Abstract
Background
We conducted a prospective randomized controlled noninferiority trial to compare objective and subjective outcomes of retropubic tension-free vaginal tape (TVT) with those of transobturator tape (TVT-O) as primary treatment for stress urinary incontinence (SUI) in women.
Study design
The study was conducted at 25 gynecology units in Austria and Germany; regional and academic hospitals participated. A total of 569 patients were randomly assigned to undergo TVT or TVT-O.
Results
A total of 480 patients (85 %) were examined at 3 months. A negative cough stress test with stable cystometry to 300 ml was seen in 87 % of patients after TVT and in 84 % after TVT-O; 64 % and 59 % of patients, respectively, reported no pad use, and 88 % of patients in both groups considered themselves much or very much better on the Patient Global Impression of Improvement (PGI-I) scale. Quality of life (QoL) as assessed with the SF-12 Health Survey, Kings’ Health Questionnaire, (KHQ), and EuroQol-5D (EQ-5D) was significantly improved in both arms, with no differences between arms. There were no significant differences in postoperative pain or complications.
Conclusions
Results of this trial demonstrate noninferiority between TVT and TVT-O with regard to postoperative continence and QoL and suggest little difference in perioperative problems (ClinicalTrials.gov NCT 00441454).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1996, Ulmsten et al. [1] described transvaginal retropubic insertion of a tape composed of polypropylene mesh under the midurethra to address stress urinary incontinence (SUI) in women. The retropubic tension-free vaginal tape (TVT) operation, as it came to be known, was introduced commercially in Europe in 1998. Subsequently, the procedure was compared with open colposuspension [2] and has become a standard of care in the surgical management of SUI in women [3]. In 2001, Delorme [4] described an alternative surgical approach that placed a tape of synthetic material through the obturator foramen rather than retropubically. The supposed rationale was that the transobturator approach was as efficacious for treating SUI but simpler and safer than the retropubic approach. Two years later, de Leval [5] described a further transobturator procedure, the so-called TVT-O. This procedure used the same polypropylene tape material as the original retropubic procedure and, in contrast to the Delorme procedure, was placed outward through the obturator foramen from a suburethral incision in the anterior vaginal wall [5].
The Austrian Urogynecology Working Group conducted a prospective randomized controlled noninferiority trial to compare objective and subjective outcomes and perioperative data of TVT with those of TVT-O as primary treatment for SUI in women.
Material and methods
This study was initiated, planned, and conducted by the Austrian Urogynecology Working Group and conducted at 25 gynecology units in Austria and Germany. Regional and academic hospitals both participated. The Ethics Committee of the Medical University of Graz and the institutional review boards at all participating centers approved the study protocol. All patients gave written informed consent. The trial was planned according to Consolidated Standards of Reporting Trials (CONSORT) guidelines [6] and registered with ClinicalTrials.gov (NCT 00441454). There was no overlap of patients with previously published registries of midurethral tape procedures [7, 8]. The tape manufacturer had no role in any aspect of the study and did not provide products for the study.
Inclusion and exclusion criteria
Inclusion criteria were planned primary surgery for urodynamically verified SUI [9] (positive cough stress test at bladder filling of 300 ml) without concomitant prolapse surgery or hysterectomy, and willingness to participate in follow-up. Exclusion criteria were detrusor overactivity or a predominant complaint of overactive bladder; concomitant prolapse surgery; other major concomitant surgery (i.e., hysterectomy); previous incontinence surgery other than colporrhaphy; residual urine ≥100 ml; neurologic disease; allergy to local anesthetic agents; and coagulation disorders or other contraindications for surgery.
Enrollment, randomization, and follow-up
Preoperative evaluation included a urogynecologic history, bladder diary, and urodynamic studies (cystometry and urethral profilometry). Generic health-related quality of life (QoL) was assessed with the 12-item Short-Form Health Survey (SF-12) [10] and the EuroQol-5D (EQ-5D)[11]; condition-specific QoL was assessed with the German-language version of the King’s Health Questionnaire (KHQ) [12], the Incontinence Outcome Questionnaire (IOQ) [13], and Patient Global Impression of Severity and Improvement (PGI-S and PGI-I)[14].
Patients were randomized according to a computer-generated random list allocating trial identification number and treatment group. Randomization was by fax through the central office of the Austrian Gynecologic Oncology Group. Randomly permutated blocks of ten patients were stratified by study site. Patients, surgeons, and physicians performing follow-up exams were not blinded to the type of surgery. All participating centers and surgeons had substantial experience with TVT; having performed ten previous transobturator procedures was required of participating surgeons. After informed consent, patients were randomized to TVT or TVT-O (Gynecare TVT vs. Gynecare TVT-O; Gynecare, Ethicon).
The procedures were performed according to the descriptions of the original authors [1, 5] and the manufacturer. For pragmatic reasons, method of anesthesia and postoperative analgesia were not stipulated. Cystoscopy was performed with all retropubic placements but not routinely with transobturator insertions. Perioperatively, we collected surgical data, including complications, voiding function (days until residual urine <100 ml), reoperations, and pain at exit site of tape (VAS 0–10) on postoperative day 1 and day of discharge if not day 1.
Postoperatively, participants were evaluated at 3 months, with a further evaluation scheduled at 5 years. The 3-month evaluation included clinical and urodynamic evaluation (cystometry to 300 ml) and QoL questionnaires. This paper reports the results at 3 months.
The primary outcome measure was objective cure of SUI, defined as a negative cough stress test and stable cystometry to 300 ml. Secondary outcomes were QoL measures and complications. Postoperative voiding function and dysfunction was assessed as postoperative days until residual urine <100 ml. De novo overactive bladder (OAB) was defined as a postoperative maximum bladder capacity <300 ml, symptomatic detrusor contractions at cystometry, or both.
Statistical analysis
The study was designed as a noninferiority study and modelled on the UK and Ireland TVT Trial [2]. The hypothesis was that TVT-O is not inferior to TVT for curing female SUI. Sample size was calculated assuming an 80 % cure rate with TVT and that a 10 % difference in cure between procedures would be clinically important. The hypothesis was that there would be no more than a 10 % difference in cure rate between methods. To detect this level of difference with 80 % power would require 198 patients in each arm (262 in each arm for 90 % power). Calculations based on anticipated throughput of the collaborating units gave a pragmatic recruitment target of 500 patients for randomization, so that with an assumed 20 % dropout rate at 3 months, we would have enough patients for analysis. Data were entered into a database (Microsoft Access) and analyzed with SPSS software (Version 20).
Objective and subjective cure rates were tested with contingency tables and the chi-square test. Secondary outcomes were compared with the chi-square test and the Student t test or Wilcoxon rank-sum test, as appropriate. A two-factorial analysis of variance (ANOVA) was carried out to test for differences in reoperation rates, urinary tract infection, pad use, stable cystometry, urodynamic parameters, incontinence episode frequency (IEF), and voids/24 h. Eta-squared was calculated as a measure of effect size for t tests and ANOVAs. A two-factorial ANOVA was used to test for differences on the SF-12, KHQ, PGI-S, and EQ-5D. The t test for independent samples was used to test for differences on the PGI-I scale and the IOQ.
Results
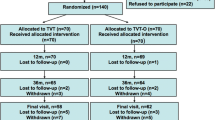
A total of 569 women were randomized to TVT or TVT-O; the flow diagram is shown in Fig. 1. Twenty-five participating centers entered between two and 161 patients. Baseline demographic and clinical characteristics and urodynamic findings in the two groups were similar (Table 1).
Perioperative data and complications are shown in Table 2. Operating times were slightly shorter for the TVT-O. The majority of both procedures were performed with general anesthesia, as opposed to local anesthesia as originally described for the TVT [1]. Bladder perforations were detected in 3.9 % of patients in the TVT group and none in the TVT-O group (although cystoscopy was not performed in the latter group). Increased intraoperative bleeding, pragmatically defined as continued bleeding after 3 min of local pressure, was uncommon in both groups (0.7 % vs. 1.1 %); no patient in either group required red-cell transfusion. Postoperative voiding, defined as days until voiding with a residual urine volume of <100 ml, did not differ between groups (Table 2).
There were five reoperations (0.9 %), all in the perioperative period (Table 2). One patient developed an acute abdomen after TVT; laparotomy showed perforation of the transverse colon. The tape was removed, and the patient subsequently did well, although she did not attend the 3-month follow-up. This complication occurred at one of the largest recruiting centers, albeit by a surgeon who did not have the experience of the ten procedures stipulated by the protocol. One patient after a retropubic TVT developed a localized wound infection that was treated by opening a stitch and using local measures. Three patients (two after TVT and one after TVT-O) required tape loosening in the immediate postoperative period for voiding dysfunction (Table 2). There were no further reoperations by the 3-month follow-up. There was no difference in VAS pain scores on postoperative day 1 or on the day of discharge (if not day 1) or at 3 months. However, at 3 months, the symptom bladder pain on the KHQ questionnaire was reported more often by patients after TVT-O than by those after TVT (p < 0.03).
A total of 480 patients (85 %) were examined at 3 months (Table 3). There were no differences in baseline characteristics and perioperative data between patients who attended follow-up and those who did not. A negative cough stress test with stable cystometry to 300 ml was seen in 87 % after TVT and 84 % after TVT-O (not significant); 64 % and 59 % of patients, respectively, reported no postoperative pad use. The rate of de novo OAB was 10.5 % and 10.1 %, respectively. With regard to PGI-I, 88 % of 261 patients completing the questionnaire considered themselves much or very much better in both groups (Table 3). If patients who did not attend follow-up are counted as failures, the cure rate would be 75.0 % and 72.9 %, respectively (not significant).
QoL assessments before and 3 months after surgery were available for 268 patients (Table 4). Baseline QoL data in the two groups were similar, except for a slightly higher score in the incontinence impact domain of the KHQ in patients receiving a TVT-O. This was statistically significant, but a <10-point difference indicates limited clinical relevance. Both groups reported significant improvement in both SF-12 domains (p < .001; p = .007). In the KHQ domains, both groups reported significant improvement in general health perception, incontinence impact, role limitation, physical limitation, social limitation, emotions, personal relationships, sleep/energy, severity measures, and overactive bladder (all p < .001). Except for general health perception, all changes were clinically significant, as indicated by improvement of >10 points. Both groups showed significant improvement (reduction) in PGI-S (p < 0.001). On the VAS of the EQ-5D, patients reported improvement in imaginable health state (p < 0.001). Although patients in both groups reported significant improvement on the incontinence impact and emotional problems scales, patients treated with TVT-O reported more improvement in both scales than did those in the TVT group (p < 0.016, p < 0.007). Bladder pain was reported more frequently by patients treated with TVT-O (p < 0.026). All differences between groups showed slight effect size. There were no differences between groups at 3 months in any of the IOQ scales (Table 4).
Discussion
Our study, one of the largest comparisons to date of retropubic versus transobturator suburethral slings, shows noninferiority and similar cure rates between the two approaches. The primary 3-month outcome of negative cough stress test and stable cystometry to 300 ml was seen in 87 % patients after TVT and 84 % after TVT-O. This is consistent with two systematic reviews [15, 16] and similar studies [17–21].
Our results confirm the negative impact of SUI on QoL and that this negative impact can often be alleviated with surgery. The two surgical options showed nearly identical results regarding QoL, with significant improvements in both groups in nearly all scales of SF-12 and KHQ. The improvement in SF-12 scales, which reflect overall but not condition-specific QoL, were statistically significant but not clinically relevant, whereas nearly all changes assessed with the KHQ, a condition-specific instrument, were clinical relevant. A limitation of the QoL aspect of this trial is that complete QoL data at 3 months were available for only about half the enrolled patients.
There were no unexpected differences in intraoperative problems or adverse events in the perioperative period. Bladder perforations were reported only with the TVT procedure, with an incidence of 3.9 %. Undetected perforations may have occurred in the TVT-O group (for which cystoscopy was not mandatory), but we consider this very unlikely, because a previous registry reported only one bladder perforation among 1,200 (inside-out) TVT-O procedures [8]. This is consistent with rates reported in registries [7, 8, 22, 23], and no sequelae were reported. Bowel perforation is a known, albeit uncommon, complication of TVT [7]. The case in this trial occurred at one of the largest participating centers, albeit by a surgeon with less experience than stipulated by the study protocol. There were no bleeding complications requiring reoperation or blood products with either technique, and there were no differences in length of hospital stay. Rates of perioperative complications were in line with previous trials [17–21] and large-scale registries set up to define the scope of complication rates [7, 8, 22, 23]. Our trial also showed no differences in postoperative pain scores perioperatively, although some studies have found more postoperative pain with transobturator compared with retropubic tapes [17–18]. In contrast to the intent of Ulmsten et al. [1], most procedures in the present trial were done under general anesthesia in both groups. Postoperative pain management was not stipulated in the protocol, for pragmatic reasons. At 3 months, the rate of patients reporting pain was low in both groups, but there was a small difference in the pain subscale of the KHQ in favor of TVT.
We designed this study to compare two types of tapes from the same manufacturer because the original TVT was by far the most widely used system in our region prior to the advent of TVT-O; also, TVT-O uses the same type of tape material. Retrospectively, this was a good decision because some of the early transobturator systems were associated with material-related complications and are no longer available [8].
With the trial conducted by the Urinary Incontinence Treatment Network [21], ours is the largest reported prospective randomized trial of retropubic vs. transobturator tapes. Strengths of the study are the large number of patients, the relatively large and diverse number of participating centers, and the restriction to two products using the same type of tape and differing only in insertion technique, with exclusion of major concomitant surgery. The 85 % follow-up rate at 3 months is modest. The study was not designed to address differences in postoperative complications, but these have been well assessed in registries with large numbers of patients [7, 8, 22, 23]. The study does not provide information for decision-making in patients with concomitant surgery, particularly prolapse, and those with recurrent incontinence. The results of our trial are not necessarily transferable to other types of retropubic or transobturator tapes and certainly not to single-incision tapes. Surgeons, patients, and physicians doing the follow-up were not blinded. Also, in the meantime, the systems used in this trial have been modified somewhat by the manufacturer, with possible effects on intraoperative problems and postoperative pain profiles [24].
In summary, the results of this trial demonstrate noninferiority between retropubic and transobturator tension-free vaginal tape with regard to postoperative continence and QoL and suggest little difference in perioperative problems.
References
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J 7:81–86
Ward K, Hilton P, on behalf of the UK and Ireland TVT Trial Group (2002) Prospective multicentre randomised trial of tension-free vaginal tape and colposuspension as primary treatment of stress incontinence. BMJ 325:67–74
Ogah J, Cody JD, Rogerson L (2009) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews doi:. doi:10.1002/14651858.CD006375.pub2
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress incontinence in women. Prog Urol 11:1306–1313
de Leval J (2003) (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transbturator vaginal tape inside-out. Eur Urol 44:724–730
Moher D, Schulz KF, Altman DG (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 357:1191–1194
Tamussino K, Hanzal E, Kölle D, Ralph G, Riss PA (2001) The tension-free vaginal tape operation: Results of the Austrian registry. Obstet Gynecol 98:732–736
Tamussino K, Hanzal E, Kölle D, Tamma A, Preyer O, Umek W et al (2007) Transobturator tapes for stress urinary incontinence: Results of the Austrian registry. Am J Obstet Gynecol 197(634):e1–e5
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfuction. Int Urogynecol J 21:5–26
Ware J Jr, Kosinski M, Keller SD (1996) A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
EuroQol Group (1990) EuroQol - a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Bjelic-Radisic V, Dorfer M, Tamussino K, Greimel E (2005) Psychometric properties and validation of the German language King’s Health questionnaire. Neurourol Urodyn 24:63–68
Bjelic-Radisic V, Dorfer M, Tamussino K, Frudinger A, Kern P, Winter R, Greimel E (2007) The Incontinence Outcome Questionnaire: an instrument for assessing patient-reported outcomes after surgery for stress urinary incontinence. Int Urogynecol J 18:1139–1149
Yalcin I, Bump RC (2003) Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol 89:98–101
Latthe PM, Foon R, Toozs-Hobson P (2007) Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG 114:522–531
Sung VW, Schleinitz MD, Rardin CR, Ward RM, Myers DL (2007) Comparison of retropubic vs transobturator approac to midurethral slings: a systematic review and meta-analysis. Am J Obstet Gynecol 197:3–11
Barber MD, Kleeman S, Karram MM et al (2008) Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence – A randomized controlled trial. Obstet Gynecol 111:611–621
Laurikainen E, Valpas A, Kivelä A et al (2007) Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. Obstet Gynecol 109:4–11
Deffieux X, Daher N, Mansoor A, Debodinance P, Muhlstein J, Fernandez H (2010) Transobturator TVT-O versus retropubic TVT: results of a multicenter randomized trial at 24 months follow-up. Int Urogynecol J 21:1337–1345
Krofta L, Feyereisl J, Otcenasek M, Velebil P, Kasikova E, Krcmar M (2010) TVT and TVT-O for surgical treatment of primary stress incontinence: prospective randomized trial. Int Urogynecol J 21:141–148
Richter HE, Albo ME, Zyczynski HM et al (2010) Retropubic versus transobturator slings for stress incontinence. N Engl J Med 62:2066–2076
Kuuva N, Nilsson CG (2002) A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand 81:72–77
Schraffordt Koops SE, Bisseling TM, Heintz AP, Vervest HA (2005) Prospective analysis of complications of tension-free vaginal tape from The Netherlands Tension-free Vaginal Tape study. Am J Obstet Gynecol 193:45–52
de Leval J, Thomas A, Waltregny D (2011) The original versus a modified inside-out transobturator procedure: 1-year results of a prospective randomized trial. Int Urogynecol J 22:145–156
Acknowledgments
We gratefully acknowledge the following participating centers and investigators: Geburtshilflich-gynäkologische Univ.-Klinik Graz (T. Aigmüller, K. Tamussino, V. Bjelic-Radisic, A. Giuliani, E. Greimel, J. Haas); Wilhelminenspital Wien (A. Tammaa, A. Mirna, R. Novak, B. Reichetzer, H. Salzer); Univ.-Frauenklinik Wien (E. Hanzal, W. Umek, K. Elenskaia); Univ.-Frauenklinik Innsbruck (D. Kölle, S. Kropshofer); LKH Mödling (A. Dungl, S. Hinterholzer, P. Riss); LKH Leoben (G. Müller, G. Ralph); Krankenhaus der Barmherzigen Brüder Graz (P. Lang, E. Gruber-Fröhlich, O. Preyer, E. Rothe); LKH Klagenfurt (K. Fabel, G. Mori); Krankenhaus der Barmherzigen Brüder Wien (G. Wagner); LKH Wiener Neustadt (C. Gamper, R. Schacherl); Krankenhaus der Barmherzigen Schwestern Linz (J. Angleitner, G. Hartmann); Krankenhaus Amstetten (K. Weghaupt); LKH Bad Ischl (A. Bichler); LKH Judenburg (M. Börecz, P. Klug); LKH Dornbirn (W. Neunteufel); LKH Wels (H.J. Huemer, K. Reisenberger); LKH Feldbach (M. Konrad, H.M.H. Hofmann); Krankenhaus der Barmherzigen Brüder St. Veit (A. Roth, F. Ronaghi); LKH Gmunden (E, Kostersitz, G. Hartmann); BKH Schwaz (D. Kölle); Donauspital Wien (K. Philipp); KH Korneuburg (P. Safar); Hanusch KH (M. Medl, D. Uhl); Amper-Klinikum Dachau (U. Peschers, G. Debus); Klinik für Frauenheilkunde/Campus Innenstadt, University of Munich (K. Jundt).
Financial support
Austrian Urogynecology Working Group
Conflicts of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Drs. Aigmüller and Tammaa contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Aigmüller, T., Tammaa, A., Tamussino, K. et al. Retropubic vs. transobturator tension-free vaginal tape for female stress urinary incontinence: 3-month results of a randomized controlled trial. Int Urogynecol J 25, 1023–1030 (2014). https://doi.org/10.1007/s00192-014-2384-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2384-z