Abstract
Introduction and hypothesis
Urinary incontinence (UI) is a prevalent clinical condition especially among women aged 40 years and above. It is not often reported as it is considered an age-related problem. This study attempts to estimate UI among women above 40 years and its determinants in an area zone of Tehran, Iran.
Methods
In this cross-sectional study, a total of 800 women were selected from residents of area zone 17 of Tehran.
Results
Prevalence of UI is estimated to be 38.4% (95% CI, 0.35–0.42). Our findings show that those who suffer from osteoarthritis or chronic cough, had any type of internal surgery, had rupture during delivery, and had no regular exercise are significantly at higher risk of UI.
Conclusion
The rather high prevalence of UI among middle-aged women has negative impact on women's quality of life; therefore, strategies regarding prevention and management, medical education, and research programs have been proposed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Iran, like many other developing countries, has had significant improvements regarding health and disease control in the past five decades resulting in an increased life expectancy. Nonetheless, longer life expectancy is also associated with more chronic conditions and thereby necessitates longer clinical cares.
Pelvic floor disorders (PFD) is a prevalent condition in women especially among older age groups. It includes a wide variety of clinical conditions, one of which is urinary incontinence (UI). UI is mainly related to different anatomic features and performances of women's pelvic floor organs [1]. Research has shown that some risk factors of PFD and especially UI among women are: age, number of pregnancies and childbirth, mode of delivery, post menopausal conditions, type of diet, and restricted mobility [2–5]. PFD is a hidden public health problem of epidemic proportions, and it seems an integral part of women's role in reproductive process. Trauma, which may happen during a vaginal birth, can cause nerve and muscle damage, and tissue disruption; therefore, it can lead to UI or other PFD conditions [1]. The prevalence of UI ranges from 10% to 40% in middle-aged women and rises to about 69% in older women [2, 6, 7]. Comparisons among different studies are also limited due to lack of standard definition and precise reproducible methods for UI assessment. As a result, prevalence rates of UI vary according to definitions and diagnostic methods [1, 5, 7]. As the issue may be embarrassing and stressful, women, especially in Iranian culture, rarely discuss the problem of UI with their health care providers and consider it as a natural result of the aging process. Some of the undesirable consequences of keeping the problem untold are: adverse effect on social life and intimate relationships, decreased self-esteem, and lower quality of life; moreover, it can cause financial burden to the health system [2].
Studies in Iran on PFD indicate that UI is quite common among women of reproductive age who refer to medical settings, and it is significantly related to the number and mode of delivery. Based on a local study, 31.8% of women aged 15–49 years suffered from stress UI, 25.5% from urge UI, 19.4% from mixed UI, and 23.3% from overactive bladder (OVB) [8]. In another population-based study in Iran, the prevalence of OVB was estimated to be 18.2%; moreover, it increased with age from 10.9% in women aged 15–29 years to 26.2% in those above 50 years of age [9]. However, to our best knowledge, no epidemiological study of UI in women of general population in Iran has been conducted so far. Majority of studies conducted in Iran are based on medical settings where women have been referred during the period of their postpartum or reproductive years. The corresponding data are also less focused on UI and its risk factors in older women especially in general populations. The aim of this population-based study is to determine the prevalence of UI and its underlying risk factors in women above 40 years of age and to find possible primary preventive strategies.
Methods and materials
Study population and design
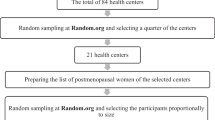
In this cross-sectional study, our study sample comprised of 800 women who were 40 years of age and above. They were selected via cluster sampling from among the residents of Tehran zone No. 17 (which is a very heterogeneous area in terms of population structure) in 2007. Clusters were initiated based on primary schools’ addresses in the zone, and the number of each cluster was selected as appropriate for one working day for each team. Each working team consisted of two female medical students who were trained about the research objectives and had research backgrounds to interview women at their homes.
Data collection
Data were obtained for women who gave complete answers to questions asked. The questionnaire consisted of demographic and personal characteristics, pregnancy and delivery history, physical and nutritional practices, medical and surgical history, and UI symptoms. Women who reported current urinary tract infection were excluded from the study.
Definitions and terms
Focusing on more severe and problematic symptoms of urinary incontinence, we defined UI through a positive response to any of the following three questions: (1) daily leakage of any amount of urine, (2) any leakage occurred during physical activities, coughing, sneezing, or laughing, and (3) using pads for urinary leakage.
The examined risk factors were : age (40–49; 50–59; 60–69; >70 years), delivery type (normal vaginal, cesarean section, vaginal delivery with forceps or vacuum extraction), parity (nulliparous, 1, 2–3, >3 births ), perineal rupture or episiotomy (non, by physician or midwife, spontaneous), age at first delivery (<18, 19–30, >30 years), diseases of osteoarthritis, depression, osteoporosis, chronic cough, bowel disease , diabetes, and pelvic surgery (yes or no). The variables of lifestyle include: beverage, vegetable and fruits consumption, and physical activity which were assessed through self report. Beverage consumption was obtained using number of daily glasses of any liquid drinks such as pure water, tea, coffee, or others. Beverage daily consumption was categorized into three levels: low (less than three glasses), moderate (four to seven glasses) and high or acceptable (greater than seven glasses). Vegetable and fruits consumption was assessed using two questions and were categorized in groups of low (less than two cups per day) and acceptable (greater than or equal to two cups per day). Physical activity was assessed using four questions of daily routine activity, daily walking, daily 10-min exercise, and weekly 90-min physical activity. It was then categorized into four groups of no regular exercising, low, medium, and high level of physical activity, respectively.
Statistical analysis
Descriptive statistics are reported through frequencies and percentages. Univariate associations of outcome variable (urine incontinence) with related risk factors were assessed using the chi-square test. For the univariate analysis, crude odds ratio (OR) and the 95% confidence intervals have also been given .The simultaneous effects of covariates on UI as dependent variable have been assessed via multiple logistic regression using the Hosmer–Lemeshow guideline [10] for variable selection.
Results
Our study sample comprised of women in the age range of 40–95 with a mean age of 53.96 years (SD = 9.96). The effect of cluster sampling was checked through methods of the survey analysis; the design effect for UI was estimated to be 0.97. This indicated that there was a very low intraclass correlation within the clusters. Therefore, there was no need for considering the effect of cluster sampling, and we proceeded with simple analysis. Out of 800 participants, 307 (38.4%) individuals suffered from UI (95% CI, 0.35–0.42). The results of univariate associations between UI and related risk factors are summarized in Tables 1, 2, and 3 categorized for three sets of variables: personal and lifestyle, disease morbidity, and delivery background.
Daily activity was the only variable of the first group (personal and lifestyle) that was significantly associated with UI (P = 0.003). The chance of UI was higher among those who claimed no regular exercising compared to those who had high levels of physical activity (OR = 2.31; 95% CI, 1.08–4.96; Table 1).
As for the disease variables, bowel diseases and diabetes mellitus were the variables that failed to show significant association with UI (P = 0.424, P = 0.063); however, UI was strongly associated with chronic cough (OR = 2.012; Table 2).
Among the variables of the third group, number and type of delivery, and age at first delivery were not significantly associated with UI; however, episiotomy during vaginal delivery was the variable that showed significant association with UI (P = 0.009); so that women who had episiotomy by midwife or physician were 72% more at risk of urine incontinence (OR = 1.718) compared to those who did not experience any perineal rupture.
The simultaneous effect of variables was first checked within each set, followed by assessing the overall effect in a final model.
Only in the second group did we reach an appropriate model by the Hosmer–Lemeshow guideline for variable selection (Table 4). The final model was then assessed (Table 5) using this model and variables significantly associated with UI in the other two groups. Age was included in all models. Five variables remained significant in the final model: osteoarthritis, chronic cough, pelvic surgery, episiotomy, and physical activity.
Discussion
In this population-based study, we investigated the prevalence of UI and its underlying risk factors among 800 women of 40 years of age and above. The estimated prevalence of UI indicates that it is a common health problem among middle-aged and older women. It does have a negative impact on their lives, causing distress and embarrassment in their social life. Nonetheless, a review of the literature shows a rather wide range for this prevalence. Specifically, it varies from 10% to 69% [2, 4, 5, 7, 11]. However, this wide range is mainly due to differences in definitions of incontinence, measurement instruments used, and survey methodologies [5, 7]. The discrepancy in prevalence of UI necessitates the need for a unified definition; therefore, results from different studies would be comparable. The definition used in this study was focused on more serious and problematic symptoms of UI such as: stress UI, daily leakage of any amount of urine, and using pads for urinary leakage. These symptoms are more of a concern not only in terms of hygiene, but also in terms of social relations.
Moreover, the rather high prevalence of UI compared to other studies in Iran could be due to different criteria used in definition as well as different survey methodologies. Herein, we used questionnaire as a tool to gather data instead of clinical or paraclinical tests.
The strong point of this study lies in the fact that it was the first attempt to determine the prevalence of UI in women of the general population and to find its risk factors. This information is critical for targeted interventions aimed at preventing related morbidity.
In a population-based study in the US, the overall prevalence of UI in women was reported as 45%; it increased with increasing age from 28% among 30–39-year-old to 55% in 80–90-year-old women [4]. Huang et al. reported the prevalence of weekly UI as 18% among Asian-American women aged 40–69 years old [11]. Swithinbank has estimated the prevalence of UI in female residents of a British city as high as 69% [5]. Another epidemiological study on 2,000 Swedish women in 1997 reported the prevalence of UI as low as 9% in 40-year-old women although the prevalence was 19% in 60-year-old women [12]. Comparing UI prevalence in different regions shows a wide range from lowest in Scandinavian countries to highest in the US and the UK. In this study, the overall prevalence of UI was 38.4%. This condition can be a problematic health issue among Iranian women considering a longer life expectancy in the future.
Danforth et al. and Melville et al. in their cross-sectional studies showed that UI prevalence increased by age, BMI, parity, smoking, diabetes, depression, and history of hysterectomy [2, 4]. In this study, UI risk factors were categorized in three groups: personal and lifestyle, disease morbidity, and child delivery factors.
Among personal and lifestyle variables, only physical activity was significantly associated with UI. In a population-based study conducted by Hannestad et al. among Norwegian women, a significant relationship between UI and physical activity and drinking tea was also reported; moreover, osteoarthritis, chronic cough, and history of pelvic surgery were among medical conditions most associated with UI [3]. Maclennan et al. have shown high prevalence of pelvic floor disease in women with arthritis, osteoporosis, and coughing [13]. Chronic obstructive pulmonary diseases are also reported as risk factors for UI by Huang et al. and Sobhgol et al. [8, 11]. The results of the present study also indicate the significant associations between UI and osteoarthritis, chronic cough, and history of pelvic surgery. One explanation for the association of osteoarthritis and UI could be due to the possible side effects of the disease itself, or the medications these patients might have taken.
Some studies report that UI prevalence increases with age [5, 13, 14]; however, this has not been concluded in the present study. Unlike some studies such as the one by Swithinbank et al. [5], our study did not show any significant association between age and UI. This may particularly be due to different age groups involved. Our study sample was confined to women above 40 years of age; whereas, some studies also recruited women in the age range of 30–39 years old. This could be due to increasing prevalence during reproductive young adult life to a broad peak around middle age, and then a steady little increase later in life. However, there was no noticeable difference in the prevalence of UI among women over 40 years of age [5].
In our study, we did not find a significant association between UI and variables of the delivery background except for perineal rupture or episiotomy. Nevertheless, some studies have reported a significant association between parity and UI [1, 2, 4, 8, 13]. Such association was not observed in our study; this could be explained by the fact that the first or second birth seems to cause the most negative effects. The findings by Sobhgol et al. also indicate a significant association between delivery background variables such as: gravidity, delivery without episiotomy, vaginal delivery, and parity with stress, urge, and mixed incontinence as well as with overactive bladder [8]. Rizk et al., in his study, showed that episiotomy had no significant association with UI but had positive correlation with history of previous instrumental delivery [15]. Some studies show differences for PFD prevalence between cesarean, vaginal, and instrumental delivery [13].
Vaginal delivery is a main determinant of PFD, and it is often done under medical supervision. Injuries during this episode can be clarified on their occurrences and can be led to effective strategies for prevention targeted at those who have a high risk of injury. Gynecologists are well aware and do realize the magnitude of this hidden epidemic of urinary incontinence among women. They also know that a considerable rate of UI could end in severe cases that may require surgery; therefore, could result in heavy cost impact and adverse health outcomes.
Some preventive recommendations are based on comprehensive reviews on PFD conditions such as UI with examining the role of obstetric management in the prevention, and assessment of UI primary prevention opportunities at the time of child delivery as a major determinant of PFD.
Preventive strategies such as primary elective cesarean or avoiding episiotomy have recently been based primarily on expert opinion. These strategies avoid injuries due to vaginal delivery; however, there are not enough research evidences supporting our hypothesis which will weaken the ability to assess its effectiveness. This can, in a way, explain the high rate of cesarean deliveries among Iranian women [16] whether it is done on the women's will or by doctors' advice. Traditionally, women in Iran considered child birth as a natural process, and were seriously against any interference with it such as cesarean or instrumental delivery. Women strongly believed that cesarean delivery should be performed only for medical indication; an attitude which has been quite changed recently. Elective cesarean birth is now popular and is unexpectedly increasing especially among urban women. One possible reason is probably due to physician recommendation to avoid suffering from possible injuries and damages to pelvic floor supportive function. This issue should be included in medical education programs (curriculum) and researches.
Conclusion
This survey presents a new insight into epidemiology of UI in middle-aged and older Iranian women from the general population. Its results can be useful to plan subsequent health care programs for incontinent women. The percentage of women reporting UI symptoms is within the range reported from other parts of the world. Nevertheless, this high prevalence has not only adverse effects on quality of life, but also has unquestionable impact on health care system. Therefore, it should be considered as a significant threat to women's health and should be a focus of primary preventions. Preventive strategies need our serious attention and are desperately necessary. These strategies can be developed in UI prevention and treatment, medical education, and research.
The findings of this study and others have shown that lifestyle factors, some types of diseases, and child delivery factors are among the main risk factors for UI in women of late adulthood ages. UI has serious impacts on women's health especially on their quality of life in relation to Islamic ethics and practices. Women who suffer from UI problems have difficulties both in physical and psychological well-being aspects. These aspects include: the need to wash and change underwear frequently, the need to use pads, the necessity to drink less liquids, and the necessity to have restricted social activities. Other impacts include embarrassment, avoidance of sexual activity, and reluctance to refer and consult with physicians. The basic concern is that the problem is not generally diagnosed and treated by practitioners; therefore, it remains hidden due to the fact that patients feel ashamed to talk about it with their physicians thinking of it as a normal process of aging which cannot be treated. Therefore, efforts should be made to change this incorrect attitude, and to convince women that their problem is in fact treatable. These efforts include detection and raising awareness of UI women to seek appropriate medical care, and not to be ashamed of their situation. Health care professionals also need to be more educated and trained about UI, and the ways they can be of help to women with this problem. For example, they can give proper advice such as: having a routine daily exercise and pursuing a healthy diet. Education for pelvic floor muscle training has also been shown to help.
Studies such as this explain the indispensable need for more efficient medical education strategies for health care professionals about UI and other pelvic floor dysfunctions. More importantly, health care providers should be informed that women with similar conditions need to be approached with more sensitivity and care.
As a preventive strategy for women's health promotion, it seems that health care providers especially gynecologists and midwives require more attention regarding UI prevention. They need to be especially more trained about the symptoms in young and middle-aged women as well as in the careful detection and management of the symptoms in women suffering from UI. This problem can be detected in history-taking and in medical examination. Routine clinical evaluation in high-risk groups such as older women or women with certain medical conditions is necessary to monitor the incontinence status to assess their treatment and improvement in their quality of life.
Educational programs and more effective medical guidelines for appropriate management of child delivery, advice for improving lifestyle, disease prevention, and treatment programs are also indispensable for UI prevention.
To have a better prevention strategy, we need to go beyond treatment. We must understand how the risk factors such as delivery factors influence PFD and UI in specific groups. However, these injuries, their processes, and the ways they can be prevented would be recognized only through research programs. This is an area where the role of gynecologists, compared to other health care providers, is quite marked. They can make tremendous advances in medical education and research fields which can help in discovering knowledge resulting in improved women's health care.
References
Patel DA, Xu X, Thomason AD, Ransom SB, Ivy JS, DeLancey JOL (2006) Childbirth and pelvic floor dysfunction: an epidemiologic approach to the assessment of prevention opportunities at delivery. Am J Obstet Gynecol 195:23–28
Danforth KN, Townsend MK, Lifford K, Curhan GC, Resnick NM, Grodstein F (2006) Risk factors for urinary incontinence among middle-aged women. Am J Obstet Gynecol 194:339–345
Hannestad YS, Rortveit G, Daltveit AK, Hunskaar S (2003) Are smoking and other lifestyle factors associated with female urinary incontinence? The Norwegian EPINCONT Study. BJOG 110:247–254
Melville JL, Katon W, Delaney K, Newton K (2005) Urinary incontinence in US women a population-based study. Arch Intern Med 165:537–542
Swithinbank LV, Donovan JL, Du Heaume JC, Rogers CA, James MC, Yang Q, Abrams P (1999) Urinary symptoms and incontinence in women: relationships between occurrence, age, and perceived impact. Br J Gen Pract 49:897–900
DeLancey JOL (2005) The hidden epidemic of pelvic floor dysfunction: achievable goals for improved prevention and treatment. Am J Obstet Gynecol 192:1488–1495
Hunskaar S, Lose G, Sykes D, Voss S (2004) The prevalence of urinary incontinence in women in four European countries. BJU Int 93:324–330
Sobhgol SS, Charandabee SMA (2008) Related factors of urge, stress, mixed urinary incontinence and overactive bladder in reproductive age women in Tabriz, Iran: a cross-sectional study. Int Urogynecol J 19:367–373
Safarinejad MR (2009) Prevalence of the overactive bladder among Iranian women based on the International Continence Society definition: a population-based study. Int Urol Nephrol 41:35–45
Jewell NP (2004) Statistics for epidemiology. Chapman & Hall/CRC
Huang AJ, Thom DH, Kanaya AM, Wassel-Fyr CL, Van den Eeden SK, Ragins AI, Subak LL, Brown JS (2006) Urinary incontinence and pelvic floor dysfunction in Asian-American women. Am J Obstet Gynecol 195:1331–1337
Eva UF, Gun W, Preben K (2003) Prevalence of urinary and fecal incontinence and symptoms of genital prolapse in women. Acta Obstet Gynecol Scand 82:280–286
MacLennan AH, Taylor AW, Wilson DH, Wilson D (2001) The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG 56:335
Kapoor DS, Thakar R, Sultan AH (2005) Combined urinary and faecal incontinence. Int Urogynecol J16:321–328
Rizk DEE, Shaheen H, Thomas L, Dunn E, Hassan MY (1999) The prevalence and determinants of health care-seeking behavior for urinary incontinence in United Arab Emirates women. Int Urogynecol J 10:160–165
Moini A, Riazi K, Ebrahimi A, Ostovan N (2007) Caesarean section rates in teaching hospitals of Tehran: 1999–2003. East Mediterr Health J 13:457–460
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahmadi, B., Alimohammadian, M., Golestan, B. et al. The hidden epidemic of urinary incontinence in women: a population-based study with emphasis on preventive strategies. Int Urogynecol J 21, 453–459 (2010). https://doi.org/10.1007/s00192-009-1031-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-1031-6