Abstract
Introduction and hypothesis
To evaluate the effect of levator ani muscle (LAM) injury on pelvic floor disorders and health-related quality of life in Chinese primiparous women during the first year after delivery.
Methods
At 8 weeks and 12 months after delivery, 328 women were assessed for symptoms of pelvic floor disorders and quality of life using the standardised questionnaire, POP-Q; and translabial ultrasound to detect LAM injury. Descriptive analysis, independent sample t test, non-parametric testing, Chi-squared test and two-sided Fisher’s exact test were used.
Results
At 8 weeks after delivery, 48 (19.0 % [95 % CI, 14.2–23.8 %]) women with vaginal delivery had LAM injury; 38 women (79.2 %) had persistent LAM injury at 12 months. At 8 weeks, LAM injury was associated with prolapse symptoms, descent at Pelvic Organ Prolapse Quantification (POP-Q) Aa and Ba points and a higher Pelvic Organ Prolapse Distress Inventory (POPDI) general and Urinary Distress Inventory (UDI) Obstructive subscale score. At 12 months, it was not associated with prolapse symptoms, Pelvic Floor Distress Inventory (PFDI) or Pelvic Floor Impact Questionnaire (PFIQ). There was also no association between stress urinary incontinence (SUI), urge urinary incontinence (UUI), mixed urinary incontinence (UI), faecal incontinence (FI) with LAM injury at both time points.
Conclusions
Seventy-nine per cent of women who had LAM injury at 8 weeks after vaginal delivery had persistent LAM injury at 12 months. LAM injury was associated with prolapse symptoms, lower POP-Q Aa and Ba points at 8 weeks after delivery and a higher POPDI general and UDI Obstructive subscale scoring. However, we are not able to confirm the association between LAM injury and SUI, UUI, mixed UI, FI at 8 weeks or 12 months after delivery; or prolapse symptoms, PFDI or PFIQ scores at 12 months after delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Levator ani muscle (LAM) injury has been reported in 13–36 % of women after vaginal delivery [1–4]. Many studies have focused on the associated obstetric factors [2, 3, 5, 6]. LAM injury was associated with pelvic organ prolapse and a more severe degree of prolapse [7, 8]. However, the relationship between LAM injuries and stress urinary incontinence remains unclear [9]. There have been conflicting reports with no clear evidence of a positive or negative effect [1, 10].
The majority of the above studies mainly involved Caucasian women and whether these findings are generalisable to other ethnic groups is unknown. Racial differences in structural and pelvic organ mobility have been demonstrated [11, 12]. Besides, information on the effect of LAM injury on health-related quality of life is limited. This study was conducted to evaluate the effect of LAM injury on pelvic floor disorders and health-related quality of life in Chinese women during the first year after delivery.
Materials and methods
This was an extended study of the previously reported prospective observational study with women recruited in a tertiary obstetric unit during the first trimester (9–12 weeks of gestation) from August 2009 to September 2010 [13, 14]. An experienced research assistant recruited Chinese, nulliparous women without symptoms of pelvic floor disorder before the pregnancy. Written informed consent was obtained. Inclusion criteria were Chinese ethnicity, nulliparous women with a singleton pregnancy who had no known urinary incontinence, faecal incontinence or prolapse symptoms prior to pregnancy. Exclusion criteria included younger than 18 years, non-Chinese ethnicity and those who refused to participate. They were followed up at 8 weeks and 12 months after delivery.
At each visit, they were asked if they had experienced symptoms of stress urinary incontinence (SUI), urge urinary incontinence (UUI), faecal incontinence to loose/liquid stool or solid stool (FI) and pelvic organ prolapse (POP). The terminology followed the IUGA/ICS joint report on terminology for female pelvic floor dysfunction [15]. Then, they filled in the validated Chinese Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ) [16]. The PFDI has 46 items and contains three scales, and each scale has its own subscales, assessing the urinary, prolapse and bowel symptoms and the distress caused by the symptoms if present. The PFIQ has 31 items and contains three scales, which measures the impact of urinary, prolapse and bowel symptoms on the health-related quality of life of women. The responsiveness of both PFDI and PFIQ has been confirmed [17]. Following this, pelvic organ prolapse was assessed according to pelvic organ prolapse quantification (POP-Q) and the investigator was blinded to the above information [18]. Lastly, a standard translabial ultrasound scan was performed to assess the pelvic floor by one of the investigators. A GE Voluson 730 3D Ultrasound system (GE Medical Systems, Zipf, Austria) with a 4- to 8-MHz 3D autosweep transducer was used for all imaging. The transducer was placed on the perineum in a mid-sagittal plane with the women in a supine position immediately after voiding. Three-dimensional (3D) ultrasound scan of the pelvic floor anatomy, with a sweep angle of 85° were obtained at rest, at Valsalva and at pelvic floor muscle contraction. Women were asked to perform Valsalva and pelvic floor muscle contractions until a satisfactory performance was achieved. At most, three Valsalva and three pelvic floor contractions were required, with the most effective contraction used for evaluation. The volume data sets were saved and analysed later.
The ultrasound (USG) volume datasets of maximum pelvic floor contraction obtained at 8 weeks after delivery were used to assess LAM injury in a standard way [19]. The LAM was assessed using tomographic ultrasound imaging on volumes obtained at maximal pelvic floor contraction at 2.5-mm slice intervals, from 5 mm below to 12.5 mm above the plane of minimal hiatal dimensions. Following this, measurements of the levator–urethral gap (LUG) were performed [20]. The LAM injury was defined according to the minimal criteria for complete avulsion of the LAM using a cut-off of 23.6 mm for LUG in at least three central slides obtained at the level of minimal hiatal dimension, 2.5 and 5 mm above [21]. The USG volumes obtained at 12 months after delivery were reviewed again for LAM injury in the same way described above. The positions of the pelvic organs, relative to the postero-inferior edge of the pubic symphysis, were measured in centimetres at rest, at Valsalva and at pelvic floor muscle contraction, as described [14, 19]. Pelvic organs proximal to the reference point have a negative value. The hiatal area was also measured in the plane of minimal hiatal dimension [14, 19]. The investigator was blinded to the symptoms and PFDI and PFIQ scoring.
Women were allowed to perform pelvic floor exercise according to their own perceived needs.
Statistical analysis
Indices measured in two groups of subjects were compared using the independent sample t test or non-parametric test where appropriate. For comparison of frequencies, Chi-squared test, or two-sided Fisher’s exact test was used where appropriate. P < 0.05 was considered statistically significant.
Ethics approval
Ethics approval for the study was granted by the local institute (CRE −2009.257)
Results
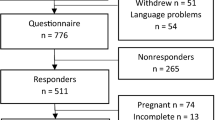
In all, 474 women were invited; 32 declined, with 442 women recruited during the first trimester; 328 women (74.2 %) completed the study. Detailed reasons for withdrawal have been reported previously [13, 14]. Their mean age was 30.6 ± 3.8 years, and mean BMI in the first trimester was 21.0 ± 2.8 kg/m2. The mean gestational age at delivery was 39.2 ± 1.8 weeks and mean birth weight was 3.09 ± 0.47 g. Overall, 192 (58.5 %) had a spontaneous vaginal delivery, 60 (18.3 %) an operative vaginal delivery (46 ventouse and 14 forceps), 13 (4 %) an elective Caesarean section and 63 (19.2 %) an emergency Caesarean section. Among those undergoing vaginal delivery, 24 (9.4 %) women had intrapartum epidural analgesia. The mean duration of the second stage of labour and the active second stage of labour was 38.1 ± 32.1 min and 35.9 ± 28.3 min respectively. A left mediolateral episiotomy was made in 242 women (96 %), 94.8 % of all spontaneous vaginal deliveries and all instrumental deliveries. Thirty-nine and ten, respectively, had a first- or second-degree vaginal tear. There was no third- or fourth-degree vaginal tear.
We have reported that the prevalence of stress urinary incontinence, urge urinary incontinence and faecal incontinence with liquid/solid stool at 8 weeks was 18.6 %, 8.8 %, 5.2 % and at 12 months 25.9 %, 8.2 % and 4.0 % respectively [13]. Symptoms of prolapse at 8 weeks and 12 months were reported by 15.8 % and 7.6 % of women respectively. Pelvic floor biometry during pregnancy and after delivery was also reported [14, 22].
At 8 weeks after delivery, 48 women (19.0 % [95 % CI, 14.2–23.8 %]) who underwent vaginal delivery, either spontaneous delivery or operative vaginal delivery, were detected to have had LAM injury: 35 unilateral (20 right, 15 left) and 13 bilateral. The mean LUG at the central three slides on TUI described above for those with right LAM injury was 26.64 (3.47) mm and left LAM injury 28.97 (3.95) mm. No LAM injury was found in the CS group. At 12 months, 38 women (79.2 %), all diagnosed with LAM injury at 8 weeks after delivery, were detected to have persistent LAM injury: 28 were unilateral (16 right, 12 left) and 10 were bilateral. The mean LUG at 12 months for those with right or left LAM injury was 25.62 (2.97) mm and 28.32 (3.71) mm respectively. There was a tendency toward a larger mean LUG at 8 weeks for those with persistent LAM injury compared with those with LAM injury not found at 12 months (LUG of persistent LAM injury 27.93 [4.3] mm vs LAM not detected 26.24 [2.3] mm, P = 0.27), but this did not reach statistical significance. Figure 1 showed right LAM injury detected in a woman at 8 weeks after delivery, but the injury was not found at 12 months.
Overall, 134 and 48 women (53.2% and 19.0 % respectively) practiced pelvic floor exercise at 8 weeks and 12 months respectively. There was no difference in the proportion of women practicing pelvic floor exercise between those with and those without LAM injury.
Table 1 showed the relationship between POP-Q findings and LAM injury at both 8 weeks and 12 months after delivery. More women had descent of the bladder neck (POP-Q Aa) at both 8 weeks and 12 months after delivery in the LAM injury group. Although there was a tendency toward more descent of the cervix and posterior compartment in the LAM injury group at both time points, this was not statistically significant.
Table 2 compared the positions of pelvic organs in the LAM injury group and the group without the injury at 8 weeks and 12 months. There was a tendency for the bladder neck, cervix and ano-rectal junction to be more distal (closer to the symphysis pubis) at rest, Valsalva and pelvic floor muscle contraction in the LAM injury group; however, statistical significance was rarely reached. The hiatal area was significantly larger in the LAM injury group.
Table 3 showed the relationship between the symptoms of pelvic floor disorder and LAM injury at both 8 weeks and 12 months after delivery. We were unable to confirm an association between SUI, UUI, mixed UI, FI and LAM injury at both time points. Significantly more women reported prolapse symptoms in the LAM injury group at 8 weeks. Fewer women reported the prolapse symptoms at 12 months and there was no statistical difference between the two groups by 12 months after delivery. The association between persistent LAM injury at 12 months and SUI, UUI, mixed UI, FI and prolapse symptoms was not confirmed.
At 8 weeks after vaginal delivery, there was a tendency toward higher PFDI scoring on all subscales in women with LAM injury compared with those without the injury. However, this only reached statistical significance on the General subscale of Pelvic Organ Prolapse Distress Inventory (POPDI; LAM injury group 16.37 [16.55] vs no LAM injury group 10.53 [12.86], P = 0.026) and Urinary Distress Inventory Obstructive subscale scoring (LAM injury group 8.05 [10.07] vs no LAM injury group 5.02 [7.30], P = 0.036). The subscale scores of PFIQ between the two groups were similar. By 12 months after delivery, there was no observed difference in any of the subscales of the PFDI and PFIQ, although there remained a higher general score in POPDI in women with LAM injury (LAM injury group 16.42 [17.34] vs no LAM injury group 14.62 [21.90], P = 0.27). There was no observed difference in PFDI and PFIQ subscale scores between the group with unilateral LAM injury and those with bilateral LAM injury, both at 8 weeks and at 12 months.
Discussion
The reported prevalence of LAM injury after vaginal delivery varies between 13 and 36 % [1, 2, 4]. Our finding was 19.0 % (95 % CI, 14.2–23.8 %). The difference in the rate of instrumental delivery, especially forceps delivery, may affect the prevalence of LAM injury [2, 3, 6]. Another possible reason could be the difference in the timing of detecting LAM injury. The reports have been time sensitive. In general, the earlier the assessment was done after delivery, the higher the incidence reported [2, 4, 6].
“Healing” or recovery of LAM injury has been reported [23–25]. By transperineal ultrasound assessment, Shek et al. reported that 2 out of 12 women (16.7 %) in whom LAM injury was detected at 3–6 months after delivery experienced improvement of the levator trauma when reassessed at 2–3 years [23]. Staer-Jensen et al. also reported that 7 out of 29 women (24.1 %) had partial recovery or complete recovery of LAM injury at 6 months after delivery [25]. Branham et al. found, using MRI assessment, that 31 % of the primiparous women who had the injury found at 6 weeks had recovered by 6 months after delivery by MRI assessment [24]. We found that 10 women (20.8 %) who had LAM injury at 8 weeks after delivery had no injury detected at 12 months. This was similar to Shek’s and Staer-Jensen’s findings (P = 1.0 and P = 0.74 respectively, results not shown above), but was lower than Branham’s finding. That may be due to a very high prevalence of LAM abnormality, 49 %, detected by Branham et al. at 6 weeks after delivery and the use of different assessment methods. In our study, the LUG at 8 weeks after delivery in the women with the injury not detected at 12 months, had a tendency to be smaller compared with those who had persistent injury at 12 months. This correlated with the findings that women with a larger injury involving more muscle did not recover compared with those with a smaller injury who tended to have normal findings later [24]. Currently, there are limited reports on the “healing” of LAM injury and we are not able to suggest a hypothesis for this observation. Only with a larger population of LAM injury and a longer follow-up may we understand more in this field. Apart from the LAM injury, we have found that by 12 months after the delivery, the pelvic floor partially “recovered” after pregnancy and childbirth. For example, the bladder neck descended during pregnancy, but returned to a more proximal position at 12 months after delivery, although it remained at a significantly lower position compared with its position in the first trimester [14, 22].
The presence of LAM injury increased the hiatal area of the women at rest, at Valsalva and at pelvic floor muscle contraction. We have previously identified that the presence of LAM injury increased the risk of women having irreversible hiatal over-distension [14], which was defined as an increase of more than 20 % in hiatal area after delivery compared with findings during pregnancy [2]. This was consistent with the findings of Shek et al. [2].
There was limited information on the effect of LAM injury on the health-related quality of life of women shortly after delivery. LAM injury was associated with prolapse symptoms at 8 weeks after delivery in our study. This is consistent with the finding that more women in the LAM injury group had bladder neck and anterior compartment descent at 8 weeks. This was compatible with a tendency toward the bladder neck and cervix being more distal in the LAM injury group, although we are not able to demonstrate statistical significance. This finding was also compatible with a higher POPDI general subscale score, meaning more severe symptoms scores in the LAM injury group at 8 weeks. It is worthwhile noting that the overall PFDI, including the POPDI general subscale score and the UDI obstructive subscale score, even in women with LAM injury in this study, were much lower than in another cohort of Chinese women with a stage I/II pelvic organ prolapse (POPDI general score of 34.7 [24.2] and a UDI obstructive score of 24.7 [20.4]) [26]. The higher POPDI general subscale scores in current study could also be due to a higher hiatal area in women with avulsion [6, 14]. However, there was no difference in terms of the impact on their quality of life, as reviewed by PFIQ scores, including the POPIQ at 8 weeks after delivery. Generally, the hiatal area at Valsalva and pelvic floor muscle contraction was significantly smaller at 12 months after delivery, both after vaginal delivery and after Caesarean section, compared with the findings at 8 weeks [14]. The absolute difference in hiatal area was small. These may be some of the explanations for the lack of observed difference in POP symptoms, POPDI scores or POPIQ at 12 months between the groups with and without LAM injury. However, more studies are needed to explore this.
There is ample evidence that childbirth or LAM injury is an important contributing factor for pelvic floor disorders [7, 8, 13, 27, 28]. However, although 26 %, 8 %, 4 % and 8 % of women reported SUI, UUI, FI and POP symptoms respectively at 1 year after delivery, we were not able to confirm that LAM injury was related to these symptoms of pelvic floor disorder by 12 months after delivery. This suggested that other factors might contribute to the onset of symptoms. We previously reported that antenatal SUI (odds ratio [OR] 2.8) and antenatal UUI (OR 2.4) were factors associated with postpartum SUI; antenatal UUI (OR 6.4) and a higher maternal body mass index at first trimester (OR 1.2) were associated with postpartum UUI and antenatal FI was associated with postnatal FI (OR 6.1) [13]. Throughout the antenatal period, at least up to 36–38 weeks of pregnancy, no LAM injury was detected [3]. Other pelvic floor changes or injuries, e.g., bladder neck mobility, hiatal area and concomitant external anal sphincter injury may be other contributing factors for the symptoms of pelvic floor disorders [8, 22, 29]. The impact of LAM injury on the pelvic floor is also likely to emerge later in life as other factors, such as age itself, exert their influence. Recently, in a group of women with confirmed LAM injury, Thomas et al. reported that the mean latency between the first vaginal delivery and the presentation of pelvic organ prolapse was 34.3 years (range 3–66.3 years) [30]. From our study, there is good evidence that the pelvic floor recovers to some extent after childbirth in the majority of women in the short term.
Although this was a prospective longitudinal study, the follow-up remained short. Further longer term study is required to fully explore the effect of LAM injury on women and whether further pregnancy, childbirth and aging may aggravate the injury and symptoms of pelvic floor disorders. In order to detect the differences between symptoms of pelvic floor disorder and the impact on the quality of life of women, a larger sample is also needed. Another limitation was that the strength of Valsalva and pelvic floor muscle contraction could not be standardised during the USG. However, as all the women have been assessed since the first trimester, they have been taught Valsalva and pelvic floor muscle contraction many times, and they could all perform this properly. The USG volume with the best Valsalva and pelvic floor muscle contraction at 12 months was used for each woman.
In conclusion, 79 % of women who had LAM injury at 8 weeks after vaginal delivery had persistent LAM injury at 12 months. LAM injury was associated with symptoms of prolapse, a more severe decrease in POP-Q Aa and Ba points at 8 weeks after delivery and higher Pelvic Organ Prolapse Distress Inventory and Urinary Distress Inventory Obstructive subscale scores. However, it was not associated with prolapse symptoms or PFDI scores at 12 months after delivery, nor was it associated with SUI, UUI, mixed UI, or FI at 8 weeks or 12 months after delivery.
Abbreviations
- FI:
-
Faecal incontinence to solid/liquid stool
- LAM:
-
Levator ani muscle
- LUG:
-
Levator–urethral gap
- PFDI:
-
Pelvic Floor Distress Inventory
- PFIQ:
-
Pelvic Floor Impact Questionnaire
- POPDI:
-
Pelvic Organ Prolapse Distress Inventory
- POP-Q:
-
Pelvic Organ Prolapse Quantification
- SUI:
-
Stress urinary incontinence
- UDI:
-
Urinary Distress Inventory
- USG:
-
Ultrasound
- UI:
-
Urinary incontinence
- UUI:
-
Urge urinary incontinence
References
Dietz HP, Lanzarone V (2005) Levator trauma after vaginal delivery. Obstet Gynecol 106:707–712
Shek K, Dietz H (2010) Intrapartum risk factors for levator trauma. BJOG 117:1485–1492
Chan SS, Cheung RY, Yiu AK, Lee LL, Pang AW, Choy KW, Leung TY, Chung TK (2012) Prevalence of levator ani muscle injury in Chinese primiparous women after first delivery. Ultrasound Obstet Gynecol 39:704–709
Dlouha K, Krofta L, Krcmar M, Feyereisl J (2013) Prevalence and trends of symptomatic pelvic floor disorders before and six weeks after the first delivery—longitudinal study. Neurourol Urodynamic 32(6):616
Kearney R, Miller JM, Ashton-Miller JA, DeLancey JOL (2006) Obstetrical factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol 107:144–149
Cassado Garriga J, Pessarrodona Isern A, Espuna Pons M, Duran Retamal M, Felgueroso Fabrega A, Rodriguez Carballeira M, Jorda Santamaria I (2011) Four-dimensional sonographic evaluation of avulsion of the levator ani according to delivery mode. Ultrasound Obstet Gynecol 38:701–706
Dietz HP, Simpson JM (2008) Levator trauma is associated with pelvic organ prolapse. BJOG 115:979–984
Shek KL, Pirpiris A, Dietz HP (2010) Does levator avulsion increase urethral mobility. Eur J Obstet Gynecol Reprod Biol 153:215–219
Schwertner-Tiepelmann N, Thakar R, Sultan AH, Tunn R (2012) Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol 39:372–383
Morgan DM, Cardoza P, Guire K, Fenner DE, DeLancey JO (2010) Levator ani defect status and lower urinary tract symptoms in women with pelvic organ prolapse. Int Urogynecol J 21:47–52
Howard D, DeLancey JO, Tunn R, Ashton Miller JA (2000) Racial differences in the structure and function of the stress urinary continence mechanism. Obstet Gynecol 95:713–717
Dietz HP (2003) Do Asian women have less pelvic organ mobility than Caucasians? Int Urogynecol J Pelvic Floor Dysfunct 14:250–253
Chan SS, Cheung RY, Yiu KW, Lee LL, Chung TKH (2013) Prevalence of urinary and fecal incontinence in Chinese women during and after first pregnancy. Int Urogynecol J 24:1473–1479
Chan SS, Cheung RY, Yiu KW, Lee LL, Chung TK (2013) Pelvic floor biometry of Chinese primiparous women one year after delivery and the relationship with obstetric factors: a prospective observational study. Ultrasound Obstet Gynecol. doi:10.1002/uog.13249
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecologic Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Chan SS, Cheung RY, Yiu AK, Li JC, Lai BP, Choy KW, Chung TK (2011) Chinese validation of Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ). Int Urogynecol J 22:1305–1312
Chan SS, Cheung RY, Lai BP, Lee LL, Choy KW, Chung TK (2013) Responsiveness of the Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaire in women undergoing treatment for pelvic floor disorders. Int Urogynecol J 24:213–221
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Dietz HP (2010) Pelvic floor ultrasound: a review. Am J Obstet Gynecol 202:321–334
Dietz H, Abbu A, Shek K (2008) The levator urethral gap measurement: a more objective means of determining levator avulsion? Ultrasound Obstet Gynecol 32:941–945
Zhuang RR, Song YF, Chen ZQ, Ma M, Huang HJ, Chen JH, Li YM (2011) Levator avulsion using a tomographic ultrasound and magnetic resonance-based model. Am J Obstet Gynecol 205:232.e1–232.e8
Chan SS, Cheung RY, Yiu KW, Lee LL, Leung TY, Chung TK (2014) Pelvic floor biometry during first singleton pregnancy and the relationship with pelvic floor disorders symptoms: a prospective observational study. BJOG 121:121–129
Shek KL, Chantarasorn V, Langer S, Dietz HP (2012) Does levator trauma ‘heal’? Ultrasound Obstet Gynecol 40:570–575
Branham VG, Thomas J, Jaffe TA, Crockett MM, South MMT, Jamison MG, Weidner AC (2007) Levator ani abnormality six weeks after delivery persists at six months. Am J Obstet Gynecol 197:65
Staer-Jensen J, Siafarikas F, Hilde G, Bo K, Ellstrom Engh M (2013) Do major defects of the levator ani muscle heal within the first 6 months postpartum? Neurourol Urodynamic 32:650–651
Chan SS, Cheung RY, Yiu AK, Lee LL, Pang AW, Chung TK (2012) Symptoms, quality of life and factors affecting women’s treatment decision on pelvic organ prolapse. Int Urogynecol J 23:1027–1033
Glazener C, Herbison G, MacArthur C, Lancashire R, McGee M, Grant A, Wilson P (2006) New postnatal urinary incontinence: obstetric and other risk factors in primiparae. BJOG 113:208–217
Solans-Domenech M, Sanchez E, Espuna-Pons M, Pelvic Floor Research Group (2010) Urinary and anal incontinence during pregnancy and postpartum. Obstet Gynecol 115:618–628
Heibrun ME, Nygaard IE, Lockhart ME, Richter HE, Brown MB, Kenton KS, Rahn DD, Thomas JV, Weidner AC, Nager CW, Delancey JO (2010) Correlation between levator ani muscle injuries on magnetic resonance imaging and fecal incontinence, pelvic organ prolapse, and urinary incontinence in primiparous women. Am J Obstet Gynecol 202:488.e1–488.e6
Thomas V, Shek K, Guzman Rojas R, Dietz H (2013) The latency between pelvic floor trauma and presentation for prolapse surgery. Ultrasound Obstet Gynecol 42(S1):39
Acknowledgement
This study obtained a grant from the Health and Health Services Research Fund from the Food and Health Bureau of Hong Kong SAR.
Financial disclaimer/conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chan, S.S.C., Cheung, R.Y.K., Yiu, K.W. et al. Effect of levator ani muscle injury on primiparous women during the first year after childbirth. Int Urogynecol J 25, 1381–1388 (2014). https://doi.org/10.1007/s00192-014-2340-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2340-y