Abstract
Introduction and hypothesis
The purpose of our study was to describe the surgical trends for female stress urinary incontinence (SUI) during 2006–2010, and a time-frame comparison with 1997–2005, based upon the National Health Insurance (NHI) claims data in Taiwan.
Methods
Women who underwent various primary surgeries for SUI during 2006–2010 were identified, with a total of 15,099 inpatients. The variables included surgical types, patient age, surgeon age and gender, specialty, and hospital accreditation levels. Chi-squared tests and SAS version 9.3.1 were used for statistical analysis.
Results
During the follow-up study, midurethral sling (MUS) application increased significantly from 53.09 % in 2006 to 78.74 % in 2010. It was associated concomitantly with a decrease in retropubic urethropexy (RPU) from 29.68 % to 12.99 %, and pubovaginal sling treatment (PVS) from 9.33 % to 3.46 %. MUS was most commonly used among all patients’ and surgeons’ age groups, and different accreditation hospital levels. MUS was more commonly used by gynecologists (71.38 %) than urologists (57.91 %); while PVS and periurethral injection were more commonly performed by urologists than gynecologists. Similar surgical trends were found during time-frame comparison, 2006–2010 vs 1997–2005. SUI surgeries increased in patients aged ≥60, surgeons aged ≥ 50, and in regional hospitals.
Conclusion
This follow-up study depicts the increase in popularity of MUS and offers evidence of surgical trends and a paradigm shift for female SUI surgery. More older women were willing to seek healthcare and undergo surgery. The surgical skills and knowledge spread from medical centers into regional hospitals. The time-frame shift may have a profound impact on patients, as well as the healthcare providers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) is the complaint of involuntary leakage on effort or exertion or on sneezing or coughing, which is caused by sphincter deficiency and/or urethral hypermobility [1]. SUI is a prevalent disease with a high socioeconomic burden and a negative influence on women’s quality of life. It is a common problem affecting approximately 35 % of women above the age of 18 years, and rises up to 45 % at the age of 60 years [2]. From a patient’s perspective, the perceived prevalence of isolated SUI was 18.0 % [3]. Although it has a significant impact on the quality of life of women; it is both greatly underestimated and widely untreated [4]. Approximately two thirds of all incontinent women tend to be restricted in their social activities owing to embarrassment and inconvenience, whilst 19.0 % note that their sex life is affected. Nevertheless, only 27.1 % of the respondents, who suffered from urinary incontinence, and/or related symptoms, had sought medical services to relieve these problems [3]. Moreover, our recent report showed that the overall healthcare seeking prevalence among patients of lower urinary tract symptoms in Taiwan was only 2.17 %, and 1.95 % for patients with storage symptoms [5].
Surgical treatment for SUI is usually considered after the failure of conservative therapy or drug treatment [6]. Our previous study reported a significant change in the distribution of different surgical types for female SUI among patients’ age, surgeons’ specialties, and hospital accreditations during the period 1997 to 2005 [7]. Among the many available types of surgery, which include retropubic urethropexy (RPU), needle suspension, traditional pubovaginal sling (PVS), tension-free midurethral sling (MUS), and periurethral injections, MUS insertion has gained rapid acceptance [6]. These surgeries were designed to prevent involuntary loss of urine from the urethra during increased intra-abdominal pressure with different mechanisms, e.g., repositioning, stabilizing the urethra, creating support for urethral compression, improving urethral coaptation, and offering dynamic midurethral support, etc. [8]. There has been a rapid adoption of midurethral synthetic sling insertion as the first-line surgical option for SUI because it is effective, less invasive, and patients recover more quickly [6]. The introduction of MUS in the mid-1990s by Ulmsten and Petros was the beginning of a revolution in the treatment of SUI over the last two decades. Initially, MUS were implanted via a retropubic approach. Later, the transobturator approach was introduced by Delorme. MUS with its impressive success rates has very quickly gained worldwide popularity. There are other surgical procedures, e.g., RPU, that emphasize bladder neck suspension, includes the original Marshall–Marchetti–Kranz (MMK) procedure, and subsequent modified Burch colposuspension. PVS, which emphasizes the suburethral support with either autologous fascia or synthetic material at the bladder neck level includes the Goeball and Stoeckel procedure and subsequent Raz's modification.
Based upon the National Health Insurance (NHI) claims data in Taiwan, our study was designed to describe the surgical trends of various primary surgeries for female SUI during 2006–2010. The study extended our previous observation of the changing trends of surgical types for SUI [7], especially focusing on the increase in popularity of MUS during 2006–2010. We also evaluated the time-frame comparison, during these two study periods, 1997–2005 vs 2006–2010.
Materials and methods
Data source
The data used in this study were obtained from the National Health Insurance Research Database (NHIRD). The NHIRD was established by the National Health Research Institute, in cooperation with the National Health Insurance Bureau, with the aim of undertaking research into current and emerging issues in Taiwan. The details of NHIRD was described in our previous report [7]. Briefly, it offered information on NHI-reimbursed hospital discharges including inpatient characteristics, the dates of admission and discharge, the type of disease, and the surgery code (based upon the International Classification of Diseases, 9th Revision, Clinical Modification, ICD-9-CM). The information about conservative therapy or drug treatment prior to the SUI surgery was not available in our inpatient data bank. Anonymous identifiers of the medical institutions and the physician were used to link the hospital discharges data to the physician and hospital registries. All discharges from 2006 to 2010 were included in this study, while the data from 1997 to 2005 were used for reference. Confidentiality assurances were ensured abiding by data regulations of the Bureau of NHI. We consulted with the Institutional Review Board of Chi Mei Foundation Hospital and obtained a formal written waiver for the need for ethics approval (No. 10202-E08).
Study subjects
The study subjects were female patients who had undergone primary surgeries for SUI in Taiwan between 1 January 2006 and 31 December 2010. A total of six surgical types for SUI are reimbursed by the NHI: RPU (ICD-9-CM code 59.5), including the Marshall–Marchetti–Kranz procedure or Burch colposuspension; PVS (code 59.4), MUS (code 59.79), including retropubic and transobturator tapes; urethral–vesical junction Kelly plication (code 59.3); bladder neck needle and paraurethral needle suspensions (code 59.6); and periurethral injection of implants into the urethra/bladder neck (code 59.72). Afterward, a total of 15,099 female inpatients who had undergone primary surgeries for SUI during the period were identified and recruited for analysis. The inclusion criteria for SUI surgery include both single SUI surgery and/or concomitant surgical procedures. The study designs were the surgical trend and time-frame comparison purposes; therefore, we followed the same principle of recruitment as our previous work [7].
Variable definitions
The variables used in this study fall into the following three categories:
-
1.
Patients’ age, which was divided into six age groups: from <40 years, 40–49 years, 50–59 years, 60–69 years, 70–79 years, and ≥80 years.
-
2.
Surgeons’ characteristics (age, gender, and specialty). The surgeons’ age was divided into three age groups, from < 40 years, 40–49 years, and ≥50 years; the surgeons’ specialty was divided into three specialty groups (gynecology, urology or others), which are defined by reference to the department into which the patient was admitted.
-
3.
Hospital characteristics (accreditation level and hospital ownership). The hospitals are accredited by the Taiwan Joint Commission on Hospital Accreditation (TJCHA), which is supervised by the Department of Health, Executive Yuan (Taiwan), and classified into three levels (medical centers, regional hospitals, and local hospitals) based on healthcare quality, medical teaching ability, clinical capabilities, and bed capacity. Hospital ownership was classified into nonprofit hospitals, government-owned hospitals, and private for-profit hospitals.
Statistical analysis
Frequency distribution of primary surgical types for SUI, by year, patients’ age, surgeons’ age, specialty, and hospital levels from 2006 to 2010 were performed. Chi-squared tests were performed to examine the distribution of the six surgical types for SUI amongst the patient, surgeon, and hospital characteristic groups. Besides, Chi-squared tests were also performed to compare the differences in the distribution of the six surgical types for SUI between two periods (1997–2005 and 2006–2010). The significance of the statistics is determined using a p value of <0.05. All of the analyses in this study were carried out using the SAS system software for Windows, Version 9.3.1.
Results
Overall surgical changing trend
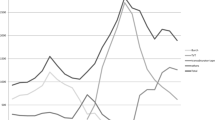
A total of 15,099 female inpatients who had undergone primary surgeries for SUI during the period were recruited. The most frequently used surgical type during the study period was MUS, with a total of 10,387 cases over the 2006–2010 period (accounting for 68.79 % of all cases), followed by 3,047 cases of RPU (20.18 %) and 855 cases of PVS (5.66 %), and other surgical types with 810 cases (5.36 %). The annual number of SUI surgeries increased from 2,571 in 2006 to 3,095 in 2010. During the follow-up study, MUS increased significantly from 53.09 % in 2006 to 78.74 % in 2010. It was concomitantly associated with a decrease in RPU from 29.68 % to 12.99 %, PVS from 9.33 % to 3.46 %, Kelly plication from 3.07 % to 2.00 %, needle suspensions from 2.18 % to 0.97 %, and periurethral injection from 2.64 % to 1.84 % (Table 1). The transition of RPU predominance to MUS predominance occurred between 2005 and 2006 (Fig. 1).
Types of surgery amongst different patient ages
Midurethral sling was most commonly used among all patient age groups: patients aged ≥ 40 years (66.67-–0.45 %), compared with < 40 years (59.41 %); while RPU was more commonly used in patients aged <50 years (21.76–23.23 %) compared with those aged ≥ 50 years (15.94–20.48 %). Periurethral injection was higher in patients aged < 40 years (11.23 %) and those aged > 70 years (2.80–2.90 %), compared with patients aged between 40 and 69 years (Table 2).
Types of surgery by surgeon age and specialty
As for the surgeons’ age, MUS was more commonly used by surgeons aged < 50 years, compared with those aged ≥ 50 years (65.63 %, 76.09 % vs 59.50 %), while PVS (7.50 % vs 1.46, 5.04 %) and periurethral injection (5.09 % vs 11.13, 0.67 %) were more commonly performed by surgeons aged ≥ 50 years (Table 2).
As for surgeon specialty, significant differences were discernible in the distribution of incidences of the various primary surgical types to treat SUI between gynecologists and urologists (χ2 = 1,987.34, p value <0.0001). Of all surgeries 12,351 (81.8 %) were performed by gynecologists, whilst 2,649 (17.5 %) were performed by urologists. Nevertheless, a comparison between the practice patterns of surgeons with different specialties reveals that MUS was the most commonly adopted surgery by both gynecologists (71.38 %) and urologists (57.91 %). Gynecologists were found to be 1.23 times more likely to perform MUS, whilst there was almost equal distribution in the respective adoption of RPU (20.05 % vs 21.10 %) and needle (1.12 % vs 0.87 %) operations in a comparison of gynecologists and urologists. The use of Kelly plication was more commonly found amongst gynecologists than urologists (2.53 % vs 0.11 %); conversely, the use of PVS and periurethral injection was found to be slightly more popular amongst urologists than gynecologists (9.29 % vs 4.87 % and 10.72 % vs 0.05 % respectively).
Types of surgery by hospital accreditation levels and ownership types
Significant differences were discernible in the distribution of incidences of the various primary surgical types for SUI amongst different hospital accreditation levels (χ2 = 1,172.13, p value <0.0001) and types of hospital ownership (χ2 = 384.59, p value <0.0001; Table 2). MUS was the most commonly adopted procedure for hospitals of all accreditation levels (ranging from 50 % to 76 %), whilst medical centers performed the highest proportion of MUS operations (6,774/10,387; 65 %). Medical centers were found to be 1.3 times more likely to perform MUS than regional hospitals (76.46 % vs 59.32 %) and 1.5 times more likely to perform MUS than local hospitals (76.46 % vs 50.41 %). The results also showed that medical centers (12.82 %, 5.03 %, and 0.37 %) tended to perform slightly fewer RPU, PVS, and needle operations than either regional hospitals (30.21 %, 6.42 %, and 1.29 %) or local hospitals (32.86 %, 7.3 %, and 6.19 %); however, they were more likely than either regional hospitals or local hospitals to perform periurethral injection (3.18 %, 0.80 %, and 0.51 %). MUS was also found to be the most commonly adopted procedure amongst hospitals of all ownership types (ranging from 61 % to 72 %), whilst MUS operations were mainly performed in government hospitals (58 %).
Time-frame comparison during 2006–2010 vs 1997–2005
During time-frame comparison, MUS increased 2.7 times (68.79 % vs 25.25 %), accompanied by a decrease in RPU 2.3 times (46.84 % vs 20.18 %) and a decrease in PVS 2.8 times (15.96 % vs 5.66 %). SUI surgeries increased in patients aged ≥60 (28.79 % vs 33.75 %), surgeons’ aged ≥ 50 (22.36 % vs 22.75 %), and in regional hospitals (27.24 % vs 34.79 %), which was associated with a decrease in the medical centers (66.76 % vs 58.68 %; Table 3).
Discussion
Based on a population-based nation-wide data base, our study observed the significant changes in clinical practice with regard to primary surgeries for SUI. MUS significantly increased up to 78 % in 2010, concomitantly decreasing the numbers of RPU and PVS considerably. In a recent review by Cox et al., MUS has been demonstrated to be just as effective as these traditional procedures, e.g., RPU and PVS, but with less associated morbidity, based on randomized controlled trials. Thus, MUS is granted as a new “gold standard” first-line surgical treatment for women with uncomplicated SUI [9]. This follow-up study depicts the increase in popularity of MUS and offers evidence for surgical trends and a paradigm shift for SUI surgery, based on a nation-wide population-based data bank. Similar findings were also observed in other studies [10]. Thus, MUS inserted via either the retropubic or the transobturator approach has become the most popular first-line surgical treatment for women with uncomplicated SUI. Meanwhile, the popularity of different surgical types waxed and waned after the emergence of MUS [9, 11]. This was because it was easy-to-use, there was a high success rate, it was minimally invasive, and had a rapid convalescent period [6]. Meanwhile, the reimbursement of TVT by the NHI system in Taiwan may explain the transition during 2005–2006.
Our overall annual case number during 2006–2010 was stationary, which followed a steep increase during our previous study period, 1997–2005 [7]. It is similar to a serial study among Medicare beneficiaries in the United States aged over 65 years: the overall number of surgical procedures increased from 1992 to 2001 [12], but showed a stable number afterward from 2002 to 2007 [13]. Other contemporary articles, including those on younger women, have actually shown a dramatic increase in the number of incontinence procedures performed [10]. This increase in the number of surgical procedures is worldwide, which is directly related to the introduction of the minimally invasive MUS [14]. Our data showed that MUS surgery has reached a plateau in Taiwan after a period of dramatic increase with a slight decrease between 2009 and 2010, which may be the result of the announcement of serious complications associated with transvaginal placement of surgical mesh by a US Food and Drug Administration warning letter that was first released in 2008 [15]. In a Cochrane Database System Review, MUS was found to be as effective as RPU, with lower perioperative morbidity, and displays high and long-term cure rates in patients with SUI [16]. Long-term data on the retropubic tension-free-vaginal tape (TVT; Gynecare, Somerville, NJ, USA) for uncomplicated SUI suggest that 77–93 % of patients remain cured 10 years after sling placement [17, 18]. This compares with the Burch procedure, the previous standard of care for SUI surgery, which has a reported 72–94 % cure rate after 10 years [19]. Systematic review of the literature found PVS to have a long-term cure/dry rate of 84–96 %, compared with 73 % for the Burch procedure [20]. In our previous review, the transobturator approach reduced some of the severe complications associated with the retropubic implantation route (e.g., bladder perforation, retropubic bleeding, and hematoma), but there was a higher risk of groin/thigh pain and higher rates of vaginal erosion [21]. However, the ICD-9 codes do not provide detailed information regarding the MUS material and the either retropubic or transobturator approach of the MUS types performed because of the nature of the claims data. Also, information on complications and reoperation were not available in this study.
This study has revealed the diversity in the distribution of the various primary surgical types amongst patients in different age groups. MUS was most commonly used among all patient age groups, especially in patients aged ≥ 40 years, compared with those aged less than 40 years. RPU was more commonly used in patients aged < 50 years. Periurethral injection was higher in those aged < 40 years, and those aged ≥ 70 years. It may be because of the minor degree of SUI in the younger age group, and less invasiveness in the aged, frail and/or comorbid patients [2]. Kelly plication was more commonly used in patients aged ≥ 60, possibly because of easy-to-perform and easily available characteristics. Kelly plication and needle suspension play smaller and smaller roles in modern practice of SUI surgeries [22]. This study confirms that patients’ age is one of the factors that the appropriate surgical type selection should take into account [23]. The treatment option on the coexistent SUI and pelvic organ prolapse, either with staged or concomitant surgery remained debatable. Women with apical prolapse can undergo repair via an abdominal route or a vaginal route. The choice of a surgical route for pelvic organ prolapse may also affect the choice of surgery for SUI. This study included both SUI surgery alone and concomitant surgery because of time-frame comparison with our previous study.
The choice of surgical procedures may more or less depend on the surgeons’ preferences for the treatment options [24]. As for surgeons’ age, MUS was more commonly used by surgeons aged < 50 years, while PVS and periurethral injection were more commonly performed by surgeons aged ≥ 50 years. Surgeons’ specialty is also found to be a variable. MUS was more commonly used by gynecologists (71.38 %) than urologists (57.91 %); on the contrary, PVS and periurethral injection were more commonly used by urologists than gynecologists. This reflects the emergence of new instruments and techniques and the training background [25].
There were significant differences in the distribution of various primary surgical types among hospitals of different accreditation levels. MUS was most commonly used in medical centers, 76.46 %, followed by regional hospitals, 59.32 %, and local hospitals, 50.41 %. It is worth noting that MUS, which is regarded as a novel and innovative technique, was performed mostly in the medical centers. The adaptation of newly developed techniques may start in medical center, and then spread the knowledge and techniques to regional and local hospitals. Therefore, in addition to the patients’ conditions, the choices of surgical procedures are partly dependent, to some extent, on the hospitals that they attend and the specialties of the surgeons with whom they consult [26]. Rogo-Gupta reported an increase in ambulatory surgery center, and decline in the hospital inpatient setting for urinary incontinence [13]. This decline may be in part because of an increase in minimally invasive treatment options and shifts in insurance reimbursement supporting procedures in less-expensive ambulatory settings [13]. This variability would, in turn, have implications for both the patients and the surgical modalities selected [26]. The necessity of proper training prior to performing MUS procedures has been proposed by medical associations worldwide [27].
Several variables were found during the time-frame comparison between 1997–2005 and 2006–2010. MUS increased, accompanied by the decreases in RPU, PVS, and others. Our study confirmed that MUS has gained popularity during recent years. Some concerns on the use of MUS remained. In contrast to RPU, only a few long-term studies of retropubic MUSs have been published [28]. Moreover, no long-term studies on transobturator MUS exist. Serati et al. reported that TVT had a subjective satisfaction rate of 89.7 % after 10 years [18]. However, a slight but not significant trend toward a decrease in satisfaction in comparison to the 1-year data (93.7 %) was seen. The data for objective cure also decreased slightly (from 95.2 % to 93.1 %) [18]. Whether this development of the role of different surgical procedures will stand the test needs long-term follow-up. The FDA announcements [15] and mid-term follow-up studies may change the rather euphoric acceptance of MUS as a solution for all patients. The importance of the long-term surgical effectiveness of SUI treatments cannot be over-emphasized [29].
One interesting phenomenon noted in this study is that more primary SUI surgeries were carried out in patients aged ≥60. More aged women were willing to seek healthcare and undergo surgery, in contrast to a stable number among the Medicare beneficiaries in the United States between 2002 and 2007 [13]. The aging of the population, as well as the willingness of aged women to undergo SUI surgeries, deserves our attention. Also, the higher incidence of mixed urinary incontinence and pure urge urinary incontinence in older age groups may be the factor in the decision on the choices of surgical type. This finding may be attributable to the higher expectations of quality-of-life amongst aged women, including their active engagement in social activities. Menopausal status and ageing, but not body mass index, influence the outcome of anti-incontinence surgery [23]. Other findings included more SUI surgeries, which were performed by surgeons aged ≥ 50. The aging of gynecologists and lower recruitment of young gynecologists are potential physician resource problems. More SUI surgeries were performed by female surgeons, which implies that more female doctors entered the field of urogynecology. More SUI surgeries were carried out in regional hospitals, which was associated with a decrease in the number carried out at medical centers. The surgical skills and knowledge spread from the medical centers into regional hospitals.
Although, surgery has been associated with impressive cure rates, it is also associated with significant potential complications, such as impaired bladder emptying, bladder overactivity, incidental bladder perforation, etc. (data were not available in the present study). A variety of conservative managements are demonstrated to be beneficial, cost-effective, and to have minimal side effects, including behavioral therapy (e.g., bladder training, fluid and dietary modification), pelvic floor muscle training with or without biofeedback, weighted vaginal cones, electrical stimulation, incontinence pessary, and drug treatment. The conservative management can be offered as a first-line treatment, while temporarily or permanently avoiding invasive procedures. Despite there being no universal data owing to the inaccessibility of outpatient data, some of the medical centers in Taiwan utilize a variety of measures, for example, pad weight, for screening the patients who do indeed need a MUS [30]. The utilization of these measures to select patients for midurethral slings was based on the belief that mild SUI can be improved by pelvic floor exercise and/or medications, while MUS can be avoided.
Certain limitations remain in this study which should be taken into consideration. First, the lack of availability of appropriate data has made the definitive diagnosis, e.g., pure stress urinary incontinence or mixed urinary incontinence, urodynamic study diagnosis, etc., unavailable because of the initial purpose of the NHI for insurance coverage, instead of scientific purpose. Second, the miscoding of some surgical procedures was inevitable. Third, the information about conservative therapy or drug treatment prior to the SUI surgery was not available in our inpatient data bank. There are factors that might interact with the primary surgical trends presented, e.g., conservative therapies, pelvic floor muscle training, drug treatment, complication rates, and previous/concomitant urogynecological surgery. Nevertheless, despite these limitations, this study has provided a descriptive analysis of SUI, based upon a trend of a nationwide databank including the surgical type, patient age, and the surgeon’s specialty.
Conclusion
Midurethral sling has the greatest gain in popularity, and could potentially revolutionize the practice of surgery for SUI. This follow-up study depicts the increase in popularity of MUS and offers evidence of surgical trends and a paradigm shift for female SUI surgery. More aged women were willing to seek healthcare and undergo surgery. The surgical skills and knowledge spread from medical centers into regional hospitals. The increasing availability of the various types of treatment modality present the possibility of tailoring therapies to the desires and needs of individual patients [8].
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al (2003) The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 61(1):37–49
Mohr S, Siegenthaler M, Mueller MD, Kuhn A (2013) Bulking agents: an analysis of 500 cases and review of the literature. Int Urogynecol J 24(2):241–247
Chen GD, Lin TL, Hu SW, Chen YC, Lin LY (2003) Prevalence and correlation of urinary incontinence and overactive bladder in Taiwanese women. Neurourol Urodyn 22(2):109–117
Yu HJ, Wong WY, Chen J, Chie WC (2003) Quality of life impact and treatment seeking of Chinese women with urinary incontinence. Qual Life Res 12(3):327–333
Wu MP, Hsu YW, Weng SF, Ho CH, Wang JJ, Tong YC (2013) Healthcare-seeking prevalence of lower urinary tract symptoms among National Health Insurance Enrollees in Taiwan, 2000–2009. Urology 81(1):61–65
Lucas MG, Bosch RJ, Burkhard FC, Cruz F, Madden TB, Nambiar AK et al (2013) EAU guidelines on surgical treatment of urinary incontinence. Actas Urol Esp 37(8):459–472
Wu MP, Huang KH, Long CY, Huang KF, Yu KJ, Tang CH (2008) The distribution of different surgical types for female stress urinary incontinence among patients’ age, surgeons’ specialties and hospital accreditations in Taiwan: a descriptive 10-year nationwide study. Int Urogynecol J Pelvic Floor Dysfunct 19(12):1639–1646
Rovner ES, Wein AJ (2004) Treatment options for stress urinary incontinence. Rev Urol 6 [Suppl 3]:S29–S47
Cox A, Herschorn S, Lee L (2013) Surgical management of female SUI: is there a gold standard? Nat Rev Urol 10:78–89
Jonsson Funk M, Levin PJ, Wu JM (2012) Trends in the surgical management of stress urinary incontinence. Obstet Gynecol 119(4):845–851
Hsu PY, Long CY, Huang YT, Huang KH, Tang CH, Wu MP (2013) The vicissitudes of open and laparoscopic retropubic urethropexy for stress urinary incontinence in Taiwan: an 11-year nationwide analysis. Gynecol Minim Invasive Ther 2(1):22–26
Anger JT, Weinberg AE, Albo ME, Smith AL, Kim JH, Rodriguez LV et al (2009) Trends in surgical management of stress urinary incontinence among female Medicare beneficiaries. Urology 74(2):283–287
Rogo-Gupta L, Litwin MS, Saigal CS, Anger JT, Urologic Diseases in America P (2013) Trends in the surgical management of stress urinary incontinence among female Medicare beneficiaries, 2002–2007. Urology 82(1):38–41
Lee J, Dwyer PL (2010) Age-related trends in female stress urinary incontinence surgery in Australia—Medicare data for 1994–2009. Aust N Z J Obstet Gynaecol 50(6):543–549
FDA (2008) FDA Public Health Notification: Serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. Issued: 20 October 2008
Ogah J, Cody JD, Rogerson L (2009) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev (4):CD006375
Nilsson CG, Palva K, Rezapour M, Falconer C (2008) Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 19(8):1043–1047
Serati M, Ghezzi F, Cattoni E, Braga A, Siesto G, Torella M et al (2012) Tension-free vaginal tape for the treatment of urodynamic stress incontinence: efficacy and adverse effects at 10-year follow-up. Eur Urol 61(5):939–946
Alcalay M, Monga A, Stanton SL (1995) Burch colposuspension: a 10–20 year follow up. Br J Obstet Gynaecol 102(9):740–745
Dmochowski RR, Blaivas JM, Gormley EA, Juma S, Karram MM, Lightner DJ et al (2010) Update of AUA guideline on the surgical management of female stress urinary incontinence. J Urol 183(5):1906–1914
Long CY, Hsu CS, Wu MP, Liu CM, Wang TN, Tsai EM (2009) Comparison of tension-free vaginal tape and transobturator tape procedure for the treatment of stress urinary incontinence. Curr Opin Obstet Gynecol 21(4):342–347
Thaweekul Y, Bunyavejchevin S, Wisawasukmongchol W, Santingamkun A (2004) Long term results of anterior colporrhaphy with Kelly plication for the treatment of stress urinary incontinence. J Med Assoc Thai 87(4):357–360
Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Bogusiewicz M, Skorupski P (2010) Body mass index does not influence the outcome of anti-incontinence surgery among women whereas menopausal status and ageing do: a randomised trial. Int Urogynecol J 21(7):801–806
Young JM, Solomon MJ, Harrison JD, Salkeld G, Butow P (2008) Measuring patient preference and surgeon choice. Surgery 143(5):582–588
Nosnik IP, Friedmann P, Nagler HM, Dinlenc CZ (2010) Resume fraud: unverifiable publications of urology training program applicants. J Urol 183(4):1520–1523
Griffiths JM, Black NA, Pope C, Stanley J, Bowling A, Abel PD (1998) What determines the choice of procedure in stress incontinence surgery? The use of multilevel modeling. Int J Technol Assess Health Care 14(3):431–445
Society of Obstetricians and Gynaecologists of Canada (SOGC) (2005) Tension-free vaginal tape (TVT) procedure. Int J Gynaecol Obstet 91(3):279–282
Nilsson CG, Palva K, Aarnio R, Morcos E, Falconer C (2013) Seventeen years’ follow-up of the tension-free vaginal tape procedure for female stress urinary incontinence. Int Urogynecol J 24(8):1265–1269
Dwyer PL (2013) Nothing lasts forever? Long-term outcomes of stress urinary incontinence surgery. Int Urogynecol J 24(8):1241–1242
Chang TC, Hsiao SM, Chen CH, Wu WY, Lin HH (2014) Utilizing preoperative 20-minute pad testing with vaginal gauze packing for indicating concomitant midurethral sling during cystocele repair. Eur J Obstet Gynecol Reprod Biol 172:127–130
Acknowledgements
The authors are grateful for the financial support provided by Chi Mei Foundation Hospital, Taiwan (CMFHR10231 and CMFHR10243). Dr S.M. Hsiao, C.C. Liang, S.J. Liang, and M.P. Wu are investigators of Taiwan Urogynecologic Group (TUGG), Taiwan Urogynecology Association (TUGA), Taiwan.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, CJ., Tong, YC., Hsiao, SM. et al. The surgical trends and time-frame comparison of primary surgery for stress urinary incontinence, 2006–2010 vs 1997–2005: a population-based nation-wide follow-up descriptive study. Int Urogynecol J 25, 1683–1691 (2014). https://doi.org/10.1007/s00192-014-2443-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2443-5