvic floor, found that 81% of respondents had never received information about the pelvic floor and only 3% had completed any training in PFMEs [12]. Another study that surveyed women about their knowledge of pelvic floor problems found an average knowledge score of 44 out of 100, and even lower knowledge scores about faecal incontinence and prolapse [11]. However, these studies included a total of only 682 pregnant women, only one study surveyed both primiparous and multiparous women [1], only one study asked women about the structure of the pelvic floor [12], and none of the studies was conducted in Australia.
Pregnant women may gain knowledge about PFMEs through health professionals providing ANE [1, 2]. However, not all women seek or receive such education [1, 12]. Therefore, there may be differences in knowledge according to if women attend ANE and women who do not attend may also lack motivation or the social opportunity to engage in PFMs [8–10]. If women do not gain this awareness and knowledge about PFMs and PFMEs through ANE or other information sources, they might not engage in PFMEs either in the ante- or the postpartum period, or be aware that they should seek help for any onset of UI or other pelvic floor problems.
The aims of the study were to evaluate Australian pregnant women’s levels of awareness, knowledge and beliefs about PFMs and PFMEs. Women were also surveyed about their self-reported engagement in PFMEs and their planned attendance at ANE classes.
Materials and methods
Design
A cross-sectional survey of pregnant women was undertaken.
Ethical considerations
The study was approved by the University of Notre Dame Australia human research ethics committee and the Department of Health of Western Australia (DoHWA), north and south metropolitan, and country health service ethics committees. All respondents provided written, informed consent before completing the survey.
Participants and setting
The survey was conducted in WA, where DoHWA reports data regarding births in WA [14]. DoHWA at the time of the survey was divided into a single rural, and two (north and south) metropolitan health regions. Recruitment was undertaken in a face-to-face setting at DoHWA maternal health clinics and postal surveys were sent through a number of other clinics with the aim of broadening the sample.
Participants were eligible for inclusion in the study if they were pregnant, aged over 18 years, able to speak and read English, able to provide written informed consent, and had not previously completed the survey. The exclusion criterion was a diagnosis of any neurological condition, including multiple sclerosis or stroke.
Data collection instrument
Data were collected using a custom-designed questionnaire, which used a mix of categorical and Likert type scales. Questionnaire items measured awareness of PFMs and knowledge of PFMs and PFMEs. Items also measured beliefs about UI as a key function of PFMs is to prevent UI, beliefs about PFMEs’ role in preventing UI, and whether respondents believed that they could engage in PFMEs. Self-reported engagement in PFMEs was also measured. Other items measured age, level of education, country of birth and language spoken at home (English or a language other than English [LOTE]), parity, gestation, body mass index (BMI), self-reported frequency of UI, and attendance at ANE classes held in WA. Socio-economic status was measured using the Socio-Economic Indexes for Areas (SEIFA), developed by the Australian Bureau of Statistics [15]. The SEIFA provides a composite measure to rank areas in Australia according to relative socio-economic advantage and disadvantage. The measures are based on information from the 5-yearly Australian census.
The questionnaire items were designed by a women’s health physiotherapist (JW) and were based on seeking to understand pregnant women’s knowledge about the structure and function of PFMs and PFMEs. The initial questionnaire was sent to three physiotherapists specialising in women’s health, who were asked to answer and appraise the questions [16, 17]. The questionnaire was also assessed for content validity by a group of pregnant women attending an ANE class. The questionnaires were then modified and piloted [16] in 10 pregnant women to ensure that any ambiguities and sensitivities had been excluded, and to identify how long the questionnaire took to answer. Feedback from these sources was analysed by the researchers and the wording in some items was altered to allow for a clearer understanding of the item. The revised questionnaire was then re-piloted with another group of 10 pregnant women attending an ANE class [17].
Procedure
All pregnant women attending the clinics were approached in consecutive order by the researcher, advised of the purpose of the research, and women over 18 years of age were invited to participate and provide written informed consent. Women who were unable to complete the survey at the time, but who consented to provide their email address and telephone number, were subsequently contacted and invited to complete the questionnaire, using an internet-based survey platform [18]. Copies of the survey were posted to clinics who indicated a willingness to distribute the surveys.
Statistical analysis
Data were summarised using descriptive statistics (frequency and means [SD] or medians [IQR]). The representativeness of the sample was inspected by comparing demographic data from the sample with the DoHWA data [14], using Chi-squared tests. Analyses were undertaken to examine differences in knowledge, awareness about PFMs and PFMEs between the demographic groups of respondents based upon those characteristics that were thought to be likely to affect knowledge, awareness and beliefs about PFMs and PFMEs. Therefore, differences between those who spoke LOTE and English speakers, between primiparous and multiparous women, and between those who had attended and those who had not attended ANE were compared using the cross-tabulations of Chi-squared or, where required, Fisher’s exact tests. All data were analysed using Stata 14 (Stata Statistical Software: Release 14; StataCorp, College Station, TX, USA).
Sample size
A minimum required sample size was estimated using previously reported DoHWA data, which indicated that there were 31,734 babies delivered in WA in 2011 [14]. It was estimated that a minimum sample of 380 was required [19] to determine using a 95% confidence interval the proportion of pregnant women (within a 5% margin of error) with a positive response to a question (e.g. the proportion of pregnant women aware that PFMEs can prevent UI).
Results
Survey response
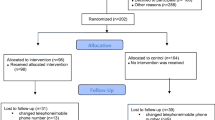
A total of 850 questionnaires were circulated, of which 633 (74.5%) were completed and returned (Fig. 1). Some respondents did not answer all questions, meaning that there were missing data for some items (Tables 1, 2, 3, and 4). Women from the northern region were proportionally more represented in the sample compared with the DoHWA data and significantly more respondents were from higher socio-economic backgrounds. More than 95% of respondents were planning to give birth in a DoHWA (public) hospital, whereas DoHWA data indicated that 40% of women in WA gave birth in private hospitals in 2011 [14].
Demographic and clinical characteristics of respondents
Demographic and clinical characteristics of respondents are presented in Table 1. Respondents mean age was 29.2 years and the mean gestation period of the cohort was 28.7 weeks. Of note, 310 respondents (49.0%) reported that they experienced UI. Respondents who were multiparous were significantly more likely to report UI (62.6%) than those who were primiparous (44.2%; p < 0.001). Respondents without asthma (or other condition causing chronic cough; n = 571) were significantly more likely to be continent (n = 274 [48.0%]) than those respondents with asthma (n = 62, continent, n = 19 [30.6%]; p = 0.008). Respondents with an increased BMI (n = 200) had an increased frequency of self-reported UI (55%) compared with those who were of normal weight who reported UI (50%), although these differences were not significant (p = 0.246).
Awareness of PFMs and engagement in PFMEs
Questionnaire responses that measured respondents’ awareness of PFMs and PFMEs and how respondents obtained information about PFMs are presented in Table 2. One hundred and eight respondents (17.4%) had not heard of, or were unsure if they had ever heard of, PFMs. Respondents who spoke LOTE, whether primiparous or multiparous, were significantly more likely to report that they had not heard about PFMs. Three hundred and six respondents (49.4%) reported that they heard about PFMs from a midwife. Seventy respondents (11.0%) reported that they were currently practicing PFMEs. Respondents who reported UI were not significantly more likely to be practicing PFMEs than those who did not report UI (p = 0.316).
There was no significant difference in engagement in PFMEs between respondents who were planning to attend ANE (practicing PFMEs, n = 29 [40.3%], not practicing PFMEs, n = 199 [35.5%], p = 0.44). However, respondents who were not planning to attend ANE were less likely to be practicing PFMEs (practicing PFMEs, n = 9 [12.5%], not practicing PFMEs, n = 179 [32.0%], p < 0.001). Respondents who had attended ANE during their present or previous pregnancy were significantly more likely to be practicing PFMEs (practicing PFMEs, n = 32 [44.5%], not practicing PFMEs, n = 146 [26.0%], p = 0.02).
Levels of knowledge about PFMs and PFMEs
Respondents’ levels of knowledge about the anatomy and function of PFMs and PFMEs are presented in Table 3. Four hundred and eighty-one respondents (76%) correctly identified that PFMs function to prevent UI, but only (27.3%) knew that the PFMs also function to prevent faecal incontinence and 131 respondents (20.7%) could not identify any PFM function. Only 34 (5.4%) respondents correctly answered the question “what do your PFMs go around?”
Beliefs about PFM function, UI and PFMEs
Respondents’ confidence in and beliefs about PFMs in pregnancy, in particular UI and engaging in PFMEs, are presented in Fig. 2. Two hundred and sixty-two respondents (41.4%) strongly agreed or agreed that it was normal to leak urine when pregnant. One hundred and eighty respondents (28.2%) were undecided as to whether there was treatment for UI during pregnancy. Respondents who had not attended ANE in the present or previous pregnancy were significantly more likely to strongly agree or agree that it was normal to leak urine than those women who had already attended ANE (not attended, n = 196, attended ANE, n = 66 [p = 0.02]).
Attendance at ANE
Around a third of respondents (36.2%) reported that they planned to attend ANE, whereas 29.7% did not plan to attend ANE (Table 1). Table 4 shows parity, the language spoken at home and attendance at ANE. Of the 178 respondents who had attended ANE either during their present or previous pregnancy, respondents who spoke LOTE were significantly less likely to have attended than those who spoke English (p = <.001). Of the 188 participants who were not planning to attend ANE those who spoke LOTE were significantly less likely to be planning to attend ANE than those participants who spoke English (p = 0.008).
Respondents from the most disadvantaged socioeconomic areas were significantly more likely not to be planning to attend ANE (n = 30 [44.8%]) than those from more advantaged (n =87 [32.4%]) or the most advantaged areas (n = 55 [23.9%]; p = 0.002). Regarding education, respondents with education beyond school (college or university education) were significantly more likely be planning to attend ANE (n = 138 [60.3%]) compared with respondents who had school education only (n = 91 [39.7%]; p < 0.001).
Discussion
This Australian survey provided new findings regarding pregnant women’s levels of knowledge of PFMs and PFMEs. Although 76% of respondents knew that PFMs play a role in preventing UI, only 27% of respondents knew that PFMs prevent or reduce faecal incontinence. Respondents also had very limited knowledge about the anatomy of the PFMs: for example, only 54% knew that PFMs went around the bladder opening and approximately 20% of women responded that they did not know what the PFMs do. This concurred with a previous study of primiparous women, which found that only 43% of women could name more than one function of the pelvic floor [12].
In this survey, almost 50% of respondents reported that they had experienced UI, similar to findings of other large studies in this population [1, 20]. This frequency could reflect that the mean gestation period of the respondents was just over the end of the second trimester. It was thus of concern that over 40% of respondents believed that it was normal to leak urine during pregnancy and over 32% of respondents were undecided or disagreed that treatment for UI is available during pregnancy. Approximately one third of women previously surveyed in Belgium also thought it was normal to leak urine or need to use a pad for incontinence [12]. Low levels of awareness and erroneous beliefs about PFMs and PFMEs, i.e. how they function to prevent UI, when viewed within the concepts of health behaviour change, suggest that pregnant women might not be sufficiently capable or motivated to seek help for UI during the antenatal period, or to initiate or consistently engage in PFMEs [8, 10].
Only 11% of respondents were practicing PFMEs and a further 30% had never or were unsure about whether they had ever exercised their PFMs, which concurs with findings from another survey reporting that only 3% of pregnant women were practicing PFMEs [12]. This differs from a survey in Scotland, which found that approximately 54% of women were practicing PFMEs [1]. However, this sample had a longer mean gestation period than ours, of 28 weeks, and almost 40% had received the information in a parent education class, whereas in our study only 28% of women had attended ANE classes. Concepts of health behaviour change applied would suggest that having awareness about PFMs alone does not mean that women are capable (including skills) of engaging in PMFEs [8]. Additionally, motivation and social opportunity (such as attending ANE) are also key factors in stimulating health behaviour change [8]. However, over 80% of respondents believed that they would do PFMEs if advised, suggesting good levels of motivation. Therefore, health professionals should ensure that all pregnant women receive training and ongoing monitoring about how to undertake PFMEs, a recommendation supported by other studies [1, 12]. In our study, only 50% of women had received information about PFMs from the midwife, even though 50% had already reported some UI.
Like the study conducted in Scotland [1], there was a significant increase in the likelihood of respondents who practiced PFMEs having attended ANE compared with respondents who were not practicing PFMEs, suggesting that social opportunity and the knowledge and motivation gained from attending ANE might be valuable. However, although respondents in this study who had attended ANE had the highest knowledge in correctly responding that PFMEs should be practiced daily, there were still low levels of engagement in PFMEs among this group. A previous study conducted in WA found that although all physiotherapists delivered education about engaging in PFMEs at ANE classes, their class contact time was very limited, with less than half of women who attended a publicly held ANE class in WA likely to have physiotherapist input [21]. Other studies suggest that effective instruction and training from a health professional might be an important means of building the skills and confidence to practice PFMEs [22, 23].
Women from higher socioeconomic groups were over-represented in our sample compared with the WA population, and these women were significantly more likely to be planning to attend ANE, meaning that in broad antenatal populations drawn from all socioeconomic groups, even fewer pregnant women may plan to attend ANE. Importantly, those respondents who spoke LOTE were significantly less likely to be aware of PFMs and also significantly less likely to be planning to attend, or to have already attended, ANE. Therefore, pregnant women from migrant backgrounds who are not planning to attend ANE may be more at risk of developing PFM dysfunction, including the resulting UI. Women who are migrants to Australia, particularly those who are primiparous, may need more tailored and culturally appropriate services in the antenatal period, aimed at avoiding postnatal pelvic floor problems.
It was not practical to obtain a list of all pregnant women in WA and generate a completely representative sample; however, 7 DoHWA sites were approached using face-to-face surveys. Mail-outs were delivered to 6 sites and data were collected from 25 sites. The sample characteristics differed in some respects, such as socioeconomic status, from the DoHWA, but the sample was still largely representative of pregnant women in WA, being similar in proportions for characteristics such as parity and medical conditions. Eighteen percent of respondents spoke LOTE at home, which is in accordance with the 2011 Australian census [24]. These data, though specific to WA, may be useful in informing services for pregnant women in other, similar health systems. There were some missing data for nearly all questionnaire items and those women who spoke LOTE were more likely to leave items unanswered, possibly because of the language difficulty. Future questionnaires should be administered in other languages to gain information about these women’s knowledge of PFMs and PFMEs, and additionally to seek their feedback about how they would like ANE to be provided.
Conclusion
Pregnant women surveyed in Australia had limited knowledge and awareness about PFMs, in particular if they were primiparous or came from a culturally diverse background. Not all women planned to attend ANE and those who did not speak English as a first language were significantly less likely to attend ANE. Therefore, more research is needed to establish broad methods of providing ANE for pregnant women that effectively increase their knowledge and awareness of PFMs, and assist them to develop the capability, motivation and social opportunity to engage in PFMEs.
References
Whitford HM, Alder B, Jones M. A cross-sectional study of knowledge and practice of pelvic floor exercises during pregnancy and associated symptoms of stress urinary incontinence in North-East Scotland. Midwifery. 2007;23:204–17. doi:10.1016/j.midw.2006.06.006.
Sangsawang B, Sangsawang N. Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment. Int Urogynecol J. 2013;24:901–12. doi:10.1007/s00192-013-2061-7.
Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900–7. doi:10.1056/NEJMoa021788.
Lasserre A, Pelat C, Gueroult V, Hanslik T, Chartier-Kastler E, Blanchon T, et al. Urinary incontinence in French women: prevalence, risk factors, and impact on quality of life. Eur Urol. 2009;56:177–83. doi:10.1016/j.eururo.2009.04.006.
Memon H, Handa VL. Pelvic floor disorders following vaginal or cesarean delivery. Curr Opin Obstet Gynecol. 2012;24:349–54. doi:10.1097/GCO.0b013e328357628b.
Boyle R, Hay-Smith EJ, Cody JD, Morkved S. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2012;10, Cd007471. doi:10.1002/14651858.CD007471.pub2.
Bo K, Hilde G. Does it work in the long term?—A systematic review on pelvic floor muscle training for female stress urinary incontinence. Neurourol Urodyn. 2013;32:215–23. doi:10.1002/nau.22292.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi:10.1186/1748-5908-6-42.
Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27:379–87. doi:10.1037/0278-6133.27.3.379.
Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. doi:10.1186/1748-5908-7-37.
O’Neill AT, Hockey J, O’Brien P, Williams A, Morris TP, Khan T, et al. Knowledge of pelvic floor problems: a study of third trimester, primiparous women. Int Urogynecol J. 2017;28:125–9. doi:10.1007/s00192-016-3087-4.
Neels H, Wyndaele JJ, Tjalma WA, De Wachter S, Wyndaele M, Vermandel A. Knowledge of the pelvic floor in nulliparous women. J Phys Ther Sci. 2016;28:1524–33. doi:10.1589/jpts.28.1524.
Moossdorff-Steinhauser HF, Albers-Heitner P, Weemhoff M, Spaanderman ME, Nieman FH, Berghmans B. Factors influencing postpartum women’s willingness to participate in a preventive pelvic floor muscle training program: a web-based survey. Eur J Obstet Gynecol Reprod Biol. 2015;195:182–7. doi:10.1016/j.ejogrb.2015.10.009.
Hutchinson M, Joyce A. Western Australia’s mothers and babies, 2011: twenty-ninth annual report of the Western Australian midwives’ notification. Department of Health WA: Western Australia; 2014.
Australian Bureau of Statistics. Socio-Economic Indexes for Areas (SEIFA), 2011 Canberra: Commonwealth of Australia; 2013. http://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa. Accessed 19 December 2016.
Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. Philadephia: Davis; 2015.
Peat J, Williams K, Wei X, Mellis C. Health science research: a handbook of quantitative methods. London: Sage; 2002.
SurveyMonkey Inc. Palo Alto, California, USA. 2016. www.surveymonkey.com. Accessed 19 December 2016.
Creative research systems Sebastopol CA 2016. http://www.surveysystem.com/sscalc.htm. Accessed 19 December 2016.
Sangsawang B. Risk factors for the development of stress urinary incontinence during pregnancy in primigravidae: a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2014;178:27–34. doi:10.1016/j.ejogrb.2014.04.010.
Wilson J, Berlach RG, Hill A-M. An audit of antenatal education facilitated by physiotherapists in Western Australian public hospitals. Aust N Z Continence J. 2014;20(2):44–6.
Whitford HM, Jones M. An exploration of the motivation of pregnant women to perform pelvic floor exercises using the revised theory of planned behaviour. Br J Health Psychol. 2011;16:761–78. doi:10.1111/j.2044-8287.2010.02013.x.
Ghaderi F, Oskouei AE. Physiotherapy for women with stress urinary incontinence: a review article. J Phys Ther Sci. 2014;26:1493–9. doi:10.1589/jpts.26.1493.
Australian Bureau of Statistics. 2012. http://www.abs.gov.au/websitedbs/censushome.nsf/home/CO-60. Accessed 19 December 2016.
Acknowledgements
Authors thank all pregnant women in WA who responded to the survey and the women’s health physiotherapists who gave input and feedback to the survey design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Nil.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Hill, AM., McPhail, S.M., Wilson, J.M. et al. Pregnant women’s awareness, knowledge and beliefs about pelvic floor muscles: a cross-sectional survey. Int Urogynecol J 28, 1557–1565 (2017). https://doi.org/10.1007/s00192-017-3309-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3309-4