Abstract
Introduction and hypothesis
This is a randomized multicenter study comparing two mid-urethra tape procedures, the tension-free vaginal tape (TVT) with the tension-free vaginal tape-obturator (TVT-O) in terms of cure rate and complication rate.
Methods
Seven Finnish hospitals participated. Power calculations required 130 women in each group to detect a 10% difference in cure rate. A total of 267 underwent the allocated operation. Follow-up was scheduled at 2, 12, 36 and 60 months. A cough stress test was used as an objective outcome measure. Subjective outcome was assessed by five different condition-specific quality of life questionnaires.
Results
At 36 months of follow-up, 96% of the patients were evaluated. Objective cure rate was 94.6% in the TVT group and 89.5% in the TVT-O group (p = 0.131). Subjective cure rates were significant with no difference between the groups.
Conclusion
The TVT and the TVT-O are equally effective in the treatment of stress urinary incontinence after 36-month follow-up with no difference in complication rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The retropubic tension-free vaginal tape (TVT) procedure for treatment of female stress urinary incontinence, introduced by Ulmsten et al. [1], is the first modern mid-urethra tape procedure. This operation has changed the surgical treatment of stress urinary incontinence substantially over the last decade, and it provides significant short-, medium- and long-term cure rates (86%–91%) [2–5]. The effectiveness of the TVT operation is at least as good as that of the traditional incontinence operations as the Burch colposuspension and traditional pubovaginal slings [6, 7]. Although TVT is a minimally invasive technique, reported complications associated with the procedure include bladder perforations, as the most common one (3.8-6.5%), bleeding complications (1.9-2.7%), mesh erosion (0.9%) and at rare occasions bowel perforations (0.3%) [8–12]. To minimize the risk of complications attributed to the retropubic approach of tape placement, alternative procedures have been developed. The outside-in transobturator tape (TOT) procedure was developed in 2001 by Delorme [13]. The inside-out tension-free vaginal tape-obturator (TVT-O) was developed by de Leval [14] in 2003, in which the tape is introduced through the obturator foramen. Reported cure rates after short- and medium-term follow-up with the TVT-O have been similar to those observed with the TVT [15]. When patients have been classified according to the severity of stress incontinence, the TVT-O procedure has, however, shown a significantly lower cure rate than the TVT procedure in one study [16]. In the study by Schierlitz et al. [17], the TVT was found to be significantly more effective than the TOT in patients with intrinsic sphincter deficiency (ISD). Bladder perforations have been rare and voiding difficulties also less common with TVT-O, whereas groin/thigh pain and vaginal erosions of the mesh have been more common with TVT-O [18]. The reports on overall complication rates in randomized trials comparing TVT with transobturator methods have been somewhat contradictory [11, 19, 20].
As the TVT procedure is a gold standard procedure in the treatment of stress urinary incontinence, later-introduced procedures ideally should be randomly compared with the TVT procedure in order to get the most reliable information of the efficacy and safety of the procedures [18].
The present study was initiated in 2004 to randomly compare two mid-urethra tape procedures, the TVT with the TVT-O, in the treatment of primary stress urinary incontinence. Follow-up visits were scheduled at 2, 12, 36, and 60 months. The results of the 2- and 12-month follow-up have been published [19, 21]. We report on the results of the 36-month follow-up.
Materials and methods
The present study is a randomized, multicenter trial comparing tension-free vaginal tape (TVT) with transobturator vaginal tape inside-out (TVT-O). Seven hospitals in Finland participated in the study: four university hospitals and three central hospitals. Eight specialists in gynecology, with wide experience in urogynecology and TVT operations, were specially trained to perform the TVT-O procedure. After the training period, they had to perform at least five TVT-O operations independently before including patients in the study. The study was approved by the Helsinki University Central Hospital Ethics Committee. This clinical trial has been registered at http://www.ClinicalTrials.gov, and the identification number is NCT00379314.
Sample size calculation was performed assuming a 95% success rate for the TVT procedure and that a 10% difference in either success rate or rates of complications would be clinically important, with a 70% power to show a 10% difference; the sample size should be 260 patients with 130 in each group. Inclusion criteria were a history of stress incontinence, indication for surgical treatment of incontinence, a positive cough stress test performed in a semilithotomy position with a comfortably filled bladder (estimated to 200–300 ml) and a detrusor instability score (DIS) not more than 7 [22]. The inclusion and exclusion criteria are shown in Table 1.
The patients were recruited between March 2004 and November 2005. Randomization was performed using a computer-generated random allocation in a ratio of 1:1 in balanced blocks of four. The investigator called an independent randomization center after the patient had signed an informed consent. Preoperative and postoperative evaluation included a medical history, physical examination, urine analysis, a cough stress test, a 24-h pad weighing test and the following condition-specific quality of life questionnaires: the Urinary Incontinence Severity Score (UISS), which includes questions on the impact of urinary incontinence on everyday activities [23]; a Visual Analog Scale (VAS), where zero means no urinary problems and 100 means unbearable urinary complaints [23]; the Incontinence Impact Questionnaire-Short form (IIQ-7) [24] and the Urinary Distress Inventory-Short form (UDI-6) [24]. General quality of life was measured with the EuroQoL-5D (EQ-5D) questionnaire, which includes questions assessing mobility, self-care, usual activities, pain or complaint and anxiety or depression and the thermometer-like scale (0–100) assessing the general health at the moment [25, 26].
The TVT and TVT-O procedures were performed as previously described in detail by Ulmsten [1] and de Leval [14], respectively. Prophylactic antibiotics were given at the beginning of the operation: a single dose of cefuroxime 1.5 g or metronidazole 500 mg intravenously. All procedures were performed in local infiltration anesthesia using 0.25% prilocain with adrenalin, and a cough stress test was performed during the operation with 300 ml saline in the bladder for adjustment of the tape. Cystoscopy with 70° optic was performed twice during the TVT and once during the TVT-O to detect possible bladder injury. The bladder was emptied at the end of the operation, and no catheter was left in the bladder. Spontaneous voiding was attempted at the latest 3 hours after the operation and postvoid residual (PVR) urine volume were measured by ultrasound or by catheterization.
The 3-year postoperative evaluation was performed by an independent physician or by the operating surgeon together with a study nurse. Objective cure was defined as a negative stress test performed in the same manner as preoperatively. Subjective cure was evaluated by the questionnaires described above. The patients were also asked if they were satisfied with the operation completely, partly or not at all and if they would recommend the operation to a friend. Any complication experienced by the patient or registered by the investigator by careful physical examination and interrogation was registered.
Statistical analysis was performed using the SPSS for Windows 15.0 (Statistical Package for Social Sciences, Chicago, IL). Continuous variables were analysed with the paired samples t-test or with Wilcoxon signed ranks test to detect statistical difference between groups, and categorical variables were analysed with the chi-square test. A p value <0.05 was considered to indicate statistical significance.
Results
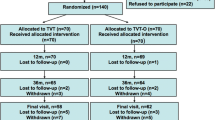
The flowchart of the trial is seen in Fig. 1. Two hundred and seventy three patients were randomized, and 267 patients received the allocated operation: 136 in the TVT group and 131 in the TVT-O group. Five patients dropped out between randomization and surgery. One TVT-O operation was altered to a TVT procedure due to technical difficulties with the TVT-O procedure. At the 36-month follow-up, 257 patients (96%) were evaluated and only 10 patients were lost to follow-up.
Among the patients seen at the 3-year postoperative visit, the stress test was negative in 94.6% of the patients in the TVT group and 89.5% of the patients in the TVT-O group, and they were thus regarded as objectively cured. The difference between the groups was not statistically significant (p = 0.131). Calculating the cure rates for both groups on an intention-to-treat basis, postulating that all the patients lost to follow-up were failures, the cure rates were 91.2% in the TVT group and 84.7 in the TVT-O group, the difference not being statistically significant (p = 0.105). Figure 2 shows the percentage of negative stress tests in both groups during the time of follow-up of the present trial. The 24-h pad test was also used as an outcome measure. The result of the pad test showed significant improvement from the mean (±SD, range) preoperative result of 41 g (±38 g; range, 0–207 g) to 3 g (±10 g; range, 0–95 g) 3 years postoperatively in TVT group and of 42 g (±53 g; range, 0–320 g) to 3 g (±10 g; range, 0–78 g) in TVT-O group, respectively. The 24-h pad test was negative (<8 g) [27] in 92.7% of the patients in the TVT group and 94.1% of the patients in the TVT-O group (p = 0.666). The scores of the condition specific quality of life questionnaires were significantly lower at the 3-year follow-up as compared with the preoperative measurements, the results of which are shown in Table 2. General health was assessed by EQ-5D score and EQ-5D thermometer-like VAS scale. The score in EQ-5D increased from preoperative 0.856 to 0.870 in the TVT group and from 0.873 to 0.895 in the TVT-O group. The EQ-5D scale improved in the TVT group from preoperative 80.01 to 82.99 three years postoperatively and from 80.41 to 83.94 in the TVT-O group (p = 0.031 and 0.001). These improvements were statistically significant with no difference between the groups.
Preoperatively, all patients had a detrusor instability score (DIS) of 7 or less (an inclusion criteria). De novo urgency, defined as new symptoms of frequency or urgency of moderate or severe degree in the UDI-6 or a score >7 in the DIS, was found in 12 (9.2%) of 130 patients in the TVT group and in 7 (5.6%) of 125 patients in the TVT-O group, the difference not being statistically significant (p = 0.270). Three patients in the TVT group and none in the TVT-O group used anticholinergic treatment at the 3-year follow-up visit.
Antibiotic treatment for urinary tract infections during the follow-up time after 2, 12 and 36 months was needed in 8%, 14.2% and 15.4% of the patients, respectively, in the TVT group and correspondingly in 13%, 16.8%, and 17.6% in the TVT-O group. One patient in the TVT group and five patients in the TVT-O group had used long-term prophylactic antibiotics because of recurrent urinary tract infections during the time period between the 1- and the 3-year follow-up visit. One patient in the TVT-O group continued prophylactic antibiotic treatment after the 3-year follow-up visit. The median PVR urine volumes were 5 (range, 0–115) ml in the TVT group and 10 (range, 0–302) ml in the TVT-O group, the difference being statistically significant (p = 0.032). Two patients in the TVT group had a PVR volume >100 ml (111 and 115 ml, respectively). Neither patient complained of voiding difficulties or had experienced urinary tract infections. In the TVT-O group, four patients had residual PVR volumes >100 ml (110, 112, 121 and 302 ml, respectively). Two of these patients had developed a grade 2 prolapse (the one with a PVR of 121 ml, a rectocele, and the one with a PVR of 302 ml, a cystocele), but had no complaints of voiding difficulties and had not experienced urinary tract infections. One patient with a PVR of 112 ml had experienced a total of nine urinary tract infection since the operation and one patient with a PVR of 110 ml reported occasional voiding problems.
Vaginal wall or other erosions were not seen in any of the patients at the 3-year visit. One TVT-O patient had tape erosion at the 1-year follow-up visit and a tape resection was performed, which resulted in recurrence of incontinence and a TVT re-operation was performed. Two other patients, who were not satisfied with the result of the TVT operation at the 12-month follow-up visit, had been reoperated with a TVT procedure. One of these two was lost to follow-up at 36 months. Two re-operated patients were evaluated, and they were continent. One patient had retention problems after TVT-O operation, and division of the tape was performed twice; 1 year 4 months and 1 year 7 months after the operation. Retention resolved after the last division of the tape, but the patient developed De Novo urge symptoms.
Satisfaction with the operation was complete in 90.0% of the patients in the TVT group and 91.2% in the TVT-O group. In the TVT group, 98.4% of the patients would definitely recommend the operation to a friend, and in the TVT-O group, the percentage was 95.2%.
Discussion
The present randomized study was designed to compare two mid-urethra tape procedures, the classical retropubic TVT and a newer modification, the transobturator TVT-O, in terms of efficacy and complication rates during a 5-year follow-up period. At 2 months of follow-up, the cure rates, defined by a negative stress test, were found to be 98.5% and 95.4% for the TVT and TVT-O, respectively [19] and, at 12 months of follow-up, to be 95.5% and 93.1%, respectively [21]. We presently report cure rates of 94.6% for the TVT procedure and 89.5% for the TVT-O procedure at 36 months of follow-up. The small differences in cure rates between the procedures do not reach statistical significance and do not either seem to have any clinical significance. The slightly steeper decline in the cure rates of the TVT-O group, illustrated in the Fig. 2, raises a small concern of a future development towards a significant difference in cure rates between the procedures at the 5-year follow-up. The latest Cochrane review of 2009 found a significantly lower objective cure rate for the obturator route than for the retrobupic one, while the subjective cure rates was similar [28]. Including all, the lost to follow-up patients as failures in an intention to treat analysis naturally gives slightly lower cure rates. The cure rates, however, are still high thus calculated with no difference between the groups.
The results of the present 36-month follow-up revealed complication rates, including De Novo urgency and urinary tract infections, of 24.6% in the TVT group and of 23.2% in the TVT-O group, with no difference in overall complication rate between the groups. De Novo urgency symptoms were recorded in 9.2% of the women in the TVT group and in 5.6% of the women in the TVT-O group, the difference not being statistically significant. Zullo et al. [20] reported De Novo overactive bladder symptoms in 9% of the patients in the TVT group and 0% in the TVT-O group after 12-month follow-up time, the difference, however not being statistically significant (p = ns). Karateke et al. [29] reported De Novo urgency symptoms in 14.8% and 12.0% in the TVT and TVT-O groups, respectively, in their 12-month follow-up study. They also found De Novo urge incontinence in 7.4% and 6.0% of the women in the TVT and TVT-O groups, respectively. The rate of De Novo urgency symptoms seems to be between 5% and 15% in the randomized studies where these symptoms have been recorded, and significant differences in the rates between the two approaches of tape placement do not seem to occur, which finding is further verified by the latest Cochrane report of 2009 [28].
At the 36-month follow-up visit of the present study, the incidence of urinary tract infections was of the same order in both groups 15.4% in the TVT group and 17.6% in the TVT-O group, respectively. There was only a small 3-ml difference in the measured median amount of residual urine volumes between the women with a history of urinary tract infections and those with no experienced infections. Median residual urine volumes were within normal ranges for both groups, 5 ml in the TVT group and 10 ml in the TVT-O group, the difference being statistically significant but of little clinical significance, as only two of the patients with a PVR more than 100 ml had clinical symptoms: repeat urinary tract infections and occasional voiding difficulties, respectively.
An increasing number of randomized trials comparing the TVT procedure with the TVT-O procedure have been initiated. Many of these have included a limited number of women with no power calculations performed. Four studies have enrolled a greater number of women, three of which reached the number required by the power calculation [12, 16, 29] and one by Wang et al. [30] with no power calculation, but 300 patients analysed. Our present trial is the largest one in which the number of patients required by the power calculation could be operated upon. The follow-up time of the trials reported on so far, comparing TVT with TVT-O, has been 12 months or less, except for the trial conducted by Wang et al. in which only half of the patients were analysed at 24 months and as little as 20% at 36 months of follow-up. We managed to bring back 96% of the women in our trial for the 36-month follow-up visit, who all could be assessed according to the protocol. Only the study by Araco et al. [16] found a significant difference in cure rate between the two procedures, where there was a 34% difference in cure rate in favour of the TVT procedure in women, who preoperatively were diagnosed to suffer from a more severe degree of stress incontinence. None of the other trials found a significant difference in cure rate. We have seen a trend of lower cure rates by time for the TVT-O group during our 3 years of follow-up. In a randomized trial comparing TVT with the outside-in TOT procedure in women with ISD, Schierlitz et al. [17] reported a significant difference in cure rates, 79% of the TVT group being urodynamically continent but only 55% of the TOT group being urodynamically continent.
The results of our randomized trial suggest that there is no significant difference in cure rates or complication rates between the TVT procedure and the TVT-O procedure during the 3 years of follow-up. This finding is supported by other randomized controlled trials with shorter time of follow-up. Some reports suggest, however, that the TVT might be more effective in cases with severe stress incontinence and in cases with ISD. Longer periods of follow-up will clarify if there is a greater decline in cure rate by time in women operated upon with the TVT-O procedure.
References
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7:81–85, discussion 85-6
Ulmsten U, Falconer C, Johnson P, Jomaa M, Lanner L, Nilsson CG et al (1998) A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 9:210–213
Ulmsten U, Johnson P, Rezapour M (1999) A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol 106:345–350
Nilsson CG, Falconer C, Rezapour M (2004) Seven-year follow-up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol 104:1259–1262
Nilsson CG, Palva K, Rezapour M, Falconer C (2008) Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 19:1043–1047
Jarvis GJ (1994) Surgery for genuine stress incontinence. Br J Obstet Gynaecol 101:371–374
Feyereisl J, Dreher E, Haenggi W, Zikmund J, Schneider H (1994) Long-term results after Burch colposuspension. Am J Obstet Gynecol 171:647–652
Tamussino K, Hanzal E, Kolle D, Ralph G, Riss P, Group Austrian Urogynecology Working (2001) The Austrian tension-free vaginal tape registry. Int Urogynecol J Pelvic Floor Dysfunct 12(Suppl 2):S28–S29
Kuuva N, Nilsson CG (2002) A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand 81:72–77
Kolle D, Tamussino K, Hanzal E, Tammaa A, Preyer O, Bader A et al (2005) Bleeding complications with the tension-free vaginal tape operation. Am J Obstet Gynecol 193:2045–2049
Liapis A, Bakas P, Giner M, Creatsas G (2006) Tension-free vaginal tape versus tension-free vaginal tape obturator in women with stress urinary incontinence. Gynecol Obstet Invest 62:160–164
Meschia M, Bertozzi R, Pifarotti P, Baccichet R, Bernasconi F, Guercio E et al (2007) Peri-operative morbidity and early results of a randomised trial comparing TVT and TVT-O. Int Urogynecol J Pelvic Floor Dysfunct 18:1257–1261
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 11:1306–1313
de Leval J (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44:724–730
Waltregny D, de Leval J (2009) The TVT-obturator surgical procedure for the treatment of female stress urinary incontinence: a clinical update. Int Urogynecol J Pelvic Floor Dysfunct 20:337–348
Araco F, Gravante G, Sorge R, Overton J, De Vita D, Sesti F et al (2008) TVT-O vs TVT: a randomized trial in patients with different degrees of urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 19:917–926
Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A et al (2008) Effectiveness of tension-free vaginal tape compared with TOT in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol 112:1253–1261
Latthe PM, Foon R, Toozs-Hobson P (2007) Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG 114:522–531
Laurikainen E, Valpas A, Kivela A, Kalliola T, Rinne K, Takala T et al (2007) Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. Obstet Gynecol 109:4–11
Zullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F et al (2007) One-year follow-up of tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence: a prospective randomised trial. Eur Urol 51:1376–1382, discussion 1383-4
Rinne K, Laurikainen E, Kivela A, Aukee P, Takala T, Valpas A et al (2008) A randomized trial comparing TVT with TVT-O: 12-month results. Int Urogynecol J Pelvic Floor Dysfunct 19:1049–1054
Kauppila A, Alavaikko P, Kujansuu E (1982) Detrusor instability score in the evaluation of stress urinary incontinence. Acta Obstet Gynecol Scand 61:137–141
Stach-Lempinen B, Kujansuu E, Laippala P, Metsanoja R (2001) Visual analogue scale, Urinary incontinence severity score and 15 d–psychometric testing of three different health-related quality-of-life instruments for urinary incontinent women. Scand J Urol Nephrol 35:476–483
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA (1995) Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. Continence program for women research group. Neurourol Urodyn 14:131–139
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343
Manca A, Sculpher MJ, Ward K, Hilton P (2003) A cost-utility analysis of tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence. BJOG 110:255–262
Victor A, Larsson G, Åsbrink AS (1987) A simple patient administered test for objective quantitation of symptoms of urinary incontinence. Scand J Urol Nephrol 21:277–279
Ogah J, Cody JD, Rogerson L (2009) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 4:CD006375
Karateke A, Haliloglu B, Cam C, Sakalli M (2009) Comparison of TVT and TVT-O in patients with stress urinary incontinence: short-term cure rates and factors influencing the outcome. A prospective randomised study. Aust N Z J Obstet Gynaecol 49:99–105
Wang W, Zhu L, Lang J (2009) Transobturator tape procedure versus tension-free vaginal tape for treatment of stress urinary incontinence. Int J Gynaecol Obstet 104:113–116
Conflicts of interest
C.G.N. has acted as consultant for Astellas, Ethicon and Pfizer. A.V. has acted as consultant for Astellas Ethicon and Pfizer. This study was instigated by the responsible researchers and funded by University-Administered funds.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Palva, K., Rinne, K., Aukee, P. et al. A randomized trial comparing tension-free vaginal tape with tension-free vaginal tape-obturator: 36-month results. Int Urogynecol J 21, 1049–1055 (2010). https://doi.org/10.1007/s00192-010-1160-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1160-y