Abstract
Introduction and hypothesis
Our objective was to evaluate bowel symptoms after colpocleisis.
Methods
This was a planned ancillary analysis of a prospective, colpocleisis cohort study of 152 women. Those with baseline and 1-year questionnaires (Colorectal-Anal Distress Inventory (CRADI) and the Colorectal-Anal Impact Questionnaire (CRAIQ)) were included. “Bothersome” CRADI symptoms (score>2(“moderately”, “quite a bit”)) were identified. CRADI and CRAIQ scores were compared, and postoperative symptom resolution and new symptom development were measured.
Results
Of 121 (80%) subjects with complete data, mean age was 79.2 ± 5.4 years and all had stage 3–4 prolapse. Procedures performed: partial colpocleisis (61%), total colpocleisis (39%), levator myorrhaphy (71%), and perineorrhaphy (97%). Bothersome bowel symptom(s) were present in 77% at baseline (obstructive (17–26%), incontinence (12–35%) and pain/irritation (3–34%)). All bothersome obstructive and most bothersome incontinence symptoms were less prevalent 1 year after surgery. CRADI and CRAIQ scores significantly improved. The majority of bothersome symptoms resolved (50–100%) with low rates of de novo symptoms (0–14%).
Conclusions
Most bothersome bowel symptoms resolve after colpocleisis, especially obstructive and incontinence symptoms, with low rates of de novo symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorders, including urinary incontinence, fecal incontinence, and pelvic organ prolapse (POP) are present in 23.7% of women in the USA and may increase with advanced age [1]. In the USA, surgery for POP and other pelvic floor disorders have increased in the last decade [2, 3]. While most prolapse surgeries restore and maintain vaginal coital function, higher risk patients with advanced age, medical comorbidities, extensive surgical history, and/or those not interested in maintaining coital function may be better served with a colpocleisis. Potential benefits of colpocleisis include its minimally invasive technique (superficial incisions without entry into the peritoneal cavity), high success rate [4], relatively short operating time, low blood loss, and ease of recovery.
As part of a multicenter, cohort study that evaluated the effects of colpocleisis on pelvic organ support, pelvic symptoms, and quality of life, women with an age range of 65 to 94 years reported improved satisfaction, as well as improved bowel symptoms, 1 year after colpocleisis [4]. Other studies have also reported improved bowel symptoms after other surgical treatments for POP. Sacrocolpopexy was found to improve both anal incontinence and obstructed defecation one year after surgery [5]. Another randomized controlled trial showed similar symptom improvement in bowel symptoms after two types of rectocele repair, with the most improvement observed for obstructive symptoms of straining and incomplete emptying [6].
More data is needed about the relationship of colpocleisis and specific bowel symptoms, such as fecal incontinence and obstructed defecation. Although the primary report from the above cohort study of women undergoing colpocleisis [4] revealed a general postoperative improvement in bowel symptoms, changes in individual bowel symptoms were not described. The purpose of this analysis was to study change in bothersome bowel symptoms after colpocleisis for the same cohort of women with advanced age. Specifically, we sought to determine rates of resolution of existing symptoms and development of new symptoms. We hypothesized that bothersome bowel symptoms would improve after colpocleisis with the most improvement observed for obstructive symptoms and less improvement for incontinence and pain/irritation symptoms.
Materials and methods
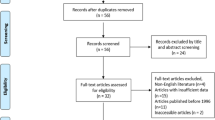
This was a planned ancillary analysis of bowel symptoms among women enrolled in a multicenter prospective, cohort study of 152 women undergoing total and partial (LeFort) colpocleisis [4]. The colpocleisis cohort study was performed through the Pelvic Floor Disorders Network (PFDN), a cooperative network sponsored by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Informed consent and institutional review board approval was obtained by individual PFDN sites.
Study patients underwent colpocleisis to surgically correct stages 3 and 4 POP. The type of colpocleisis (total or partial (LeFort)) as well as concomitant procedures such as perineorrhaphy, levator myorrhaphy, and/or incontinence surgery were performed at the discretion of the surgeon. Surgeons preserved the distal 3 to 4 cm of the anterior vaginal epithelium caudad to the urethrovesical junction. Total colpocleisis was defined as removal of all proximal anterior and posterior vaginal epithelium cephalad to the urethrovesical junction. Partial (LeFort) colpocleisis was defined as partial removal of the proximal anterior and posterior vaginal epithelium cephalad to the urethrovesical junction creating a longitudinal vaginal septum with bilateral vaginal epithelium tunnels. Data collection and methods have been published [4]. Baseline data collection included a Pelvic Organ Prolapse Quantification (POP-Q) exam [7], body mass index (BMI; kilograms per square meter), sociodemographic data, medical history, and surgical history (prior prolapse repair and hysterectomy). Bowel symptoms were evaluated at baseline and one year postoperative using validated quality-of-life measures including the Colorectal-Anal Distress Inventory (CRADI) and the Colorectal-Anal Impact Questionnaire (CRAIQ) [8].
The CRADI, a subscale of the Pelvic Floor Distress Inventory (PFDI), contains 16 questions that evaluate the presence of bowel symptoms and related bother. The CRADI has four subscales: obstructive, incontinence, pain/irritation, and rectal prolapse. Respondents are asked whether they experience each symptom, and if so, how much the symptom bothered them on a scale of 1 (not at all) to 4 (quite a bit). CRADI subscale scores range from 0 to 100 with higher scores indicating more severe symptom bother. The CRADI composite score is the sum of the four subscale scores and ranges from 0 to 400. The CRAIQ, a subscale of the Pelvic Floor Impact Questionnaire (PFIQ), measures the impact of bowel symptoms on 31 activities of daily living. Responses range from 1 (“not at all”) to 4 (“quite a bit”). The CRAIQ score ranges from 0 to 400 with higher scores indicating more severe functional impairment.
In order to describe the effect of colpocleisis on “bothersome” bowel symptoms, we defined the presence of individual “bothersome” CRADI symptoms as the presence of a symptom and a bother >2 (“moderately” or “quite a bit”). Bothersome symptoms were compared at baseline and 1 year after colpocleisis. Resolution of a bothersome baseline symptom at 1 year was defined as the absence of the symptom at 1 year after surgery or a bother score of ≤2 (“not at all” or “somewhat”). Development of a de novo bothersome symptom was defined as an absent baseline symptom or a CRADI score ≤2 preoperatively in a patient who recorded a score of >2 at 1 year postoperative. We also compared baseline and 1 year postoperative CRADI composite scores, CRADI subscale scores, and CRAIQ scores. In a subgroup of women who underwent levator myorrhaphy, we compared the resolution of bothersome bowel symptoms, the development of de novo bothersome symptoms, and the change in CRADI composite scores, CRADI subscale scores, and CRAIQ scores from baseline to 1 year after surgery. We also compared the effects of each type of colpocleisis (total or partial (LeFort)) on bowel symptom resolution and CRADI scores.
Continuous variables (age, BMI) were described using means and standard deviations (SD). Bowel symptoms were described using dichotomous variables (CRADI individual questions) and continuous variables (CRADI composite, CRADI subscales, and CRAIQ). Since the bowel symptoms with continuous scales were severely skewed to the right, they were described by median and interquartile range (IQR). To compare the presence of bothersome bowel symptoms at baseline and 1 year postoperative, we used McNemar's test for dichotomous data and Wilcoxon's signed-rank test for continuous data. Resolution of bothersome symptoms and de novo bothersome symptoms among groups were analyzed using Wilcoxon's scores test and Wilcoxon's signed-rank test. A p value of ≤0.05 was considered statistically significant.
In order to assess the magnitude of change in CRADI and CRAIQ composite and subscale scores, we calculated the group effect size for each score change. This measure evaluates change in relation to sample variation, providing a means of demonstrating that change has occurred and of presenting that change in a standardized metric [9]. The effect size was calculated as the change in mean score divided by the SD of the baseline score [10].
The sample size for this ancillary analysis was determined by the number of subjects enrolled in the original study (152), and was limited by the number of women that had complete baseline and 1 year postoperative CRADI and CRAIQ questionnaires.
Results
One hundred fifty-two patients enrolled in the colpocleisis cohort study, of whom 121 (80%) completed both baseline and 1-year questionnaires. Clinical and demographic characteristics of subjects with complete data (Table 1) were similar to those without complete data with respect to sociodemographics, prior medical history, POP-Q stage, and baseline bowel symptoms.
As detailed in Table 2, at least one bothersome bowel symptom was present in 77% of subjects at baseline, including obstructive symptoms (17–26%), incontinence symptoms (12–35%) and pain/irritation symptoms (3–34%). All bothersome obstructive and most bothersome incontinence symptoms were less prevalent 1 year after surgery with the exception of fecal incontinence of solid stool (p = 0.23). While the prevalence of three of the pain/irritation symptoms (fecal urgency, mucus with bowel movements, and hemorrhoids) was lower postoperatively, the prevalence of the remaining four symptoms (low back pain, pain prior to bowel movements, pain with defecation, and pain with straining) was not significantly different.
Detailed in Table 3, the CRADI composite scores, CRADI subscale scores, and CRAIQ scores were all significantly lower (p < 0.01) 1 year after colpocleisis indicating an overall improvement in all aspects of bowel symptoms. The greatest improvement was observed in the CRADI composite score and the CRADI obstructive and incontinence subscale scores in comparison to the CRADI pain/irritation subscale score and CRAIQ score. The effect sizes for the CRADI composite, CRADI-obstructive, CRADI-incontinence, CRADI-pain/irritation and CRAIQ score changes were 0.48, 0.53, 0.42, 0.31, and 0.33, respectively.
Presented in Table 4, bothersome bowel symptoms resolved in the majority of subjects (50–100% for each symptom) with low rates of de novo bothersome symptoms (0–14%). Concomitant levator myorrhaphy influenced neither the resolution of bothersome bowel symptoms nor the development of de novo symptoms with one exception: de novo incomplete bowel emptying did not develop in any of the women who had a myorrhaphy but developed in three (11%) that did not undergo myorrhaphy (p = 0.03).
At baseline and 1 year, there were no differences in CRADI composite scores, CRADI subscale scores, and CRAIQ scores between the women who had levator myorrhaphy and those that did not undergo myorrhaphy (data not included.) Also, bowel symptom resolution, CRADI composite score, and CRADI subscale scores were not significantly different between the total and partial (LeFort)) colpocleisis subjects.
Discussion
This secondary analysis from a prospective observational study demonstrates that bothersome colorectal symptoms are common in older women with stages 3–4 prolapse, and that most symptoms improve after colpocleisis with perineorrhaphy. All bothersome obstructive symptoms and almost all incontinence symptoms were less prevalent after surgery, and the development of new bothersome bowel symptoms was uncommon.
Little data has been previously published on bowel function after colpocleisis. Barber et al. [11], reported improvements in overall CRADI and CRAIQ scores in 30 women followed-up 1 year after colpocleisis. The bowel symptom changes seen by Barber et al. and reproduced here in a larger cohort of women are similar to improvements reported after both abdominal and vaginal reconstructive prolapse surgeries, despite an older study population in the colpocleisis cohorts [5, 6, 11]. It is reassuring that bowel symptoms improve with surgical procedures that correct severe apical support defects (sacrocolpopexy), posterior compartment defects (rectocele repair), and global support defects involving all compartments (colpocleisis).
This study adds to the literature by providing detail about colorectal symptom subtypes and individual symptom changes after colpocleisis. Among the CRADI subscales, the obstructive and incontinence symptom scores demonstrated the greatest improvement. All individual bothersome obstructive and incontinence symptoms (except incontinence of solid stool) were significantly less frequent after surgery. While the pain-irritation symptom subscale demonstrated modest score improvement overall, changes in individual pain-irritation symptoms were more variable, perhaps because these symptoms may more often result from underlying bowel disorders rather than from POP. Persistent bothersome bowel symptoms after colpocleisis that do not respond to medical management can be evaluated using techniques such as colonoscopy, dynamic MRI, defecography, and anal manometry.
Levator myorrhaphy or plication is performed routinely with colpocleisis by many surgeons to reduce the genital hiatus, although to our knowledge, no comparative study exists to support or refute this practice. As previously published, in this prospective cohort study, anatomic success did not differ by levator myorrhaphy [4]. Similarly, we did not find substantial differences in individual bowel symptom resolution or in new symptom development in those women who did or did not have levator myorrhaphy with colpocleisis, but we caution that our power to compare these groups was limited. Furthermore, since levator myorrhaphy was not performed in a randomized fashion, measured and unmeasured differences between the groups may have existed at baseline, limiting our ability to compare their outcomes. Reassuringly, in the larger group who had concurrent levator myorrhaphy, CRADI (total and subscale), and CRAIQ score changes all significantly improved after surgery, suggesting that this procedure when performed with colpocleisis is not associated with detrimental outcomes in terms of bowel symptoms.
Strengths of this study include the prospective design and the use of validated instruments to measure bowel symptoms. The multi-center study design also enhances generalizability of the results. While not surprising in an older study population, the loss to follow-up at 1 year (15%) was a limitation of the study, further limiting the power of subgroup comparisons. Possible reasons for the 15% loss to follow-up may include greater burden of comorbid conditions, worsening functional status, and even death.
Finally, although we demonstrated statistically significant changes in the CRADI and CRAIQ scores after surgery, such changes may not always represent clinically significant differences. The minimum important difference (MID; the smallest change in score associated with a clinically meaningful change in a questionnaire) [12] was recently reported for the urinary subscales of the PFDI and PFIQ, [13] but has not yet been reported for the CRADI and CRAIQ. However, a change equivalent to an effect size of 0.5 (or score change equal to half of the baseline score SD) may be used to approximate the MID, and this is roughly what we observed for the CRADI composite and CRADI obstructive scale scores, suggesting that the symptom improvement we observed is clinically significant. Further research using these questionnaires is needed to better understand these differences.
In conclusion, individual bothersome bowel symptoms, including obstructive, incontinence, and some pain/irritation symptoms, improve after colpocleisis, and the development of new bothersome bowel symptoms is uncommon. Given the high prevalence of bothersome colorectal symptoms found in this cohort of women, our finding that the majority of these symptoms resolve after colpocleisis is significant. These results should be useful to clinicians in counseling patients planning colpocleisis for advanced POP.
References
Nygaard I, Barber M, Burgio K, Pelvic Floor Disorders Network et al (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300:1311–1316
Shah AD, Kohli N, Rajan SS, Hoyte L (2008) The age distribution, rates, and types of surgery for pelvic organ prolapse in the USA. Int Urogynecol J Pelvic Floor Dysfunct 19:421–428
Anger JT, Weinberg AE, Albo ME et al (2009) Trends in surgical management of stress urinary incontinence among female Medicare beneficiaries. Urology 74:283–287
Fitzgerald MP, Richter HE, Bradley CS, Pelvic Floor Disorders Network et al (2008) Pelvic support, pelvic symptoms, and patient satisfaction after colpocleisis. Int Urogynecol J Pelvic Floor Dysfunct 19:1603–1609
Bradley CS, Nygaard IE, Brown MB, Pelvic Floor Disorders Network et al (2007) Bowel symptoms in women 1 year after sacrocolpopexy. Am J Obstet Gynecol 197:642–648
Gustilo-Ashby AM, Paraiso MF, Jelovsek JE, Walters MD, Barber MD (2007) Bowel symptoms one year after surgery for prolapse: further analysis of a randomized trial of rectocele repair. Am J Obstet Gynecol 197(76):e1–e5
Bump RC, Mattiasson A, Bo K, Brubaker LP et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC (2001) Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 185:1388–1395
Revicki D, Hays RD, Cella D, Sloan J (2008) Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol 61:102–109
Wyrwich KW, Wolinsky FD (2000) Identifying meaningful intra-individual change standards for health-related quality of life measures. J Eval Clin Pract 6:39–49
Barber MD, Amundsen CL, Paraiso MF, Weidner AC, Romero A, Walters MD (2007) Quality of life after surgery for genital prolapse in elderly women: obliterative and reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct 18:799–806
Crosby RD, Kolotkin RL, Williams GR (2003) Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol 56:395–407
Barber MD, Spino C, Janz NK, Pelvic Floor Disorders Network et al (2009) The minimum important differences for the urinary scales of the Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaire. Am J Obstet Gynecol 200(580):e1–e7
Acknowledgements
Supported by the National Institute of Health Office of Research on Women's Health with grants from the National Institute of Child Health and Human Development (U01 HD41249, U10 HD41268, U10 HD41248, U10 HD41250, U10 HD41261, U10 HD41263, U10 HD41269, and U10 HD41267) and the National Institute of Diabetes, Digestive and Kidney Diseases (K24 DK068389).
Conflicts of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Oral presentation at the 35th Annual Society of Gynecologic Surgeons Scientific Meeting in New Orleans, Louisiana, 30 March to 1 April 2009.
Rights and permissions
About this article
Cite this article
Gutman, R.E., Bradley, C.S., Ye, W. et al. Effects of colpocleisis on bowel symptoms among women with severe pelvic organ prolapse. Int Urogynecol J 21, 461–466 (2010). https://doi.org/10.1007/s00192-009-1062-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-1062-z