Abstract
Introduction and hypothesis
This study reports long-term outcomes of the transvaginal tension-free vaginal tape–obturator (TVT-O) procedure for treating stress urinary incontinence (SUI), including possible risk factors for failure.
Methods
This was a retrospective study of women who underwent TVT-O with or without concomitant prolapse surgery. Procedures were performed at a tertiary referral urogynecology unit. Participants presented with SUI and had urodynamic stress incontinence (USI). Women with a history of previous anti-incontinence procedures, radical pelvic surgery, and detrusor overactivity (DO) were excluded. Objective cure was defined as absence of urine leakage during a cough stress test (CST). Subjective outcome was based on the International Consultation on Incontinence Questionnaire for Evaluating Female Lower Urinary Tract Symptoms (ICIQ-FLUTS). Quality of life was assessed using the King’s Health Questionnaire (KHQ). Univariate and multivariate analyses were used to identify risk factors for subjective failure.
Results
One hundred twenty-four consecutive women were assessed, with a median follow-up of 90.3 (range 80–103) months. Overall objective and subjective cure rates were 81.5 % (101/124) and 83.5 % (103/124), respectively. A significant improvement was observed in all KHQ domains. Concomitant vaginal hysterectomy [odds ratio (OR) = 2.98, 95 % confidence interval (CI) 1.10–8.05, p = 0.03] and increasing point C (OR = 1.17, 95 % CI 1.05–1.30, p = 0.006] were associated with a higher risk for subjective failure. De novo urgency rate was 7 %.
Conclusions
The TVT-O procedure provides high objective and subjective long-term efficacy, a clinically meaningful improvement in patient quality of life, and an excellent safety profile. Concomitant vaginal hysterectomy and apical compartment prolapse were associated with a higher risk for objective and subjective failure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) represents the most common type of involuntary urine loss, affecting up to 20 % of women worldwide [1]. This percentage is estimated to grow as life expectancy of women in the developed world increases. Although SUI is considered a benign situation, symptoms impact social, physical, and psychological well-being of affected women, with associated low self-esteem and social isolation [2]. Several surgical procedures, both vaginal and abdominal, have been proposed over the years for treating SUI. Current evidence suggests that midurethral slings (MUS), such as the retropubic tension-free vaginal tape (TVT) and the transvaginal tension-free vaginal tape–obturator, or transobturator tape (TVT-O, TOT) have become the treatment of choice and are considered the gold standard [3, 4]. Transobturator slings were shown to have comparable short-term cure rates with the retropubic approach, carrying a decreased risk of bladder, bowel, and vascular injury [5]. Until now, TVT has been the only MUS with reports on long-term cure rates at a maximum follow-up of 17 years [3, 6]. The few published studies assessing medium- to long-term outcomes of the TVT-O procedure reach a maximum follow-up period of 5 years [7–10]. It therefore becomes necessary to provide outcomes that include data on long-term efficacy and complications related either to the surgical technique itself or to the mesh material.
The primary aim of this study was to determine long-term objective and subjective cure rates of the TVT-O procedure in treating SUI and to identify any risk factors for failure. Secondary outcome measures were the effects of TVT-O on health-related quality of life and perioperative and long-term postoperative complications.
Materials and methods
This retrospective study assessed 145 consecutive women who underwent a TVT-O procedure (Gynecare Worldwide, Inc. Johnson & Johnson) with or without a concomitant pelvic floor reconstructive surgery between January 2004 and June 2006. All surgical procedures were performed or supervised by a urogynecologist at a tertiary referral urogynecology unit. Ethical approval and consent for this study was obtained by the Institutional Review Board. All participants presented complaining predominantly of SUI symptoms and had urodynamic stress incontinence (USI) on urodynamics (UDS). Women with a history of previous anti-incontinence procedures, radical pelvic surgery, and detrusor overactivity (DO) on UDS were excluded from the study.
Preoperatively, all women completed the International Consultation on Incontinence Questionnaire for Evaluating Female Lower Urinary Tract Symptoms (ICIQ-FLUTS) [11, 12] and the King’s Health Questionnaire (KHQ) [13]. Additional assessment included a comprehensive medical history, clinical examination, urinalysis, and multichannel UDS. The degree of prolapse was graded using the Pelvic Organ Prolapse Quantification (POP-Q) system [14].
TVT-O placement was performed as originally described by de Leval [15], with minor modifications. The needles were inserted at the level of the midurethra and after passing through the obturator membrane were directed 1 cm medially rather than 2 cm laterally in relation to the genitofemoral fold. Routine cystoscopy was performed to detect any bladder or urethral injuries. Traditional anterior and posterior pelvic floor repairs (PFR) and/or vaginal hysterectomy (VH) with suspension of the vault to the uterosacral ligament (USL) were performed in women with symptomatic pelvic organ prolapse (POP). Women with vaginal-vault prolapse underwent laparoscopic sacrocolpopexy (SCP). The TVT-O was placed after completion of prolapse surgery. All vaginal procedures were carried out under epidural anesthesia. Intraoperative and perioperative complications were retrieved from patients’ medical notes.
Patients meeting the inclusion criteria were contacted and asked to attend a follow-up visit between September 2012 and February 2013. This assessment included completion of both ICIQ-FLUTS and KHQ, a cough stress test (CST) performed in a semilithotomy position with a comfortably filled bladder (approximately 300 ml), and a gynecological examination focused on detecting any local mesh-related complications. Women were specifically asked to report any postoperative voiding difficulties needing tape division. Lastly, patients were asked whether they had any postoperative groin pain on the day of the follow-up visit. Their responses were documented as “yes” or “no” in a standardized fashion.
Objective cure was defined as the absence of urine leakage during the CST. Subjective outcome was based on the ICIQ-FLUTS. Subjective cure was defined when patients responded “never” in the question: “Does urine leak when you are physically active, exert yourself, cough, or sneeze?” A lower score from that given preoperatively was considered as a subjective improvement. Women who underwent a second anti-incontinence procedure within the follow-up period were considered as objective and subjective failures. Quality of life improvement was indicated by a decrease in KHQ domain scores. The minimal important clinical difference (MICD) (the smallest change in score that patients perceive as beneficial) was set at −5 points for each KHQ domain [16]. De novo urgency and any change in the degree of urgency symptoms were assessed by the ICIQ-FLUTS question: “Do you have to rush to the toilet to urinate?”.
Statistical analysis
Descriptive statistics of data are presented as means ± standard deviation (SD), medians [quartiles (Q1, Q3)], or percentages for normally and nonnormally distributed continuous variables or categorical variables, respectively; proportions were compared using the z test, and comparisons for continuous variables between before and after surgery results were done using the t test for paired data or Wilcoxon signed-rank test. To find independent factors associated with subjective failure, univariate and stepwise multivariate logistic regression analysis (p value for removal was set at 0.1 and for entry at 0.05) was performed. Adjusted OR with 95 % CI was computed from results of logistic regression analyses. All statistical tests were two sided. Stata 11.0 software was used for all statistical analyses (Stata Corp., College Station, TX, USA).
Results
Overall, 124/145 (85.5 %) women were available for the follow-up visit; 18 (12.4 %) were not able to be contacted based on personal contact data provided, and three (2.1 %) women had died of reasons unrelated to the surgery. Demographic characteristics of the study population are presented in Table 1. Median follow-up was 90.3 (range 80–103) months.
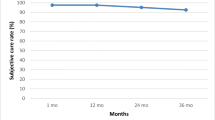
Overall objective and subjective cure rates were 81.5 % (101/124) and 83.1 % (103/124), respectively; 3.2 % (4/124) of patients were subjectively improved, and 13.7 % (17/124) reported no improvement or worsening of the SUI symptoms. Three women (2.4 %) underwent a second anti-incontinence procedure (TVT) 1–3 years after the primary surgery and were considered as objective and subjective failures. Objective and subjective results of women undergoing different types of surgery are presented in Table 2.
Univariate analysis (Table 3) showed that advancing age (p = 0.047) and concomitant VH (p = 0.02) were factors associated with increased risk for subjective failure. Moreover, women with higher preoperative values of points Aa (p = 0.048), Ba (p = 0.027) ,and C (p = 0.008) appeared to have greater odds for subjective failure. However, multivariate analysis showed that concomitant VH and increasing value of preoperative point C were the only statistically significant factors for subjective failure. According to these results, women who underwent a concomitant VH had almost three times greater likelihood of belonging in the subjective failure group (OR = 2.98, 95 % CI = 1.10–8.05, p = 0.03); increase in the degree apical compartment (point C) prolapse was statistically correlated with higher risk for subjective failure (OR = 1.17, 95 % CI = 1.05–1.30, p = 0.006). Lastly, concomitant VH was the only statistically significant prognostic factor for objective failure in univariate analysis (OR = 4.39, 95 % CI = 1.04–18.54, p = 0.044): therefore, no multivariate analysis was performed.
KHQ data analysis showed a statistically significant improvement in all domains. Furthermore, in terms of clinically relevant improvement, the difference between mean postoperative and preoperative values was over the MICD (Table 4).
There were no major perioperative complications, such as bladder perforations, vessel injuries, and obturator hematomas. One patient (0.8 %) reported postoperative voiding difficulties that required tape division 3 months after surgery. Another patient (0.8 %) reported the presence of vaginal erosion diagnosed 1 year after the procedure; it was situated on the midurethral midline, and a large part of the tape was excised. At the follow-up visit, no cases of vaginal erosions were detected. Assessment of postoperative urgency symptoms revealed that 76.3 % (29/38) of patients with preoperative urgency symptoms reported an improvement at the time of the visit; 15.8 % (6/38) reported no change, and 7.9 % (3/38) reported aggravation of the pre-existing urgency. De novo urgency was reported in 7 % (6/86) of the patients; all women with de novo urgency and women with persistent SUI were scheduled for further investigation and management. No patient reported persistent groin pain at the long-term follow-up.
Discussion
Since its introduction, the TVT-O procedure has become increasingly popular for surgical management of SUI due to equivalent short-term success rates and lower perioperative morbidity compared with retropubic approaches [6–10, 17]. However, the efficacy of a surgical procedure aiming to be considered as a old standard should also be tested in terms of long-term durability, patient satisfaction, and impact of the procedure on the patient’s quality of life [18]. This study reports the 7-year objective and subjective cure rates of TVT-O, representing the longest follow-up thus far reported in the literature. Overall objective and subjective cure rates (81.5 % and 83.1 %, respectively) are in agreement with other studies presenting medium- to long-term follow-up results [7–10]. Serati et al. [7] reported a 5-year follow-up with objective and subjective cure rates of 90.8 % and 90.3 %, respectively. The slightly higher cure rates could be attributed to the fact that the abovementioned study evaluates only women with pure SUI, excluding patients with overactive bladder (OAB) symptoms and/or POP. This is a highly homogeneous study population but far removed from daily practice, as the concomitant occurrence of POP and SUI is more than common [18, 19]. Similar 5-year results were presented by Cheng and Liu [8], who reported objective and subjective cure rates of 87.4 % and 90 %, respectively, in a population without significant POP. Groutz et al. [9] reported a 5-year cure rate of 74 % in a group of 61 women, but patients with preoperative DO were not excluded from the study. Lastly, Angioli et al. [10] reported objective and subjective cure rates of 73 % and 62 %, respectively; it was a small sample-size study (n = 31), and no validated questionnaire was used to assess subjective outcomes.
Our results show that increasing point C and concomitant VH were independent risk factors for a higher long-term subjective failure rate. Findings from the Norwegian National Database for Incontinence Surgery [20] showed that SUI cure was lower in women who had TVT combined with prolapse surgery compared with women having only TVT. This is consistent with the study by Matthew et al. [21], who demonstrated an increased risk for recurrent SUI in women who underwent concurrent surgery for POP. On the contrary, several studies [4, 17] report that combined prolapse and incontinence surgery provides excellent results, similar to cure rates achieved with placement of slings only; however, Richter et al. [22] found that concomitant POP surgery is not associated with overall failure but does decrease the odds of objective compared with subjective failure by nearly 50 %. We hypothesize that the risk factors for higher subjective failure observed in our study could be attributed to various parameters related to either surgical technique or differences in SUI pathophysiology. A subtle distortion of the local anatomy due to VH and vault suspension might influence optimal sling positioning and tensioning. Additionally, minor posthysterectomy neurophysiologic damage or even scarring of the vaginal wall might influence long-term local dynamics of the urethral sphincter mechanism. It has also been shown that hysterectomy itself may alter the local neural network and circulation [23]. Finally, Veronikis et al. [24] proposed that in patients with severe POP, urethral kinking at the level of the bladder neck or even more distally may decrease arterial blood flow, causing urethral muscle ischemia. Additionally, traction by the unreduced genital prolapse may add a stretch injury to the urethra, further compromising its innervation. In their study, 56 % of patients with severe prolapse had low urethral closure pressures, which could predispose to a high risk of postoperative failure with standard incontinence operations [25, 26]. Future prospective trials such as the Multicenter Randomized Controlled Trials to Assess the Value of Combining Prolapse Surgery and Incontinence Surgery in Patients with Genital Prolapse and Evident Stress Incontinence (CUPIDO-I) could possibly clarify optimal management for these higher-risk patients [27].
Health-related quality of life is considered an essential endpoint of surgical procedures treating benign conditions such as SUI [13]. Our data show a statistically significant improvement in all KHQ domain scores. Moreover, assessment of the difference between preoperative and postoperative mean values show a small clinical effect in the General Health Perceptions domain and a more significant treatment benefit in all other condition-specific domains. These findings, combined with the fact that this change was greater than MICD, confirm that this type of surgery leads to a meaningful improvement in patients’ quality of life.
An important aspect of this study is that it provides information about potential late complications that may be related either to the mesh material or to the surgical procedures undertaken. In our study, perioperative and long-term postoperative morbidity associated with the TVT-O procedure were uncommon. The most prevalent complication was the development of de novo urgency (7 %), although some of those women could have naturally developed age-related urgency symptoms. Few data are available assessing the relationship between TVT-O and long-term de novo urgency. Serati et al. [7] observed that de novo OAB symptoms were reported by 19.5 % of patients at the 5-year follow-up visit. This is considered rather high, even though the authors did not clarify the methodology used to diagnose OAB symptoms postoperatively. Our results were similar with those reported by Angioli et al. [10], who found a 5-year de novo urgency rate of 6.4 %.
Groin pain may occur after transobturator procedures but mostly settles within the first month following surgery [28]. Persistent groin pain can be present in up to 3.8 % of patients [8]. At follow-up, no patient reported persistent groin pain, and this could be attributed to the slightly modified surgical technique. Obviously, this is only a hypothesis and thus needs to be tested in prospective randomized trials.
Managing recurrent or persistent SUI after TVT-O placement represents a critical dilemma for clinicians. Current evidence suggests that either subsequent placement of a TVT without removing the TVT-O sling [29] or suburethral mesh readjustment [30] represent two simple and safe minimally invasive procedures that have high success rates.
We acknowledge that the major limitation of our study is its retrospective nature. Most patients were external referrals and had their postoperative follow-up in their local health authority; therefore, no valid intermediate outcomes could be included. However, our results reflect patients’ clinical condition 7 years after surgery. The study population represents 85.5 % of the initial pool of patients, and one could argue that this may introduce an important selection bias. Nevertheless, the 12.4 % of women excluded were undetectable based on personal contact data provided prior to surgery and therefore cannot be considered as failures. Finally, including patients with POP who underwent concomitant PFR increased the heterogeneity of the study population. However, the group is representative of patients seen in our daily clinical practice and more than likely in other urogynecological units. The results of other studies assessing long-term efficacy of MUS in patients without POP cannot be extrapolated directly to patients with concomitant POP. Our study adds valuable information for preoperative counseling of women opting to undergo a TVT-O with concomitant PFR surgery. Conversely, points of strength of this study are the large number of patients and the use of validated tools for assessing objective and subjective outcomes.
In conclusion, this study reports the long-term TVT-O outcomes using a retrospective design in a real-life cohort. It shows that the TVT-O procedure provides high long-term efficacy, clinically meaningful improvement in patients’ quality of life, and an excellent safety profile. However, women with central compartment prolapse and those undergoing concomitant VH had a higher risk of subjective failure. These results could therefore be useful to clinicians for preoperative consultation of patients with SUI.
Abbreviations
- SUI:
-
Stress urinary incontinence
- MUS:
-
Midurethral slings
- USI:
-
Urodynamic stress incontinence
- UDS:
-
Urodynamics
- DO:
-
Detrusor overactivity
- ICIQ-FLUTS:
-
International Consultation on Incontinence Questionnaire for Evaluating Female Lower Urinary Tract Symptoms
- KHQ:
-
King’s Health Questionnaire
- POP-Q:
-
Pelvic Organ Prolapse Quantification
- PFR:
-
Anterior and posterior pelvic floor repairs
- VH:
-
Vaginal hysterectomy
- SCP:
-
Laparoscopic sacrocolpopexy
- POP:
-
Pelvic organ prolapse
- CST:
-
Cough stress test
- MICD:
-
Minimal important clinical difference
- OAB:
-
Overactive bladder
- USL:
-
Uterosacral ligament
References
Hunskaar S, Lose G, Sykes D, Voss S (2004) The prevalence of urinary incontinence in woman in four European countries. BJU Int 93:324–330
Fultz NH, Burgio K, Diokno AC, Kinchen KS, Obenchain R, Bump RC (2003) Burden of stress urinary incontinence for community-dwelling women. Am J Obstet Gynecol 189:1275–1282
Nilsson CG, Palva K, Aarnio R, Morcos E, Falconer C (2013) Seventeen years’ follow-up of the tension-free vaginal tape procedure for female stress urinary incontinence. Int Urogynecol J [Epub ahead of print]
Serati M, Salvatore S, Uccella S, Artibani W, Novara G, Cardozo L, Bolis P (2009) Surgical treatment for female stress urinary incontinence: what is the gold-standard procedure? Int Urogynecol J Pelvic Floor Dysfunct 20:619–621. doi:10.1007/s00192-009-0850-9
Latthe PM, Foon R, Toozs-Hobson P (2007) Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG 114:522–531
Serati M, Ghezzi F, Cattoni E, Braga A, Siesto G, Torella M, Cromi A, Vitobello D (2012) Salvatore S (2012) Tension-free vaginal tape for the treatment of urodynamic stress incontinence: efficacy and adverse effects at 10-year follow-up. Eur Urol 61:939–946. doi:10.1016/j.eururo.2012.01.038
Serati M, Bauer R, Cornu JN, Cattoni E, Braga A, Siesto G, Lizée D, Haab F, Torella M, Salvatore S (2012) TVT-O for the Treatment of Pure Urodynamic Stress Incontinence: Efficacy, Adverse Effects, and Prognostic Factors at 5-Year Follow-up. Eur Urol doi:10.1016/j.eururo.2012.12.022
Cheng D, Liu C (2012) Tension-free vaginal tape-obturator in the treatment of stress urinary incontinence: a prospective study with five-year follow-up. Eur J Obstet Gynecol Reprod Biol 161:228–231. doi:10.1016/j.ejogrb.2012.01.011
Groutz A, Rosen G, Gold R, Lessing JB, Gordon D (2011) Long-term outcome results of the inside-out transobturator tension-free vaginal tape: efficacy and risk factors for surgical failure. J Womens Health (Larchmt) 20:1525–1528. doi:10.1089/jwh.2011
Angioli R, Plotti F, Muzii L, Montera R, Benedetti Panici P, Zullo MA (2010) Tension-free vaginal tape versus transobturator suburethral tape: five-year follow-up results of a prospective, randomised trial. Eur Urol 58:671–677. doi:10.1016/j.eururo.2010.08.004
Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P (2004) A scored form of the bristol female lower urinary tract symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol 191:73–82
Athanasiou S, Grigoriadis T, Kyriakidou N, Giannoulis G, Antsaklis A (2012) The validation of international consultation on incontinence questionnaires in the Greek language. Neurourol Urodyn 31:1141–1144. doi:10.1002/nau.22197
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S (1997) A new questionnaire to assess the quality of life of urinary incontinent women. Br Obstet Gynecol 104:1374–1379
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
de Leval J (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44:724–730
Kelleher CJ, Pleil AM, Pr R, Burgess SM, Brodish PH (2004) How much is enough and who says so? BJOG 111:605–612. doi:10.1111/j.14710528.004.00129.x
Tommaselli GA, D’Afiero A, Di Carlo C, Formisano C, Fabozzi A, Nappi C (2012) Efficacy of a modified technique for TVT-O positioning: a twelve-month, randomized, single-blind, multicenter, non-inferiority study. Eur J Obstet Gynecol Reprod Biol doi:10.1016/j.ejogrb.2012.11.014.
Waltregny D (2013) TVT-O: A New Gold Standard Surgical Treatment of Female Stress Urinary Incontinence? Eur Urol doi:10.1016/j.eururo.2013.01.017
Bai SW, Jeon MJ, Kim JY, Chung KA, Kim SK, Park KH (2002) Relationship between stress urinary incontinence and pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 13:256–260
Kulseng-Hanssen S, Borstad E (2002) Comparison of subjective and objective outcome values and complication rate after TVT operations exclusively and TVT operation and vaginal repair for prolapse combined. IUGA. Int Urogynecol J Pelvic Floor Dysfunct 13:S33
Barber MD, Kleeman S, Karram MM, Paraiso MF, Ellerkmann M, Vasavada S, Walters MD (2008) Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. Am J Obstet Gynecol 199(666):e1–e7. doi:10.1016/j.ajog.2008.07.050
Richter HE, Litman HJ, Lukacz ES, Sirls LT, Rickey L, Norton P, Lemack GE, Kraus S, Moalli P, Fitzgerald MP, Dandreo KJ, Huang L, Kusek JW, Network UIT (2011) Demographic and clinical predictors of treatment failure one year after midurethral sling surgery. Obstet Gynecol 117:913–921. doi:10.1097/AOG.0b013e31820f3892
Bai SW, Kang SH, Kim SK, Kim JY, Park KH (2003) The effect of pelvic organ prolapse on lower urinary tract function. Yonsei Med J 44:94–98
Veronikis DK, Nichols DH, Wakamatsu MM (1997) The incidence of low-pressure urethra as a function of prolapse-reducing technique in patients with massive pelvic organ prolapse (maximum descent at all vaginal sites). Am J Obstet Gynecol 177:1305–1313
Sand PK, Bowen LW, Panganiban R, Ostergard DR (1987) The low pressure urethra as a factor in failed retropubic urethropexy. Obstet Gynecol 69:399–402
McGuire EJ (1981) Urodynamic findings in patients after failure of stress incontinence operations. Prog Clin Biol Res 78:351–360
van der Steen A, van der Ploeg M, Dijkgraaf MG, van der Vaart H, Roovers JP (2010) Protocol for the CUPIDO trials; multicenter randomized controlled trials to assess the value of combining prolapse surgery and incontinence surgery in patients with genital prolapse and evident stress incontinence (CUPIDO I) and in patients with genital prolapse and occult stress incontinence (CUPIDO II). BMC Womens Health 10:16. doi:10.1186/1472-6874-10-16
Meschia M, Bertozzi R, Pifarotti P, Baccichet R, Bernasconi F, Guercio E, Magatti F, Minini G (2007) Peri-operative morbidity and early results of a randomised trial comparing TVT and TVT-O. Int Urogynecol J Pelvic Floor Dysfunct 18:1257–1261
Moore RD, Gamble K, Miklos JR (2007) Tension-free vaginal tape sling for recurrent stress incontinence after transobturator tape sling failure. Int Urogynecol J Pelvic Floor Dysfunct 18:309–313
de Landsheere L, Lucot JP, Foidart JM, Cosson M (2010) Management of recurrent or persistent stress urinary incontinence after TVT-O by mesh readjustment. Int Urogynecol J 21:1347–1351. doi:10.1007/s00192-010-1200-7
Conflict of interest
Stavros Athanasiou has received travel expenses from Johnson & Johnson.
Themos Grigoriadis has received travel expenses from Johnson & Johnson.
Dimitrios Zacharakis: None
Nikolaos Skampardonis: None
Dionysia Lourantou: None
Aris Antsaklis: None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Athanasiou, S., Grigoriadis, T., Zacharakis, D. et al. Seven years of objective and subjective outcomes of transobturator (TVT-O) vaginal tape: Why do tapes fail?. Int Urogynecol J 25, 219–225 (2014). https://doi.org/10.1007/s00192-013-2186-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2186-8