Abstract
Introduction and hypothesis
The purpose of this observational study was to examine the effect of periurethral injections with polyacrylamide hydrogel (PAHG) on quality of life (QoL) in selected patients with stress urinary incontinence (SUI).
Methods
Fifty-four women with comorbidities or other reasons precluding other surgery received PAHG for SUI. Patient-reported outcomes were assessed with the “Incontinence Outcome Questionnaire” (IOQ) 9 months postoperatively. The IOQ is a 27-item, condition-specific instrument that assesses patient-reported outcomes after incontinence surgery.
Results
Forty-two women (78%) completed the questionnaire. Responses ranged from considerable (40%) and slight improvement (21%) to no change (29%) and worsening of symptoms (10%).
Conclusion
Periurethral injections with PAHG are likely to provide relief of symptoms and improvement in QoL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence occurs in about 10% of nulliparous and between 16% and 21% of parous women [1] and negatively impacts on quality of life (QoL) [2, 3]. The severity of symptoms as well as age and comorbidities influences treatment decisions [2–5]. While surgical options such as midurethral tapes have high success rates [6], they do have complications, and not all patients are good candidates for surgery. Conservative methods such as pelvic floor muscle training require a minimum of physical fitness and good patient participation [5].
Periurethral injections of bulking agents are minimally invasive and can be performed with local anesthesia on an outpatient basis [7–13]. Injections of bulking agents into the urethral wall create artificial urethral cushions that can improve continence. Injection therapy may also work by augmenting the power of the urethral sphincter [14]. A Cochrane review of 12 randomized trials of periurethral injection therapies found that bulking agents have a better safety profile than open surgery but show inferior results at 12 months. The authors conclude that injection therapy cannot be recommended for women fit for other surgical procedures but may be a useful option for relief of symptoms for women with substantial comorbidities [7].
A number of materials have been used for periurethral bulking, and a number of them have been abandoned because of problems [7, 8]. The ideal bulking agent should be non-immunogenic, biocompatible, durable, and of sufficient size to prevent migration.
Polyacrylamide hydrogel (PAHG) (Bulkamid®, Contura, Denmark and Ethicon Women’s Health and Urology) is one of the more recent agents to be studied. PAHG is a homogeneous, non-absorbable, stable, and nonbiodegradable watery gel consisting of 2.5% cross-linked polyacrylamide and 97.5% nonpyrogenic water. The gel is biocompatible and also used in plastic and esthetic surgery [11].
The purpose of this observational study was to evaluate the procedure and to examine the effect of periurethral injections with PAHG on QoL in patients with primary or recurrent stress urinary incontinence (SUI). Most of our patients had comorbidities, previous surgery for incontinence, or both. We hypothesized that the majority of treated women would benefit from the procedure.
Materials and methods
The initial study population consisted of 54 consecutive women who received periurethral injections with PAHG for SUI between December 2005 and September 2009 at our institution. Patients were treated with PAHG because of comorbidities and/or previous surgery for incontinence or genital cancer (Table 1). Decisions regarding treatment were made on the basis of clinical findings, history, overall health status, and patient preference. The procedure was done with mild sedation and local anesthesia. One to two milliliters of PAHG was injected transurethrally into the submucosa at the 3, 6, and 9 o’clock positions with a specially designed 0° urethroscope.
Before intervention, a urogynecologic history and detailed clinical examination were done. Urodynamic evaluation was not performed in all patients. Patient satisfaction and impact on QoL were assessed with the “Incontinence Outcome Questionnaire” (IOQ) [15]. Nine months after the procedure, all treated women were sent the IOQ by mail and asked to complete and return it in a prepaid envelope.
The IOQ is a 27-item, condition-specific instrument to assess patient-reported outcomes in women after surgery for SUI [15]. It contains 27 questions related to symptoms, complications, QoL and satisfaction, problems with urinary incontinence before surgery, and demographic and treatment-related information. The IOQ consists of one multi-item subscale with 15 items, six single questions, and six nonscoring questions. For all scores, high values indicate poorer outcomes and lower values indicate better outcomes. The IOQ is an instrument for one-point assessment after treatment, and no pretreatment data needs to be collected. It was psychometrically evaluated in patients with SUI who underwent tension-free tape (TVT) operation and completed a 3-month follow-up [15]. Inclusion criteria for this population had been no prior urogynecologic surgery and overall good health status.
Descriptive statistics were used to present IOQ results and sociodemographic and clinical data. The t test for independent samples was used to compare continuous IOQ variables between the study population and the reference population. Significance level was determined at 0.05. The Bonferroni correction for multiple testing was applied, which resulted in a critical p value of 0.002.
Results
The clinical characteristics and relevant histories of the 54 women who underwent periurethral injection with PAHG are shown in Table 1. The majority of patients had substantial comorbidities and/or a history of gynecologic surgery for malignant or benign conditions. Twenty-four women (44%) had undergone surgery for urinary incontinence. The median age was 69 years (range 41–87), and the median parity was three (range 0–6). Forty-one patients (76%) had severe SUI, 13 patients (24%) had moderate SUI, and 18 patients (33%) additionally had urge symptoms. Because of comorbidity, age, and geographic reasons, most women stayed in the hospital overnight.
Postoperative urinary retention occurred in five patients (9%), two of them required temporary suprapubic catheterization. There was one incident of temporary paraurethral hematoma in a woman with oral anticoagulation. Thirteen women (24%) underwent a second and one (2%) a third periurethral injection; the median time between PAHG injections was 9 months (range 1–17).
The results of the IOQ (Table 2) are based on the 42 women (78%) who completed and returned the questionnaire. Thirteen women (31%) were living alone and 29 (69%) with partner and/or other family members. There were no differences between respondents and nonrespondents in sociodemographic and clinical variables. Mean time between injection and completion of the questionnaire was 9 ± 5 months. The mean value for the multi-item scale QoL/satisfaction indicates an average improvement in various aspects of QoL and satisfaction with the procedure. The high standard deviations of this and most other questions reflect the wide variety in patients’ perceptions and responses, which ranged from complete cure and full satisfaction to worsening of symptoms and QoL. Thirty-one women (74%) stated that they would recommend the procedure to others. Seventeen women (40%) reported a considerable improvement and nine women (21%) a slight improvement of symptoms; 12 women (29%) considered them unchanged and four women (10%) reported a worsening of symptoms. Overall, 43% of women diagnosed with mixed incontinence and 71% of women with pure SUI reported improvement of symptoms. Patients with recurrent SUI were more likely to have noticed improvement (66% versus 58%) and had better scores for QoL (30.9 versus 37.4) compared to patients with no prior incontinence therapy.
Discussion
This study reviews our experience with a series of patients with complicated SUI treated with periurethral injection. PAHG was chosen as bulking agent mostly because of its favorable safety profile and ease of use. The majority of women in our series reported improvement in QoL and reduction of SUI symptoms, but over a third reported no change or even worsening of symptoms. Women with complaints of OAB showed distinctly lower subjective improvement and satisfaction rates. This is consistent with the findings of Lose et al. who reported a subjective success rate of 70% in women with pure SUI and 50% in women with mixed incontinence after periurethral injection with PAHG [11].
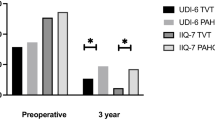
Comparison between our IOQ QoL results and previously reported QoL results after TVT operation [15, 17] showed poorer outcomes in our study group. This finding is in line with the results of two previous studies comparing periurethral injection therapy with other surgical managements. Corcos et al. found that open surgery was more effective than collagen injection 12 months after the intervention in terms of 24-h pad tests [12]. Maher et al. compared transurethral polydimethylsiloxane with pubovaginal sling and described a significant advantage in objective cure with pubovaginal sling at 6 months [13].
Our results support the conclusion of the Cochrane review that bulking agents should not be used for women fit for other surgical options [7]. Periurethral-injection-related complications in our series were minor (temporary retention and hematoma) and occurred in 11%. This confirms that periurethral injections are generally safe [7–13] and have fewer complications than midurethral slings [6]. However, 9 months after the procedure, 33% of women who received PAHG reported subjective voiding difficulties. In our series, 26% of women had repeated periurethral injections due to primary persistence of incontinence or diminished effect over time. Similar reinjection rates have been reported in other series and with other materials [7, 10, 11].
Several bulking agents have been associated with the development of urethral granuloma, abscess, and cysts, and their clinical use has been stopped [4, 7, 8]. No such complications have been reported after periurethral injection of PAHG. However, bony erosions and facial ulcers after use of PAHG in facial augmentation have been described [16].
This study has several limitations. No objective outcome parameters were examined. Due to the mostly impaired health status of this patient group, we refrained from asking for a return visit and clinical check-up. Furthermore, we believe that in this selected patient group changes in urodynamic data are less meaningful than changes in QoL. High correlation between QoL and SUI symptoms has been described before [2–4, 15, 17]. However, results of some single items may be influenced by comorbidities.
The modest number of patients in our study limits the comparability and generalisability of the results but does reflect that periurethral injections were used for a selected group only. The women in our sample were on average 9 years older and had more comorbidities than most women receiving TVT operations [6, 17]. The mean follow-up was 9 months, so that we cannot draw conclusions about long-term effects. Also, we did not address costs.
Overall, we conclude that periurethral injections with PAHG can alleviate symptoms and improve QoL in women with SUI. A less beneficial effect can be expected in women with mixed incontinence. The effect of the procedure seems inferior to TVT operation and may be temporary, and need for reinjection is common. The limited morbidity of the procedure is an option for women with comorbidities precluding other treatment options.
References
Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S, Norwegian EPINCONT Study (2003) Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med 348:900–907
Tennstedt SL, FitzGerald MP, Nager C, Xu Y, Zimmern P, Kraus S, for the Urinary Incontinence Treatment Network et al (2007) Quality of life in women with stress urinary incontinence. Int Urogynecol J 18:543–549
Gil KM, Somerville AM, Cichowski S, Savitski JL (2009) Distress and quality of life characteristics associated with seeking surgical treatment for stress urinary incontinence. Health Qual Life Outcomes 7:8
Chapple CR, Brubaker L, Haab F, van Kerrebroeck P, Robinson D (2007) Patient-perceived outcomes in the treatment of stress urinary incontinence: focus on urethral injection therapy. Int Urogynecol J 18:199–205
Shamliyan TA, Kane RL, Wyman J, Wilt TJ (2008) Systematic review: randomized, controlled trials of nonsurgical treatments for urinary incontinence in women. Ann Intern Med 148:459–473
Tamussino K, Hanzal E, Kolle D, Ralph G, Riss P (2001) Tension-free vaginal tape operation: results of the Austrian registry. Obstet Gynecol 98:732–736
Keegan PE, Atiemo K, Cody J, McClinton S, Pickard R (2007) Periurethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev 3:CD003881
Kotb AF, Campeau L, Corcos J (2009) Urethral bulking agents: techniques and outcomes. Curr Urol Rep 10:396–400
Schulz JA, Nager CW, Stanton SL, Baessler K (2003) Bulking agents for stress urinary incontinence: short-term results and complications in a randomized comparison of periurethral and transurethral injections. Int Urogynecol J 15:261–265
Tamanini JT, D’Ancona CAL, Tadini V, Netto NR (2003) Macroplastique implantation system for the treatment of female stress urinary incontinence. J Urol 169:2229–2233
Lose G, Mouritsen L, Nielsen JB (2006) A new bulking agent (polyacrylamide hydrogel) for treating stress urinary incontinence in women. BJU Int 98:100–104
Corcos J, Collet JP, Shapiro S, Herschorn S, Radomski SB, Schick E et al (2005) Multicenter randomized clinical trial comparing surgery and collagen injections for treatment of female stress urinary incontinence. Urology 65:898–904
Maher CF, O'Reilly BA, Dwyer PL, Carey MP, Cornish A, Schluter P (2005) Pubovaginal sling versus transurethral Macroplastique for stress urinary incontinence and intrinsic sphincter deficiency: a prospective randomised controlled trial. BJOG 112:797–801
Klarskov N, Lose G (2008) Urethral injection therapy: what is the mechanism of action? Neurourol Urodyn 27:789–792
Bjelic-Radisic V, Dorfer M, Tamussino K, Frudinger A, Kern P, Winter R et al (2007) The Incontinence Outcome Questionnaire: an instrument for assessing patient-reported outcomes after surgery for stress urinary incontinence. Int Urogynecol J 18:1139–1149
Liu HL, Cheung WY (2010) Complications of polyacrylamide hydrogel (PAAG) injection in facial augmentation. J Plast Reconstr Aesthet Surg 63:e9–e12
Bjelic-Radisic V, Dorfer M, Greimel E, Frudinger A, Tamussino K, Winter R (2006) Quality of life and continence 1 year after the tension-free vaginal tape operation. Am J Obstet Gynecol 195:1784–1788
Acknowledgement
We thank Fedor Daghofer, Ph.D., for the statistical analysis.
Conflicts of interest
Dr. Tamussino has served as a consultant for Contura and Ethicon Women’s Health and Urology. The other authors have no disclosures. No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trutnovsky, G., Tamussino, K., Greimel, E. et al. Quality of life after periurethral injection with polyacrylamide hydrogel for stress urinary incontinence. Int Urogynecol J 22, 353–356 (2011). https://doi.org/10.1007/s00192-010-1296-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1296-9