Abstract
Introduction and hypothesis
The aim of the study was to evaluate the clinical and functional outcomes of laparoscopic sacrocolpopexy, in particular its effect on female sexual function.
Methods
A retrospective observational study of women undergoing laparoscopic sacrocolpopexy between February 2005 and March 2009 was undertaken. Pelvic organ support was assessed objectively using the pelvic organ prolapse quantification scale (POP-Q). Functional outcomes were assessed using the International Consultation on Incontinence questionnaire for vaginal symptoms (ICIQ-VS), both preoperatively and at 6–36 months postoperatively.
Results
Eighty-four women with a mean age of 65 years (range, 49–78 years) were studied. At follow-up in clinic, all women had good vault support (mean point C, −8.9; range, 10 to −8). Subjective improvements in prolapse symptoms and sexual well-being were observed with significant reductions in the respective questionnaire scores.
Conclusions
Our results confirm previous findings that laparoscopic sacrocolpopexy is a safe and efficacious surgical treatment for post-hysterectomy vaginal vault prolapse. It provides excellent apical support and good functional outcome with overall improvement in sexual function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of symptomatic vault descent following hysterectomy is unknown; however, it has been estimated to affect 0.2–43% [1–3] of hysterectomised women. Vaginal pessaries are commonly used as a first-line conservative treatment for symptomatic prolapse; however, long-term pessary use has a high discontinuation rate. Only 14% of patients continue to use pessaries over the long-term [4].
Numerous surgical procedures have been described for the management of vault prolapse and few have been subject to rigorous assessment of their anatomical and functional outcome. Consequently, the optimal surgical approach remains controversial. Abdominal sacrocolpopexy is well described in the literature, with reported success rates in the range of 78–100% [3, 5, 6]. When compared with vaginal sacrospinous fixation, sacrocolpopexy has been shown to have a lower rate of recurrence, less postoperative dyspareunia and a lower re-operation rate [6–8]; however, the procedure takes longer to perform and has a longer recovery time.
Laparoscopic sacrocolpopexy has evolved from classical abdominal sacrocolpopexy and provides the potential to combine the success rate of an abdominal approach with the faster recovery time associated with a minimally invasive technique. Tissue dissection and mesh placement are facilitated by magnification of the operating field. The success rate of laparoscopic sacrocolpopexy has been reported to be 90–98% [9–13]; however, most of the published studies are retrospective and mainly describe objective anatomical and surgical outcomes. There are limited data in the literature on subjective functional results. One study by North et al. [14] involved 22 women with the results of laparoscopic sacrocolpopexy evaluated prospectively using the pelvic organ prolapse quantification (POP-Q) system [15] together with the assessment of functional outcome using a validated questionnaire.
We report here the results of a retrospective observational study on 84 patients who underwent laparoscopic sacrocolpopexy. The aim of the study was to evaluate the clinical outcomes, surgical morbidity and functional outcomes of laparoscopic sacrocolpopexy, in particular its effect on female sexual function, using the International Consultation on Incontinence questionnaire for vaginal symptoms (ICIQ-VS) [16].
Materials and methods
Patient selection
The investigation was conducted as a retrospective observational study (clinical audit) at a tertiary referral urogynaecology unit in the UK and involved 84 consecutive women with post-hysterectomy vaginal vault prolapse who underwent laparoscopic sacrocolpopexy between February 2005 and March 2009.
Prolapse assessment: preoperative
Subjective assessment of the prolapse symptoms and their impacts (degree of bother), as well as related sexual matters, was conducted using the validated vaginal symptoms questionnaire, ICIQ-VS.
Objective clinical assessment of the pelvic organ prolapse was performed during a Valsalva manoeuvre, in the left lateral position, utilising a Sims' speculum. The POP-Q scale was used to grade the degree of prolapse at all sites. Where indicated, urodynamic studies were also performed.
Operative details and peri-operative complication data were collected. Parameters recorded included age, previous pelvic surgery, concomitant surgical procedure, conversion to laparotomy or vaginal procedure, operating time, occurrence and timing of any complication, estimated blood loss and duration of hospital stay.
Prolapse assessment: postoperative
Each woman was followed up in clinic 3 months later and was reassessed for pelvic organ prolapse using the POP-Q scale. The primary measure for successful objective outcome was the absence of vaginal vault prolapse, postoperatively. Surgical cure of the vaginal vault prolapse was defined as point C being higher than one half of the total vaginal length and no need for re-operation or pessary use for a symptomatic apical failure. We also recorded the presence or absence of prolapse in any other compartment. The ICIQ-VS questionnaire was then sent by post to each patient 6–36 months after surgery to evaluate the functional outcome of the laparoscopic sacrocolpopexy.
Surgical technique
Surgery was performed by the senior author or under his direct supervision. After skin preparation, draping and catheterisation, a Deaver retractor was inserted into the vagina. A pneumoperitoneum was created and four laparoscopic ports were placed, 11-mm umbilical and suprapubic ports and two 5-mm lateral ports. The peritoneum over the sacral promontory was incised with bipolar graspers and monopolar scissors. The ureters were identified bilaterally and a peritoneal relaxing incision was made medial to the right ureter and lateral to the rectum. A type-1 lightweight polypropylene monofilament macroporous non-absorbable mesh was used in every case. Following dissection of the rectovaginal space to the level of the levator ani muscles, a mesh was placed along the full length of the posterior vaginal wall. The mesh was then sutured in place along the posterior vaginal wall and vault using 10–12 sutures. If a significant cystocoele was also present, the bladder was dissected from the upper half of the anterior vaginal wall and a mesh was placed anteriorly. The cranial aspect of the mesh was secured to the sacral promontory with 5-mm tacks (ProTack; Tyco Healthcare, Norwalk, CT, USA). Complete peritonisation of the mesh was achieved by opposing the edges of peritoneum with interrupted absorbable 2.0 polyglactin sutures (Monocryl, Ethicon/Johnson & Johnson, UK).
Our surgical technique for laparoscopic sacrocolpopexy evolved during the study. Initially, we inserted the mesh along the full length of the posterior vaginal wall with low dissection down to the level of the perineal body. Although vault support was satisfactory in all cases, in some early procedures low mesh placement at sacrocolpopexy failed to address any concurrent deficiency of the perineal body; some women then required further vaginal surgery at a later date. To correct this problem, we amended the technique by first placing the mesh along the posterior vaginal wall laparoscopically and then performing a concomitant repair of the deficient perineal body vaginally. The choice of suture material was also modified. Initially, non-dissolvable polyester 2.0 sutures (Ethibond, Ethicon Inc., Somerville, NJ, USA) were used to secure the mesh to the vaginal wall; however, after observing several cases of vaginal suture erosion requiring removal of the Ethibond sutures, we changed to slowly dissolvable polydioxanone monofilament 2.0 sutures (PDS, Ethicon/Johnson & Johnson, UK), which loses its tensile strength at 3 months and is completely absorbed by 6 months.
Additional procedures such as posterior colpoperineorrhaphy, anterior colporrhaphy, paravaginal repair, surgery for stress urinary incontinence or ventral rectopexy, were performed concomitantly when clinically indicated. Patients received a single prophylactic dose of antibiotics (intravenous Co-amoxiclav 1.2 g unless contraindicated).
Results
Eighty-four women with a mean age of 65 years (range, 49–78 years) were studied. The number of previous procedures ranged from zero to five, with 67 women (80%) having had at least one previous prolapse repair procedure, including vaginal hysterectomy, anterior and/or posterior colporrhaphy, colposuspension or vaginal sacrospinous ligament fixation. Forty-nine women (58%) had previously undergone vaginal hysterectomy and 35 (42%), abdominal hysterectomy. Preoperatively, all women had a significant vault descent of greater than or equal to stage 2, as measured on the POP-Q system. Thirty-six women (43%) had a stage 2 vault prolapse, 42 women (50%) had a stage 3 prolapse and the remaining six (8%) had a stage 4 prolapse.
Sixty-eight women (81%) had concomitant procedures performed at the same time as the laparoscopic sacrocolpopexy (Table 1).
The mean duration of the sacrocolpopexy operation was 64 min (range, 50–95 min), measuring from the first knife incision and excluding the time required to perform any concomitant procedures. All 84 procedures were completed laparoscopically. In 16 women out of 84 (19%), a mesh was placed over the upper half of the anterior vaginal wall to correct the cystocele as well as posteriorly.
There were two intraoperative bladder injuries that occurred during dissection of the bladder from the vaginal vault. These were repaired laparoscopically and the sacrocolpopexy procedure was then completed. The bladder injuries subsequently healed without any long-term sequelae. Immediate postoperative complications included urinary tract infection (5%) and voiding dysfunction (3%). The mean estimated blood loss was 75 ml (range, 50–250 ml) and no patient required a peri-operative blood transfusion. The mean duration of postoperative inpatient stay was 2.5 nights (range, one to five nights).
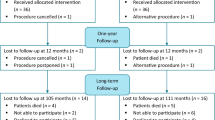
All 84 women were available for follow-up in clinic at 3 months and 56 completed the ICIQ-VS questionnaire at 6–36 months (mean, 24 months). On follow-up examination, all 84 women were found to have good anatomical vaginal vault support (Table 2; Fig. 1). Objective improvement in prolapse symptoms was observed from the POP-Q measurements, in particular the substantial reduction in mean value of point C, the distance of the vaginal cuff to the hymen (Table 2; Fig. 1). Seventy-four women had no objective findings of prolapse in any compartment, giving an overall objective cure rate of 88%.
On subjective assessment, 72 women (86%) were free of prolapse symptoms and 12 (14%) still had persistent symptoms of vaginal prolapse. On examination of the latter group, two had no physical finding of vaginal prolapse and were reassured accordingly. Six had persistent low rectocele with deficient perineal body and subsequently underwent posterior colpoperineorrhaphy with perineal body reconstruction 6 to 12 months later. The remaining four women had persistent anterior vaginal wall prolapse and underwent further prolapse repair; these comprised two laparoscopic paravaginal repairs, one anterior Prolift procedure and one anterior colporrhaphy under local anaesthesia.
Forty-eight women were sexually active. Of these, four (8%) had dyspareunia and vaginal soreness at 3 to 6 months. This was treated with vaginal topical oestrogen and subsequently resolved. Overall, substantial subjective (functional) improvement in vaginal symptoms, sexual well-being and general quality of life was observed postoperatively, as detected by the respective questionnaire scores (Table 3). The changes in mean scores for vaginal symptoms, sexual function and quality of life were each much greater than the standard deviations for the respective preoperative scores, indicating that these changes are statistically significant and therefore likely to be clinically significant.
Five women presented 3–15 months post-surgery with vaginal discharge and bleeding due to vaginal erosion by the polyester sutures or polypropylene mesh. This was treated initially with topical oestrogen and oral antibiotics and resolved successfully in two cases. Two women required trimming of their sutures. One woman had a small (5 × 10 mm) area of erosion by mesh and sutures in the upper third of the vagina, which did not respond to the topical oestrogen therapy. In this case, the exposed piece of mesh was excised vaginally under general anaesthesia. Excision of the mesh did not compromise support of the vaginal vault. All three women who had trimming of the sutures or mesh were asymptomatic 3 months later.
Discussion
Since it was first described in 1992 [17], numerous authors have published their experience of laparoscopic sacrocolpopexy for the management of post-hysterectomy vault prolapse [8–13]; however, most previous reports mainly describe objective anatomical outcomes. Ours is the first study evaluating sexual function after laparoscopic sacrocolpopexy. We report a large series and have evaluated functional, in addition to anatomical, outcome.
Our results support previous findings [9–14] that laparoscopic sacrocolpopexy is a safe and effective surgical treatment for post-hysterectomy vault prolapse. The procedure provided excellent vault support in all 84 women studied. However, persistent prolapse of the vaginal walls (but not the vault) was found in ten women on examination at 3 months postoperatively, resulting in a total persistence/recurrence rate of 12% and an overall objective cure rate [15] of 88%. Six women had persistent low rectocele and four had 1 to 2-degree cystocele. These were considered most likely to be persistent defects that had not been addressed adequately at the primary prolapse surgery. We noted that all the cases of persistent rectocele were in early patients who had not received any vaginal repair concomitantly with their laparoscopic sacrocolpopexy. Therefore, during the study, we amended our technique by first placing the mesh along the posterior vaginal wall laparoscopically and then performing a concomitant repair of any deficient perineal body vaginally. We observed that low laparoscopic placement of the mesh along the posterior vaginal wall to the level of the levator ani muscles did not correct perineal deficiency sufficiently. Our subsequent experience showed that transvaginal repair of the perineal body at the time of sacrocolpopexy gave better anatomical and functional results.
Intraoperative complications were rare and consisted of two bladder injuries that were managed laparoscopically without long-term sequelae. Medium-term complications included one case of mesh erosion and four cases of suture erosion. All four cases of suture erosion occurred when non-dissolvable polyester 2.0 (Ethibond) sutures were used, the removal of which was necessary in three cases. This observation led us to change to a slowly dissolvable suture material, monofilament polydioxanone (PDS). No cases of suture erosion were encountered after dissolvable sutures were used. One woman in our study (1%) had a small (5 × 10 mm) vaginal mesh erosion in the upper third of the vagina that did not respond to topical oestrogen therapy. This was completely excised and did not recur. Excision of the mesh did not compromise support of the vaginal vault. This finding is consistent with the 1–8% rate of mesh erosion previously reported for sacrocolpopexy by either the open or the laparoscopic route [9–13].
There is some controversy about the need to peritonise the mesh during sacrocolpopexy; the findings from one retrospective observational study suggest that the peritonisation of non-absorbable mesh in abdominal apical prolapse surgery may not be necessary [18]. Moreover, the authors suggested that burial of the mesh might, theoretically, contribute to complications such as ureteric injury or formation of retroperitoneal haematomas. Our own observational findings, from laparoscopies conducted on patients for other reasons, suggest that non-peritonised mesh can cause significant bowel adhesions. Therefore, our normal practice is to peritonise the mesh completely in order to minimize any possible bowel complications in the future.
Traditionally, the outcome of prolapse repair surgery is assessed by the degree of restoration of normal pelvic anatomy; however, such surgery inevitably has an effect, which may be considerable, on a woman's sexual function. This is often ignored as it is a difficult parameter to measure [19]. Our study is the first one to evaluate sexual function after laparoscopic sacrocolpopexy. The results in Table 3 show significant reductions in the average scores for all three domains (vaginal prolapse symptoms, sexual matters and related quality of life) of the ICIQ-VS questionnaire following laparoscopic sacrocolpopexy compared with the corresponding scores preoperatively. Therefore, it appears that overall sexual function is improved after laparoscopic sacrocolpopexy. The low rate of de novo postoperative dyspareunia (8%) observed in this study was surprising, as some previous studies have reported rates of up to 44% [19]. Interestingly, three women in their questionnaire assessments reported complete resolution of prolapse symptoms postoperatively but no improvement in sexual function, confirming that correlation between the anatomical and functional outcomes of surgery can be complex.
A weakness of our study is the relatively short follow-up period and the varying interval for subjective (questionnaire) assessment (6 to 36 months). A longer follow-up period is needed to draw conclusions about the rate of recurrent prolapse. Two years is also too short a time frame to reveal all mesh complications, as these can occur several years after surgery. Extrusion of mesh into the vagina has occurred up to 3 years following surgery [13] and extrusion of mesh following TVT has occurred 5 years after surgery [20].
The laparoscopic approach has a number of potential advantages, including excellent intraoperative visualisation of the pelvic anatomy, possible reduction in adhesion formation, decreased postoperative pain and quicker postoperative recovery. This study suggests that laparoscopic sacrocolpopexy is a safe technique that offers effective vault support comparable with that of the open procedure; however, surgeons need to be skilled in both prolapse and advanced laparoscopic surgery. In particular, a high level of laparoscopic suturing skill is necessary, if the efficacy of laparoscopic surgery is to replicate that of open abdominal techniques and if the surgery is to be completed in comparable time. Most published papers are based on the work of experienced surgeons who have performed large numbers of laparoscopic prolapse procedures.
Conclusions
Our results confirm previous findings that laparoscopic sacrocolpopexy is a safe and efficacious surgical treatment for post-hysterectomy vaginal vault prolapse. It provides excellent apical support and good functional outcome with significant overall improvement in sexual function. An extended period of follow-up is needed to confirm these findings over the longer term.
References
Marchionni M, Bracco GL, Checcucci V, Carabaneanu A, Coccia EM, Mececci F et al (1999) True incidence of vaginal vault prolapse. Thirteen years of experience. J Reprod Med 44:679–684
Toozs-Hobson P, Boos K, Cardozo L (1998) Management of vaginal vault prolapse. Br J Obstet Gynaecol 105:13–17
Flynn BJ, Webster GD (2002) Surgical management of the apical vaginal defect. Curr Opin Urol 12(4):353–358
Sarma S, Ying T, Moore K (2009) Long-term vaginal ring pessary use: discontinuation rates and adverse events. BJOG 116:1715–1721
Nygaad IE, McCreery R, Brubaker L (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynaecol 104:805–823
Maher CF, Qatawneh AM, Dwyer PL (2004) Abdominal sacrocolpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol 190:20–26
Benson JT, Lucente V, McClellan E (1996) Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. Am J Obstet Gynecol 175(6):1418–1421
Maher C, Baessler K, Glazener CMA, Adams EJ, Hagen S (2007) Surgical management of pelvic organ prolapse in women. Cochrane Database of Systematic Reviews, Issue 3
Agarwala N, Hasiak N, Shade M (2007) Laparoscopic sacral colpopexy with Gynemesh as graft material: experience and results. J Minim Invasive Gynecol 14:577–583
Sundaram CP, Venkatesh R, Landman J, Klutke CG (2004) Laparoscopic sacrocolpopexy for the correction of vaginal vault prolapse. J Endourol 18:620–623
Ross JW, Preston M (2005) Laparoscopic sacrocolpopexy for severe vaginal vault prolapse: 5-year outcome. J Minim Invasive Gynecol 12:221–226
Cosson M, Rajabally R, Bogaert E et al (2002) Laparoscopic sacrocolpopexy, hysterectomy, and Burch colposuspension: feasibility and short-term complications of 77 procedures. JSLS 6:115–119
Higgs PJ, Chua HL, Smith AR (2005) Long term review of laparoscopic sacrocolpopexy. BJOG 112:1134–1138
North C, Ali-Ross N, Smith A, Reid F (2009) A prospective study of laparoscopic sacrocolpopexy for the management of pelvic organ prolapse. BJOG 116:1251–1257
Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Price N, Jackson SR, Avery K, Brookes ST, Abrams P (2006) Development and psychometric evaluation of the ICIQ Vaginal Symptoms Questionnaire: the ICIQ-VS. BJOG 113:700–712
Ostrzen’ski A (1992) Laser video-laparoscopic colpopexy. Ginekol Pol 63:317–323
Elneil S, Cutner A, Remy M, Leather A, Toozs-Hobson P, Wise B (2005) Abdominal sacrocolpopexy for vault prolapse without burial of mesh: a case series. BJOG 112:486–489
Neill C, Abdel-Fattah M, Ramsay IN (2009) Sexual function and vaginal surgery. Obstetrician Gynaecologist 11:193–198
Ward KL, Hilton P, on behalf of the UK and Ireland TVT Trial Group (2008) Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow up. BJOG 115:226–33
Conflicts of interest
None.
Ethical approval
No ethical approval was required for this investigation, as it was a simple observational study (clinical audit).
Funding
No funding or sponsorship from any commercial or industrial source supported the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Price, N., Slack, A. & Jackson, S.R. Laparoscopic sacrocolpopexy: an observational study of functional and anatomical outcomes. Int Urogynecol J 22, 77–82 (2011). https://doi.org/10.1007/s00192-010-1241-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1241-y