Abstract
Introduction and hypothesis
Midurethral slings (MUS) are the gold standard primary procedure for the surgical treatment of stress urinary incontinence (SUI). There is no robust evidence on the success with MUS in the treatment of recurrent SUI. Our objective was to evaluate the effectiveness and complications of MUS in women with recurrent SUI by systematic review and meta-analysis of the literature.
Methods
A systematic literature search was carried out (up to August 2011) using relevant search terms in MEDLINE, EMBASE, CENTRAL and Google Scholar. Relevant randomised controlled trials (RCT) and prospective studies were selected and then analysed by two independent reviewers. Meta-analysis of cure stated in prospective cohort studies was performed with a random effects model using Stata 8.
Results
There was 1 randomised trial and 11 good quality prospective studies included in this systematic review. The overall subjective cure rate per meta-analysis of prospective cohort studies following MUS for recurrent SUI after any previous surgery was found to be 78.5 % [95 % confidence interval (CI) 69–88] at the follow-up of 29.72 ± 29.49 months. The subjective cure rate following MUS after previous failed MUS was 73.3 % (95 % CI 55–97) at the follow-up of 15.7 ± 7.7 months.
Conclusions
The studies report good cure rates of SUI after MUS surgery following previous incontinence surgery (62–100 %). There seems to be a lower cure rate with transobturator compared to the retropubic tape for recurrent SUI after previous surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) is estimated to affect 50 % of women presenting with urinary incontinence (UI) [1]. Patients with SUI are treated with conservative measures such as pelvic floor exercises initially. Those who do not respond to conservative measures are offered surgery. Midurethral slings (MUS) are the primary gold standard procedure for treating SUI with long-term cure rates of 77–90 % [2]. Recurrent SUI after failed incontinence surgery is a challenging problem.
The reoperation rate for incontinence within 5 years following surgery for prolapse and incontinence has been reported to be 8 % [3]. There is no consensus on the procedure of choice for treating recurrent SUI. There are variable data available regarding the cure rate of SUI with MUS after persistence or recurrence of SUI following previous surgery. We aimed to evaluate the effectiveness of MUS in women with persistent or recurrent SUI after previous surgery. We also wanted to study the complication rates following repeat surgery.
Methods
Sources
All prospective studies describing effectiveness of MUS in women with recurrent SUI were included in this review. They were identified by searching the MEDLINE, EMBASE, CINAHL, CENTRAL (The Cochrane Library, Issue 2, 2009), National Library for Health, metaRegister of Controlled Trials and Google Scholar (up to August 2011). The conference proceedings and abstracts from the International Continence Society and the International Urogynecological Association annual meetings for the last 3 years were also searched. The following keywords were used for the search as text word or subject headings without language restriction: ‘stress urinary incontinence, midurethral sling, tension-free tape, transobturator tape and recurrent stress urinary incontinence’. Hand searches of the bibliographies and citation list of all relevant articles were also carried out. The first or corresponding authors of included trials were contacted for additional information if necessary. No ethical approval was sought for this study, as it was a systematic review and meta-analysis of published manuscripts.
Study selection
Randomised controlled trials (RCTs) and prospective studies of women who underwent retropubic and transobturator vaginal tapes [TVT, outside in transobturator tape (TOT), inside out transobturator tape (TVT-O)] for recurrent SUI following previous surgeries were included. Two reviewers (AP and PJ) independently selected the articles for inclusion by assessing the eligibility of full papers against the review inclusion criteria, with disagreements resolved by discussion, if necessary, with a third reviewer (PL) per a priori protocol. In cases of duplication, the study that reported most recent data was included.
-
Participants: women with recurrent SUI following failed stress continence surgery
-
Intervention: synthetic MUS TVT/ TOT/TVT-O
-
Outcome measures: subjective/objective cure/improvement
Data extraction and quality assessment
Two independent reviewers (AP and PJ) extracted data for quality and results independently. Data included characteristics of participants, intervention, comparisons if any, outcome assessment tools and results of the studies. The Jadad score was used to assess quality of RCT and the Newcastle-Ottawa Scale was used for the prospective cohort studies.
Statistical analysis
Regression rates from individual prospective studies were meta-analysed using a random effects model. Statistical analysis was performed using Stata 8.0 (StataCorp, College Station, TX, USA).
Results
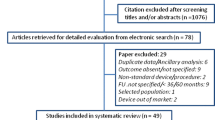
We included 12 studies in total; Fig. 1 summarises the flow for study selection in this systematic review. There was 1 RCT [4] and 11 prospective studies [5–15] with a total of 430 participants between 23 and 87 years of age (see Table 1 for details of included studies). There were nine non-comparative studies, eight of which described effectiveness of TVT and one used TOT (see Table 1). Three comparative studies that described comparison between different sling procedures in the management of recurrent SUI included TVT vs TOT [8], TVT-O vs TOT [4] and TVT vs TOT vs intravaginal sling (IVS) [14]. The interval between primary and repeat surgery ranged from 6 weeks to 48 months. Previous surgery included Burch colposuspension, Kelly plication, Marshall-Marchetti-Krantz procedure (MMK), Stamey needle suspension, Pereyra’s operation, MUS, conventional slings and paraurethral collagen injection in eight studies[4–11], while four studies [12–15] included women with previous failed MUS only.
Methodological quality
For the RCT, the Jadad score was 3, randomisation was done using opaque sealed envelope and follow-up was adequate. Power calculation was done and blinding was described.
The quality of the non-randomised prospective studies is shown in Fig. 2. The recruitment was consecutive in two studies [5, 9]. The diagnosis was ascertained both clinically and urodynamically in ten studies, and clinically [with urodynamics (UDS) if history not suggestive] in one study [9]. The instruments used to assess outcomes were satisfactorily described in ten studies. The outcome was assessed as overall cure in the majority of studies [5–10, 14, 15], while subjective and objective components were assessed separately in some studies [4, 11–13]. The follow-up was described in all of them and ranged from 1 month to 12 years and it was adequate (>80 %) in all 11 studies.
Outcomes
The studies used different parameters for subjective/objective cure and improvement. Subjective parameters used were bladder diary, patient satisfaction, subjective symptoms analysis, quality of life (QOL) evaluation, King’s Health Questionnaire (KHQ), Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12), Patient Global Impression of Improvement (PGI-I), International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF), Incontinence Severity Index (ISI), Urogenital Distress Inventory (UDI), Incontinence Impact Questionnaire (IIQ), Urinary Incontinence Severity Score (UISS), visual analogue scale (VAS) and absence of complaint of leakage.
The objective outcomes measured in these studies were UDS, cough stress test and pad test (which included 1-h pad test <2 g/h, <1 g/h, 24-h pad test <10 g/24 h).
Criteria used for improvement were 1-h pad test < 5 g, 24-h pad test showed >80 % reduction in leakage, reduction in urine leakage to less than 50 % and QOL improvement >75 % but less than <90 %.
Overall subjective cure
On meta-analysis the subjective cure rate following MUS for recurrent SUI after any previous surgery was found to be 78.5 % [95 % confidence interval (CI) 69–88] at the follow-up of 29.72 ± 29.49 months (Fig. 3).
There were four studies looking at cure rate of MUS after previous MUS surgery for SUI [12–15]. The subjective cure rate was 73.3 % (95 % CI 55–97) at 15.7 ± 7.7 months follow-up (Fig. 4).
Outcome after TVT
The subjective cure rate following retropubic MUS (TVT) was 79.8 % (95 % CI 71–89) at a follow-up of 27.26 ± 26.85 months (Fig. 5). There were ten studies looking at outcome after retropubic MUS following any previous failed incontinence surgery. Three of these ten studies looked at outcome with repeat retropubic MUS after previous failed MUS [13–15]. Seven of these ten studies had a success rate of over 80 %. One study reported a cure rate of 61 % and two others had a cure rate ≥ 70 %.
Outcome after TOT
There were four studies looking at outcome after TOT following any previous surgery and the collated subjective cure was 54 % (Fig. 6). Two of these four looked at outcome of repeat TOT after previous failed MUS [12, 14]. The highest cure rate reported after TOT was 66.7 % (95 % CI 25–100) [8]. One study had a cure rate of 33.3 % [14] and the other two studies had cure rates of 52.6 % [12] and 55.6 % [4].
Complications
In this systematic review, there were 28 urinary tract injuries during 363 retropubic sling procedures (7.7 %) during repeat continence surgery. This compares favourably with a previous systematic review showing bladder injury in 10 of 238 procedures (4.2 %) during primary retropubic sling procedures [16]. The incidence of de novo urgency was 5.5–20 %. Voiding dysfunction was found in 4–16 % and urinary tract infection in 5.9–13 %. Excess bleeding (1.7–6.7 %) and urinary retention needing loosening of tape (9 %) were the other complications seen in some studies [7, 9, 13].
Discussion
The studies report good cure rates for recurrent SUI with MUS following previous failed incontinence surgery (62–100 %). There seems to be a lower cure rate with TOT (33–67 %) compared to the retropubic tape (61–100 %) for recurrent SUI after previous surgery for this condition. The rate of urinary tract injuries is around 7.7 % with retropubic slings.
The search was thorough and not restricted by language. The manuscript adheres to the 27-item PRISMA checklist [17]. The latest joint International Urogynecological Association/International Continence Society terminology for female pelvic floor dysfunction was used [18]. The definition of cure varied between studies and this can also account for the variable success rates described. The drawbacks of this piece of work are not weaknesses of the systematic review itself but the dearth of primary RCTs in this area. The long-term success of MUS has been reported between 78.9 and 84.7 % [19, 20]. The common reason for failure of initial sling is either anatomical or functional [21]. A correctly placed MUS mimics the effect of the pubourethral ligament. [22].
Repeat continence surgery is often difficult as a result of scarring and adhesions with the distortion in anatomy from previous surgeries, thereby increasing intraoperative complications [5]. Retropubic MUS has a good success rate after any type of previous surgery for SUI including previous MUS surgery with bladder perforation rates quoted between 2.9 and 19 %. Our view is that, as long as bladder perforation is recognised and the tape is repositioned, it may not have long-term implications. A retropubic approach is preferred over a transobturator approach for repeat surgery [12]. The axis of the transobturator is less acute to the urethral axis as compared to the retropubic route, thereby creating a platform sling with less circumferential compression of the urethra [23]. Another reason could be the need for wider dissection of the periurethral area with the transobturator approach resulting in migration of the tape [24].
The retropubic sling has been used successfully to treat recurrent SUI due to intrinsic sphincter deficiency (ISD) [15]. The rationale proposed for this is the greater acute angle which may be more obstructive than the transobturator and, therefore, more successful in treating incontinence due to ISD. The main mechanism of MUS relies on dynamic kinking of the proximal urethra and compression of the midurethra at the level of the sling. This procedure requires adequate mobility of the urethra. The success rate of repeat surgery was 90 % in women with sufficient preoperative mobility of the urethra, while it was only 33 % in women with a fixed urethra [7].
It would be ideal to collect data on repeat surgery on failed incontinence surgery prospectively via national databases (e.g. British Society of Urogynaecology, BSUG in the UK) to build up a further evidence base and perform individual patient data meta-analysis.
Abbreviations
- MUS:
-
Midurethral sling
- SUI:
-
Stress urinary incontinence
- TVT:
-
Tension-free vaginal tape
- TOT:
-
Transobturator tape
- KHQ:
-
King’s Health Questionnaire
- PISQ-12:
-
Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire
- PGI-I:
-
Patient Global Impression of Improvement
- ICIQ-SF:
-
International Consultation on Incontinence Questionnaire-Short Form
- ISI:
-
Incontinence Severity Index
- MMK:
-
Marshall-Marchetti-Krantz procedure
- DIS:
-
Detrusor instability score
- VAS:
-
Visual analogue scale
- UDI:
-
Urogenital Distress Inventory
- IIQ:
-
Incontinence Impact Questionnaire
- UISS:
-
Urinary Incontinence Severity Score
- VLPP:
-
Valsalva leak point pressure
- MUCP:
-
Mean urethral closure pressure
- ICIQ:
-
International Consultation on Incontinence Questionnaire
- PVR:
-
Post-void residual
- ISD:
-
Intrinsic sphincter deficiency
- UDS:
-
Urodynamics
- UPP:
-
Urethral pressure profilometry
References
Hunskaar S, Burgio K (2005) Epidemiology of urinary and faecal incontinence and POP. In: Abrams P, Cardozo L (eds) 3rd international consultation on incontinence. [Web page]:255–312
Nilsson CG, Palva K, Rezapour M, Falconer C (2008) Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 19(8):1043–1047
Clark AL, Gregory T, Smith VJ, Edwards R (2003) Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 189(5):1261–1267
Abdel-Fattah M, Ramsay I, Pringle S, Hardwick C, Ali H, Young D et al (2011) Evaluation of transobturator tension-free vaginal tapes in management of women with recurrent stress urinary incontinence. Urology 77(5):1070–1075
Rezapour M, Ulmsten U (2001) Tension-free vaginal tape (TVT) in women with recurrent stress urinary incontinence–a long-term follow up. Int Urogynecol J Pelvic Floor Dysfunct 12(Suppl 2):S9–S11
Lo TS, Horng SG, Chang CL, Huang HJ, Tseng LH, Liang CC (2002) Tension-free vaginal tape procedure after previous failure in incontinence surgery. Urology 60(1):57–61
Liapis A, Bakas P, Lazaris D, Creatsas G (2004) Tension-free vaginal tape in the management of recurrent stress incontinence. Arch Gynecol Obstet 269(3):205–207
Sivaslioglu AA, Unlubilgin E, Keskin HL, Gelisen O, Dolen I (2011) The management of recurrent cases after the Burch colposuspension: 7 years experience. Arch Gynecol Obstet 283(4):787–790
Ala-Nissilä S, Haarala M, Mäkinen J (2010) Tension-free vaginal tape - a suitable procedure for patients with recurrent stress urinary incontinence. Acta Obstet Gynecol Scand 89(2):210–216
Azam U, Frazer MI, Kozman EL, Ward K, Hilton P, Rane A (2001) The tension-free vaginal tape procedure in women with previous failed stress incontinence surgery. J Urol 166(2):554–556
Kuuva N, Nilsson CG (2003) Tension-free vaginal tape procedure: an effective minimally invasive operation for the treatment of recurrent stress urinary incontinence? Gynecol Obstet Invest 56(2):93–98
Van Baelen AA, Delaere KP (2009) Repeat transobturator tape after failed mid-urethral sling procedure: follow-up with questionnaire-based assessment. Urol Int 83(4):399–403
Liapis A, Bakas P, Creatsas G (2009) Tension-free vaginal tape in the management of recurrent urodynamic stress incontinence after previous failed midurethral tape. Eur Urol 55(6):1450–1455
Tsivian A, Neuman M, Yulish E, Shtricker A, Levin S, Cytron S et al (2007) Redo midurethral synthetic sling for female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18(1):23–26
Moore RD, Gamble K, Miklos JR (2007) Tension-free vaginal tape sling for recurrent stress incontinence after transobturator tape sling failure. Int Urogynecol J Pelvic Floor Dysfunct 18(3):309–313
Latthe PM, Foon R, Toozs-Hobson P (2007) Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG 114(5):522–531
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21(1):5–26
Nilsson C, Kuuva N, Falconer C, Rezapour M, Ulmsten U (2001) Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 12(Suppl 2):S5–S8
Tsivian A, Mogutin B, Kessler O, Korczak D, Levin S, Sidi A (2004) Tension-free vaginal tape procedure for the treatment of female stress urinary incontinence: long-term results. J Urol 172:998–1000
Penson D, Raz S (1996) In: Raz S, Raz S (eds) Why anti-incontinence surgery succeeds or fails. Saunders, Philadelphia
Petros P (2007) The female pelvic floor. Function, dysfunction and management according to the integral theory. Springer, Berlin, pp 174–180
Whiteside J, Walters M (2004) Anatomy of the transobturator region: relations to a trans-obturator sling. Int Urogynecol J Pelvic Floor Dysfunct 15:223–226
Lee K, Doo C, Han D, Jung B, Han J, Choo M (2007) Outcomes following repeat mid urethral synthetic sling after failure of the initial sling procedure: rediscovery of the tension-free vaginal tape procedure. J Urol 178:1370–1374
Acknowledgments
Dr. Ioannis Gallos for his help with Stata analysis.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pradhan, A., Jain, P. & Latthe, P.M. Effectiveness of midurethral slings in recurrent stress urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J 23, 831–841 (2012). https://doi.org/10.1007/s00192-012-1803-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1803-2