Abstract
Introduction and hypothesis
Mesh-augmented reconstructive surgery for pelvic organ prolapse (POP) does not meet clinical expectations. A tissue-engineered fascia equivalent needs to be developed.
Methods
Human vaginal fibroblasts (HVFs) from 10 patients were characterized in vitro. Eligible HVFs and a biodegradable scaffold were used to fabricate a fascia equivalent, which was then transplanted in vivo.
Results
The cultured HVFs were divided into high (n = 6) or low (n = 4) collagen I/III ratio groups. Cells of the high-ratio group exhibited significantly higher proliferation potential than those of the low-ratio group (P < 0.05). A fascia equivalent was made with HVFs of the high-ratio group. In the subsequent animal study, a well-organized neo-fascia formation containing HVFs could be traced up to 12 weeks after transplantation.
Conclusions
Our results suggest that a tissue-engineered fascia could be developed from HVFs in vitro and in vivo, which might be an effective treatment for POP in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is a common disorder affecting women’s lives. Women with POP may suffer from chronic pelvic pain, stress urinary incontinence (SUI), and impaired quality of life. The lifetime risk of undergoing a surgery to correct POP or SUI is 11%, with 30% of patients needing re-operation [1]. Despite the high prevalence and recurrence rates of this disorder, its pathophysiology is still not fully understood. It has been speculated that a structural defect in the vagina and its supportive tissues is one of the mechanisms that predispose a woman to POP [2]. In an attempt to improve surgical outcomes, recently, synthetic mesh and biological grafts have been increasingly employed in reconstructive pelvic surgery for repairing POP [3].
Recent meta-analysis has showed that in anterior vaginal wall repair, there is short-term evidence that mesh/grafts significantly reduced objective POP recurrence compared with no mesh/grafts (relative risk 0.48, 95% CI 0.32–0.72). The recurrence rate was lower with non-absorbable synthetic mesh (8.8%) compared to rates associated with absorbable synthetic mesh (23.1%) or biological grafts (17.9%). However, the erosion rates were higher with synthetic non-absorbable mesh (10.2%) compared to the absorbable synthetic mesh (0.7%) or biological grafts (6.0%) [4]. A recent literature review indicated that in contrast to the great success rates associated with several small case series, an erosion rate of up to 26% and a dyspareunia rate of 38% has been reported for mesh introduced vaginally for POP repair [5]. Therefore, the U.S. Food and Drug Administration has recently announced to the public that serious complications can occur with trans-vaginal placement of surgical mesh for the repair of POP and SUI and recommend thorough counseling before an operation [6].
Currently, tissue-engineering includes cell transplantation and biodegradable scaffolds to construct biological substitutes that will restore and maintain normal function in diseased and injured tissues or organs. Regenerative medicine efforts including cellular therapy and tissue-engineering are also underway within the field of genitourinary tract reconstruction. De Filippo et al. demonstrated the first tissue-engineered vaginal tissue in vivo with vaginal epithelial and smooth muscle cells from female rabbits [7]. Atala et al. successfully treated seven young patients who needed cystoplasty with tissue-engineered autologous bladder transplantation [8]. Recently, para-urethral injection of autologous myoblasts with or without the additional injection of autologous fibroblasts has been used to treat women with SUI [9, 10].
We hypothesize that a tissue-engineered fascia equivalent can be developed in vitro with autologous fibroblasts and a biodegradable scaffold. In the future, this tissue-engineered fascia equivalent may then be transplanted in vivo to facilitate the formation of appropriate connective tissue during the repair of POP. In order to test our hypothesis, in this study, we tried to (1) characterize human vaginal fibroblasts (HVFs) in vitro with regard to their morphology, collagen contents, and proliferation potential; (2) construct a tissue-engineered fascia equivalent in vitro with eligible HVFs and an absorbable mesh scaffold; and (3) evaluate the histological outcomes of subcutaneous transplantation of the tissue-engineered fascia equivalent in experimental nude mice.
Materials and methods
Tissue biopsy and cell culture
Full-thickness vaginal walls were excised from the vaginal cuff during vaginal hysterectomies of 10 consecutive patients with benign uterine tumors (patients 1, 2, and 10) or symptomatic POP (patients 3, 4, 5, 6, 7, 8, and 9) (Table 1). The tissue samples were immediately washed in phosphate-buffered saline (PBS) solution to remove contaminated blood and were then cut into small pieces. HVFs were obtained by enzymatic digestion of tissue samples with 2 mg/ml collagenase type I (Gibco, NY, USA) overnight at 37°C. Isolated HVFs were subsequently cultured in Dulbecco’s modified Eagle medium (DMEM, Gibco) supplemented with 10% fetal bovine serum (FBS, Gibco) and 1% penicillin–streptomycin solution (Gibco) in culture flasks. For routine culture and experiments, HVFs were cultured in an incubator at 37°C in 5% CO2, 95% air, and 99% relative humidity, and the medium was changed every 2 days. HVFs at the second or third passage were used in the subsequent experiments. All experiments were repeated three times. All procedures that involved human subjects received prior approval from the IRB of our institute, and a written informed consent was obtained from each subject.
Cell morphology and phenotype identification
HVFs were cultured on round cover glasses in a 24-well plate. HVFs were fixed with methanol at 4°C for 15 min and washed with PBS three times. Mouse anti-human fibroblast surface protein (1:200, Abcam, Cambridge, UK) was added to the cells at 4°C overnight. After being washed with PBS three times, the cells were incubated with goat anti-mouse IgG-conjugated fluorescein isothiocyanate (FITC) (1:200, Molecular Probes, USA) at room temperature for 2 h, and then 4,6-diamidino-2-phenylindole dihydrochloride (DAPI) nuclear staining was performed at room temperature for 10 min. The slides were mounted with Prolong® Gold antifade reagent (Invitrogen, Carlsbad, CA, USA). The morphology and phenotype of the HVFs were observed under a light microscope and a fluorescence microscope, respectively (Carl Zeiss Axiovert 200M, Oberkochen, Germany).
Analysis of type I and III cellular collagen
Immunostaining
HVFs were cultured in six-well plates and were washed with ice-cold PBS three times and fixed with ice-cold methanol for 5 min. For blocking non-specific binding sites, HVFs were incubated in PBS with 1% bovine serum albumin (DMEM, Gibco) and washed with PBS three times. The HVFs were incubated with primary antibody mouse anti-human collagen type I (1:200, Sigma, USA) and goat anti-human collagen type III (1:200, Sigma, USA) at 4°C overnight followed by secondary antibody goat anti-mouse IgG-conjugated FITC (1:200) and rabbit anti-goat IgG-conjugated FITC (Molecular Probes) at room temperature for 2 h. The slides were mounted with Prolong® Gold antifade reagent (Invitrogen) and examined using a fluorescence microscope (Carl Zeiss Axiovert 200M, Oberkochen, Germany). The staining for collagen type I and III was done separately.
Western blotting
Equivalent amounts of protein were separated by electrophoresis on an 8% SDS–polyacrylamide gel and transferred to a polyvinylidine difluoride membrane (Millipore, MA, USA). The membrane was blocked with PBS containing 5% bovine serum albumin at room temperature for 1 h. The membrane was then incubated with primary antibody solution at 4°C overnight. After washing with PBS, the membrane was incubated with horseradish peroxidase (HRP)-conjugated secondary antibody at room temperature for 1 h. Signals were detected with enhanced chemiluminescence substrate (Perkin Elmer, Boston, USA) and the Fujifilm E1000 imaging system. Data were analyzed with Fujifilm Image Gauge V4.0 (Fuji film Science Lab 2001). Antibodies used for western blotting were mouse anti-human collagen type I (1:1,000, Sigma, USA), goat anti-human collagen type III (1:1,000, Sigma, USA), goat anti-mouse HRP-conjugated secondary antibody (1:4,000, Sigma, USA), and rabbit anti-goat HRP-conjugated secondary antibody (1:4,000, Sigma, USA).
Cell growth curve
HVFs were seeded at a density of 2 × 104 cells/well in 24-well plates for 90 min to allow for cell attachment. Randomly selected plates were photographed in five visual fields by a phase contrast microscope at the beginning, 0 h, and at 12, 24, 48, and 72 h after seeding. The cells were pre-cooled at 4°C for 30 min, fixed in methanol for 5 min, and stained with nuclear stain DAPI. The numbers of HVFs at different time points were calculated. The percentage of increasing HVFs at different time points was obtained (cell numbers at 12, 24, 48, and 72 h divided by the cell numbers loaded at the beginning). The percentage of HVFs was plotted against culture time to generate the growth curve. The experiment was repeated three times.
Fabrication of tissue-engineered fascia equivalent in vitro
The preparation was modified from the methods described by Nakanishi et al. [11]. In brief, a collagen gel was prepared by mixing 1.5 ml of ice-cold porcine collagen type I solution (BD Bioscience, Bedford, USA) with 0.5 ml of 5.7× DMEM (Gibco), 0.5 ml HEPES, 0.25 ml NaHCO3, 50 μl CaCl2, and 50 μl 0.1 N NaOH. Before polymerization of the gel in the inserts at 37°C, the HVFs suspension solution (5 × 105 cells/ml in 2.15 ml of 1× DMEM supplemented with 23.3% FBS; Gibco) was added to the collagen solution (the final collagen concentration was 1.1 mg/ml). The collagen solution containing the HVFs was then applied to the biodegradable poly-dl-lactico-glycolic acid (PLGA) mesh (Ethicon, Edinburgh, UK). The HVFs were labeled in advance with a 1:200 dilution of dialkylcarbocyanine fluorescent solution (Vybrant® DiI, Molecular Probes) according to the manufacturer’s protocol. DiI is a hydrophobic and lipophilic cyanine dye that can be incorporated into cell membranes. HVFs were stained and tracked in vitro and in vivo by using this dye. When the gel containing the HVFs underwent polymerization, DMEM supplemented with 10% FBS and ascorbic acid (final concentration, 50 ng/ml) was added. The scaffold seeded with HVFs (fascia equivalent) was kept in a submerged culture for 5 days in standard culture conditions before the animal study. Three sets (four pieces in each set) of the fascia equivalent were prepared with HVFs of high collagen I/III ratios from three patients (patients 5, 6, and 7, respectively) with symptomatic POP. PLGA mesh mixed with collagen gel without HVFs seeding was used for implantation as the control.
Graft transplantation and tissue procurement
Animal studies were performed according to the guidelines set by the Animal Research Committee at our institution. Three sets (four mice in each set) of experimental nude mice (8 weeks old) were prepared for the transplantation of the tissue-engineered fascia equivalent. Each mouse underwent subcutaneous transplantation with one HVFs-seeded (left side) and one unseeded (right side) scaffold under the back skin. The animals were killed at 2, 4, 8, and 12 weeks after transplantation to harvest tissue samples for the subsequent histological analysis.
Histological analysis
All specimens were fixed with formalin and embedded with paraffin. Tissue sections were cut for histological examination. All slides were photographed, and images were digitalized using a color digital camera and imaging software (Spot, version 2.1, Diagnostic Instruments, Sterling Heights, MI, USA). Localization of DiI-labeled cells was determined using a fluorescence microscope (Carl Zeiss Axiovert 200M, Oberkochen, Germany) filtered for excitation/emission at 546/590 nm. Cell nuclei were counterstained with DAPI, and HVFs were simultaneously identified by DiI.
Statistical analysis
All data were presented as mean ± SD (standard deviation). The statistical analysis was performed using paired Student’s t test. The level of statistical significance was set at P value <0.05.
Results
Vaginal tissue samples were harvested from 10 consecutive patients. The mean age was 55.5 (range 40–69) years old, and the median POP stage was 2 (range 0–3). The cultured HVFs demonstrated high cell purity with homogenous and typical cell morphology at the second or third passage. The phenotype of the HVFs was further identified by immunostaining of fibroblast surface protein.
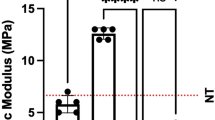
Collagen type I and type III were determined by immunostaining and Western blotting. HVFs derived from the 10 patients were divided into two groups: the high (ratio > 1.0; patients 1, 2, 5, 6, 7, and 10; n = 6) or low (ratio < 1.0; patients 3, 4, 8, and 9; n = 4) ratio group according to the collagen I/III ratios determined by Western blotting (Fig. 1a–c). The mean collagen I/III ratios of the high- and low-ratio groups were 1.26 ± 0.08 and 0.56 ± 0.13, respectively. HVFs with high collagen I/III ratios also expressed significantly greater cell proliferation potential than those of the low-ratio group after 72 h incubation of the subculture (7.83 ± 1.18 versus 3.12 ± 0.96, P < 0.01; Fig. 1d). The clinical data, collagen I/III ratios, and growth ratios of the HVFs of the 10 consecutive patients are summarized in Table 1.
Determination of cellular collagen I and III and the growth curve of cultured HVFs. a Immunostaining for the expression of collagen I and III differed among patients, with a decrease in collagen I shown in patient 4 compared to patient 1 (original magnification, ×400). b Western blotting results revealed a decrease in collagen I and an increase in collagen III in patients 3, 4, 8, and 9 that resulted in low collagen I/III ratios in these patients. c Patients were divided into two groups with either high or low collagen I/III ratios. d HVFs with high collagen I/III ratios expressed greater cell proliferation ability than those with low ratios
HVFs with high collagen I/III ratios from three patients (patients 5, 6, and 7) with symptomatic POP also expressed higher proliferation potential under cultured conditions. These HVFs were used for the subsequent experiment to construct the tissue-engineered fascia equivalent in vitro. Microscopically, at the beginning of the fabrication, HVFs appeared in the collagen gel, which was applied to the openings of the PLGA mesh (Fig. 2 a, a1). After 5 days of in vitro cultivation, a tissue-engineered fascia equivalent of high cellularity with homogenous distribution was harvested (Fig. 2 b, b1). Meanwhile, the previously DiI-labeled HVFs in the tissue-engineered fascia equivalent were traced under a fluorescence microscope after 5 days of in vitro cultivation (Fig. 2 c).
Fabrication of tissue-engineered fascia equivalent in vitro. a, b After 5 days of in vitro cultivation, a fascia equivalent was made with biodegradable PLGA mesh and the eligible HVFs (original magnification, ×40). a1, b1 are the magnification of a, b to demonstrate the rapid proliferation and homogenous distribution of HVFs cultured in the fascia equivalent (original magnification, ×200). c The previously DiI-labeled HVFs were identified in the fascia equivalent under fluorescence microscopy (original magnification, ×100)
Figure 3a, d shows the histological results of the tissue-engineered fascia equivalent up to 12 weeks after subcutaneous transplantation. Neo-fascia formation with complete resolution of the mesh was observed in all three sets that were transplanted. The newly formed fascia tissue was either a multi-layered structure with smooth contours (Fig. 3c) or a well-organized, lamellar structure with abundant cellularity and became well incorporated into the native tissues of the host (Fig. 3d). In contrast to the favorable outcome of the in vivo transplantation of tissue-engineered fascia equivalent, only one of the three sets that were implanted in the control group of collagen gel-coated PLGA mesh without cell seeding resulted in well-defined neo-tissue formation (Fig. 3e–h). However, the neo-tissue formation appeared as a disorganized, clumpy structure with scanty cellularity (Fig. 3g). Meanwhile, in the control study where no obvious neo-tissue was formed, a granuloma-containing inflammatory cells was noted (Fig. 3h).
The H&E staining results of the in vivo transplantation of the tissue-engineered fascia equivalent (a–d) and the control study (e–h). a Two weeks later, the fascia equivalent remained intact with superficial lamellar fascia-like tissue formation. Meanwhile, e a rapid degradation of the implanted mesh in the host was noted in the control. b At 8 weeks, a nodular neo-fascia with capsule formation was noted. Meanwhile, f a marked fibrotic tissue reaction was noted in the control. c After 12 weeks, a multi-layered neo-fascia with smooth contours or d a well-organized lamellar neo-fascia formation was noted following the transplantation of the fascia equivalent. In contrast, g a disorganized, clumped neo-tissue formation with scanty cellularity or h a granuloma formation was noted in the control study. (Original magnification, ×100 except a and d ×200; SK skin, SM superficial muscle, DM deep muscle, F fascia, FE fascia equivalent, MH mesh, TF tissue formation, arrow granuloma)
In addition, the neo-fascia formation after the in vivo transplantation of the tissue-engineered fascia equivalent was identified to be of human origin by the demonstration of previously DiI-labeled HVFs under fluorescence microscopy (Fig. 4a, b). Also, the collagen component was abundant in the neo-fascia as shown by Manson Trichrome staining (Fig. 4c).
The histological outcomes of the subcutaneous transplantation of the tissue-engineered fascia equivalent in experimental nude mice after 12 weeks using H&E staining, fluorescence microscopy, and Manson Trichrome staining (original magnification, ×100). a A neo-fascia formation was noted between the superficial muscle (SM) and deep muscle (DM) layers. b Under fluorescence microscopy, the newly formed fascia tissue was full of the previously DiI-labeled HVFs. c Manson Trichrome staining revealed abundant collagen content (blue) within the neo-fascia formation. (SK skin, SM superficial muscle, DM deep muscle, F fascia)
Discussion
To the best of our knowledge, this is the first study to successfully fabricate a tissue-engineered fascia in vivo with eligible HVFs. We found that cultured HVFs in groups with high cellular collagen I/III ratios (>1.0) expressed a significantly higher proliferation potential than the groups with low ratios (<1.0). Subsequently, we used HVFs with high collagen I/III ratios from patients with symptomatic POP to fabricate a tissue-engineered fascia equivalent. These tissue-engineered fascia equivalents transplanted subcutaneously in experimental nude mice resulted in a well-organized neo-fascia formation, which has been proven to be of human origin.
Human fibroblasts have the advantages of being easily harvested, cultured, and expanded in vitro, which make them an ideal cell source for regenerative medicine. In this study, we found that a homogenous cell population of typical morphology could be harvested by sub-culturing HVFs at the second or third passage. Applying these sub-cultured HVFs to develop a tissue-engineered fascia equivalent to reinforce the defective supportive or suspension tissue of the vagina in reconstructive pelvic surgery for repairing POP seems promising. In contrast, De Filippo et al. used vaginal epithelial and smooth muscle cells from female rabbits to make the first tissue-engineered vaginal tissue in vivo. However, they aimed to correct congenital vaginal anomalies and cloacal malformations [7]. Recently, there have been several clinical trials of cellular therapy using autologous fibroblasts. Weiss et al. [12] conducted a study to demonstrate the efficacy and safety of autologous fibroblast injections for treatment of various facial contour defects. Mitterberger et al. [9] used a double urethral injection of autologous myoblasts and fibroblasts to treat SUI in 123 women with 79% of patients being cured at a 1-year follow-up.
Our novel findings show that cultured HVFs in groups with high cellular collagen I/III ratios expressed a significantly higher proliferation potential than the groups with low ratios. However, the correlation of fibroblast proliferation and changes in collagen metabolism in vitro and in women with POP (in vivo) needs to be further explored. To date, there are limited investigations on the collagen metabolism of HVFs. Makinen et al. [13] studied the rates of collagen synthesis and pro-collagen mRNA levels in cultured fibroblasts of patients with POP. They found that these fibroblasts exhibited rates of collagen synthesis similar to or slightly higher than those from age-matched controls. However, the existence of a possible qualitative change of collagen subtypes could not be excluded in their study. In contrast, the collagen metabolism in skin fibroblasts derived from patients with inguinal hernias has been well investigated [14, 15]. POP is considered to share similar pathophysiology with the condition of a hernia, and it was found that patients with advanced POP also had a higher prevalence of this abnormality [16]. Zheng et al. [15] studied cultured skin fibroblasts from patients with recurrent inguinal hernias and found that both ratios of pro-collagen mRNAs type I/III and collagen type I/III decreased significantly in the patient group compared to the control group.
By using a modification of the tissue-engineering method as described by Nakanishi et al. [11], we were able to fabricate a fascia equivalent of high and homogeneously distributed cellularity in vitro within a short duration of five days. The efficiency of the tissue-engineering techniques may be a result of the usage of the extracellular matrix medium, e.g., the collagen gel in this study, to enhance the incorporation of the cells and mesh scaffold components. It is believed that in the tissue-engineered construct, the mesh scaffold contributes strength, and the extracellular matrix medium promotes cell growth and homogeneous distribution [17]. In their study, Nakanishi et al. successfully constructed a tissue-engineered urinary bladder wall by seeding porcine urothelial cells on a collagen sponge-PLGA mesh and smooth muscle cells on collagen gel–PLGA mesh scaffolds [11].
In the subsequent animal study and histological analysis, we have shown that the transplantation of the tissue-engineered fascia equivalent resulted in neo-fascia formation, which was well organized and appeared to be well incorporated into the native tissue of the host. In contrast, the implantation of the collagen gel-coated PLGA mesh scaffold resulted in a histological outcome that was obviously inferior. Furthermore, the serial histological findings indicated a tissue regeneration process following the in vivo transplantation of a tissue-engineered fascia equivalent (Fig. 3a–d). There is a progressive diminished inflammatory reaction concomitant with neo-fascia formation and maturation. Although the thickness of the neo-fascia formation varied at 12 weeks of transplantation, it did not seem to increase with time in the assessment period. The difference may be due to the surgical manipulation with single or multi-layered transplantation. Besides, the thin neo-fascia formation is not likely a granulation tissue reaction induced by surgery itself because it did not contain the defined components such as dilated vessels, infiltrated fibroblasts, and inflammatory cells. In contrast, the serial histological findings of the control study indicated an induced inflammatory reaction resulting in fibrotic tissue deposition or granuloma formation (Fig. 3e–h). Recently, Vandevord et al. examined the in vivo implantation of several biological sling materials and found varying stages of tissue remodeling through a 12-week evaluation. Changes in biocompatibility parameters such as capsule formation (collagen deposition), cellular infiltration, and angiogenesis were compared among different materials [18]. Similarly, the limitations of their study as well as ours is the difficulty in translating the knowledge gained from the animal model directly to humans, and the short-term (12 weeks) histological outcomes need to be verified by further long-term evaluation.
Another important histological finding in our in vivo experiment was that the DiI-labeled HVFs fully occupied the neo-fascia formation after the in vivo transplantation of the tissue-engineered fascia equivalent. This result indicates that it is the transplanted HVFs and not the host cells that aid in the regeneration process. Therefore, autologous cells for tissue-engineering applications in regenerative medicine should be screened for their eligibility beforehand to ensure favorable outcomes. As we have shown in this study, eligible HVFs for tissue engineering were cells with high collagen I/III ratios. Unfortunately, HVFs from most (4/7) of our patients with symptomatic POP had low collagen I/III ratios. Therapeutic regimens or replacement cell sources should be found for these patients. Zong et al. [19, 20] studied the cultured pelvic fibroblasts from women with POP and found that the active form of MMP-1 and MMP-13 is suppressed by the concomitant addition of estradiol and progesterone, suggesting their protective effect against collagen degradation. It has also been suggested that POP could be treated with autologous stem cells [21]. Recently, mesenchymal stem cells from human bone marrow have been successfully differentiated into the fibroblastic lineage [22].
In conclusion, we suggest that HVFs with high collagen I/III ratios, which also exhibit a high proliferation potential, could be the candidate cells for the construction of a fascia equivalent in vitro with a biodegradable scaffold. On the other hand, therapeutic regimens or replacement cell sources should be found for patients who have HVFs with low collagen I/III ratios and are, therefore, ineligible for therapeutic applications. The favorable histological outcome of in vivo transplantation of a tissue-engineered fascia equivalent resulting in a well-organized neo-fascia formation suggests a promising treatment option for POP in the future.
Abbreviations
- POP:
-
Pelvic organ prolapse
- SUI:
-
Stress urinary incontinence
- HVFs:
-
Human vaginal fibroblasts
- PBS:
-
Phosphate-buffered saline
- DMEM:
-
Dulbecco’s modified Eagle medium
- FBS:
-
Fetal bovine serum
- FITC:
-
Fluorescein isothiocyanate
- DAPI:
-
4,6-Diamidino-2-phenylindole dihydrochloride
- HRP:
-
Horseradish peroxidase
- ECL:
-
Enhanced chemiluminescence
- PLGA:
-
Poly-dl-lactico-glycolic acid
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Bump RC, Norton PA (1998) Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 25:723–746
Silva WA, Karram MM (2005) Scientific basis for use of grafts during vaginal reconstructive procedures. Curr Opin Obstet Gynecol 17:519–529
Jia X, Glazener C, Mowatt G, MacLennan G, Bain C, Fraser C, Burr J (2008) Efficacy and safety of using mesh or grafts in surgery for anterior and/or posterior vaginal wall prolapse: systematic review and meta-analysis. Br J Obstet Gynaecol 115:1350–1361
Baessler K, Maher CF (2006) Mesh augmentation during pelvic-floor reconstructive surgery: risks and benefits. Curr Opin Obstet Gynecol 18:560–566
Dwyer PL (2009) Minimally invasive surgery in urogynecology. Int Urogynecol J Pelvic Floor Dysfunct 20:485–486
De Filippo RE, Yoo JJ, Atala A (2003) Engineering of vaginal tissue in vivo. Tissue Eng 9:301–306
Atala A, Bauer SB, Soker S, Yoo JJ, Retik AB (2006) Tissue-engineered autologous bladders for patients needing cystoplasty. Lancet 367:1241–1246
Mitterberger M, Marksteiner R, Margreiter E, Pinggera GM, Colleselli D, Frauscher F, Ulmer H, Fussenegger M, Bartsch G, Strasser H (2007) Autologous myoblasts and fibroblasts for female stress incontinence: a 1-year follow-up in 123 patients. Br J Urol Int 100:1081–1085
Carr LK, Steele D, Steele S, Wagner D, Pruchnic R, Jankowski R, Erickson J, Huard J, Chancellor MB (2008) 1-Year follow-up of autologous muscle-derived stem cell injection pilot study to treat stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 19:881–883
Nakanishi Y, Chen G, Komuro H, Ushida T, Kaneko S, Tateishi T, Kaneko M (2003) Tissue-engineered urinary bladder wall using PLGA mesh-collagen hybrid scaffolds: a comparison study of collagen sponge and gel as a scaffold. J Pediatr Surg 38:1781–1784
Weiss RA, Weiss MA, Beasley KL, Munavalli G (2007) Autologous cultured fibroblast injection for facial contour deformities: a prospective, placebo-controlled, Phase III clinical trial. Dermatol Surg 33:263–268
Mäkinen J, Kähäri VM, Söderström KO, Vuorio E, Hirvonen T (1987) Collagen synthesis in the vaginal connective tissue of patients with and without uterine prolapse. Eur J Obstet Gynecol Reprod Biol 24:319–325
Rosch R, Klinge U, Si Z, Junge K, Klosterhalfen B, Schumpelick V (2002) A role for the collagen I/III and MMP-1/-13 genes in primary inguinal hernia? BMC Med Genet 3:2
Zheng H, Si Z, Kasperk R, Bhardwaj RS, Schumpelick V, Klinge U, Klosterhalfen B (2002) Recurrent inguinal hernia: disease of the collagen matrix? World J Surg 26:401–408
Segev Y, Auslender R, Feiner B, Lissak A, Lavie O, Abramov Y (2009) Are women with pelvic organ prolapse at a higher risk of developing hernias? Int Urogynecol J Pelvic Floor Dysfunct 20:1451–1453
Chen G, Sato T, Ohgushi H, Ushida T, Tateishi T, Tanaka J (2005) Culturing of skin fibroblasts in a thin PLGA-collagen hybrid mesh. Biomaterials 26:2559–2566
Vandevord PJ, Broadrick KM, Krishnamurthy B, Singla AK (2009) A comparative study evaluating the in vivo incorporation of biological sling materials. Urology (in press)
Zong W, Zyczynski HM, Meyn LA, Gordy SC, Moalli PA (2007) Regulation of MMP-1 by sex steroid hormones in fibroblasts derived from the female pelvic floor. Am J Obstet Gynecol 196(349):e1–11
Zong W, Meyn LA, Moalli PA (2009) The amount and activity of active matrix metalloproteinase 13 is suppressed by estradiol and progesterone in human pelvic floor fibroblasts. Biol Reprod 80:367–374
Bhatia NN, Ho MH (2004) Stem cell therapy for urinary incontinence and pelvic floor disorders: a novel approach. Curr Opin Obstet Gynecol 16:397–398
Lee CH, Moioli EK, Mao JJ (2006) Fibroblastic differentiation of human mesenchymal stem cells using connective tissue growth factor. Conf Proc IEEE Eng Med Biol Soc 1:775–778
Acknowledgments
We thank MY Lee and YF Lin for their technical assistance. This study was supported by Taichung Veterans General Hospital and Tunghai University (TCVGH-T) grant no. 947808, 957802, and 967803.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hung, MJ., Wen, MC., Hung, CN. et al. Tissue-engineered fascia from vaginal fibroblasts for patientsneeding reconstructive pelvic surgery. Int Urogynecol J 21, 1085–1093 (2010). https://doi.org/10.1007/s00192-010-1168-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1168-3