Abstract
Introduction and hypothesis
The objective of this study is to estimate efficacy of prophylactic antibiotics in UTI prevention during CISC for postoperative voiding dysfunction after prolapse/incontinence surgery.
Methods
We constructed a decision tree model to evaluate risks and benefits of prophylactic antibiotics during CISC for voiding dysfunction after prolapse/incontinence surgery. The model randomized women requiring CISC to prophylactic antibiotics or no prophylaxis. Probabilities for UTI after CISC with or without prophylactic antibiotics, sequelae from antibiotic use or UTI, and utility values were obtained from published literature and practice quality assurance reviews. Main outcome was probability of experiencing no UTI or adverse event.
Results
Under baseline assumptions, prophylactic antibiotics were favored in both models. In the true UTI model, prophylactic antibiotics had an 83.1% probability of no UTI or adverse events; 16.1% better than no prophylactic antibiotics.
Conclusions
Using decision analysis methods, prophylactic antibiotics are favored for prevention of UTI during CISC to manage voiding dysfunction after prolapse/incontinence surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infection (UTI) is the most common complication following surgery for pelvic organ prolapse (POP) and urinary incontinence (UI). Reported rates of postoperative UTI range from 32% to 48% in a recent randomized controlled trial of two anti-incontinence procedures and an analysis of Medicare patients after mid-urethral sling procedures [1, 2]. The high rate of UTI after urogenital tract surgery may not be surprising given the frequent instrumentation of the urinary tract intraoperatively and postoperatively, primarily bladder catheterization during and after surgery and cystoscopy.
Studies suggest that the most significant risk for development of a postoperative UTI is bladder catheterization. Most patients undergoing surgery for POP or UI have an indwelling catheter for some period after surgery. Systemic perioperative antibiotics are protective against development of a postoperative UTI in patients who have their foley catheter removed within 24 h of surgery [3]. Typically, patients will undergo a voiding trial after POP/UI surgery to rule out incomplete bladder emptying or urinary retention. Patients who “fail” the voiding trial require assisted urinary bladder drainage by one of the following methods: a transurethral catheter, a suprapubic catheter, or a clean intermittent self-catheterization (CISC). In the SISTEr trial of Burch procedure versus pubovaginal sling for treatment of incontinence, catheter use for postoperative incomplete bladder emptying increased risk of UTI over twofold [1].
Efficacy of prophylactic antibiotics administered to patients performing CISC after surgery for POP/UI to prevent UTI is unknown. Numerous studies have examined efficacy of prophylactic antibiotics in adults with spinal cord injuries [4–7] and children with neurogenic bladders yielding mixed results [8–10]. To date, no randomized clinical trial of prophylactic antibiotics to prevent UTI during CISC for voiding dysfunction after surgery for POP/UI has been performed.
The objective of this study was to model prophylactic antibiotics versus no antibiotics for prevention of UTI during CISC for voiding dysfunction after POP/UI surgery using decision analysis modeling. We sought to determine the predicted treatment strategy based on estimates from published literature prior to conducting a randomized clinical trial of this clinical scenario.
Materials and methods
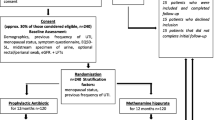
We used standard decision analysis software (TreeAge Pro Suite 2008, TreeAge Software, Williamston, MA, USA) to construct a decision tree model to evaluate risks and benefits of prophylactic antibiotic use during CISC for voiding dysfunction after POP/UI surgery in women. Our base-case analysis took the patient perspective and assessed “harm” versus “no harm” from sequelae of antibiotic use and development of UTI in the first 6 weeks postoperatively. We assessed two clinical scenarios of postoperative UTI diagnosis in models that we named: (1) UTI model—diagnosis of UTI reported in the literature was based on a urine culture (typically defined as a single organism with 106 colony-forming units) and (2) Bacteriuria model—diagnosis of UTI was based on symptoms or an urinalysis suspicious of a UTI (leukocyte esterase “+” and/or nitrite “+”) only. In addition, we performed a utilities-based model using both clinical scenarios. This study received Institutional Review Board approval as an exempt study. We had no external funding for this study.
The model
A schematic diagram of the decision tree model is shown in Fig. 1. We defined our hypothetical study population as adult women performing CISC for voiding dysfunction after POP/UI surgery. “Subjects” were randomized to prophylactic antibiotics versus no antibiotics if they failed their voiding trial after POP/UI surgery and required CISC. Our model assumed nitrofurantoin as first line prophylactic antibiotic and sulfamethoxazole/trimethoprim for any subject unable to take nitrofurantoin. The first branch of the decision tree was randomization for prophylactic antibiotics versus no prophylactic antibiotics. The second branch was the chance of developing a UTI. The subsequent branches account for the possibilities of developing complications both from prophylactic antibiotic exposure as well as from developing a UTI. The last tier of the tree addressed resolution (recovery or death) from possible complications. Each branch point represents a binary outcome (Yes/No) in all models (probability and utility-based models).
Assumptions
The main simplifying assumption of the UTI model was that subjects would present with UTI symptoms, have a urine culture performed, and be treated based on culture results. In the Bacteriuria model, we assumed that subjects would be treated either by symptoms or by simple urinalysis suggestive of a UTI (“positive” leukocyte esterase and “positive” nitrites). In both models, we assumed that the course of events occurred in a linear fashion and there were no recurrences of UTI in the 6-week postoperative period. We also made assumptions that the “resolution” branch of complications occurred completely ending either in full recovery or death. We did not account for long-term disability states that could develop from these complications.
Parameter values
Probabilities and utilities are listed in Table 1. Probabilities for UTI were obtained from published literature and an internal quality assurance review from our clinical practice. Probability values used for complications were either obtained from the published literature or estimated by author consensus. Utilities are represented on a scale from 0 to 1 and were obtained and adapted from Gold et al. [11]. The utility for “no adverse event” was 1.0 and “death” was 0. Utility values for recovery from complications were obtained and adapted from Gold et al. Table 2 “Health State Values Derived for the Health and Activity Limitation Index” (p 782) [11]. This table is originally derived from Erickson et al. [12] and lists utility values for self-rated health categories of “Excellent,” “Very Good,” “Good,” “Fair,” and “Poor” by role limitation categories of “No Limitation,” “Limited, other,” “Limited, major,” “Unable, major,” “Limited, IADL,” and “Limited, ADL.” We assumed that our population was of “Good” health and that the role limitation was estimated by author consensus for the severity of the complication sustained.
Sensitivity analysis
All parameters were varied through ranges listed in Table 1. Both one- and two-way sensitivity analyses were performed. This analysis was performed for both clinical scenarios (UTI and Bacteriuria) and for both “harm” vs. “no harm” and utility-based models.
Results
Results of both clinical scenarios (UTI and Bacteriuria) and both model types (“harm” vs. “no harm” and utility-based models) were similar and only results of the “harm” vs. “no harm” model will be presented. Under baseline assumptions, prophylactic antibiotics were favored in both models and clinical scenarios. In the UTI model, prophylactic antibiotics were associated with an 83.1% probability of no UTI or adverse events, 16.1% better than no prophylactic antibiotics. Prophylactic antibiotics were favored unless the probability of UTI without prophylaxis was <17% (base 33%) or probability with prophylaxis was >32% (base 16%). Using two-way sensitivity analysis for these two parameters, prophylaxis was favored unless the absolute risk of UTI was decreased <1% by prophylaxis (Fig. 2). Results were not sensitive to variation of antibiotic adverse events within clinically plausible ranges. Similar findings were seen in the Bacteriuria scenario as well as utilities-based models.
A two-way sensitivity analysis of Prophylactic Antibiotics vs. No Prophylactic Antibiotics. Two-way sensitivity analysis of the probability of UTI with antibiotic prophylaxis and no antibiotic prophylaxis in the UTI /“harm” vs. “no harm” model. The area of the diamond pattern indicates the probabilities over which the strategy of antibiotic prophylaxis is favored; the area of the square pattern shows the probabilities when the strategy of no antibiotic prophylaxis is favored. As long as the probability of UTI with antibiotic prophylaxis is at least 1% greater than probability of UTI without antibiotic prophylaxis, antibiotic prophylaxis is favored
We calculated a number needed to treat (NNT) to estimate the effectiveness of prophylactic antibiotics during clean intermittent self-catheterization based on the results of this model. The NNT estimates how many patients would need to be treated to prevent one bad additional outcome. From this model, seven patients would need to be treated with prophylactic antibiotics to prevent one additional bad outcome in the model.
Next, we ran the model with the utility value for lower UTI (Lower UTI) = 1; treating this event as clinically “trivial.” A variable with a utility value of 1 will not have an effect on utility model outcomes. If lower UTI is treated as a “trivial” event, then the “No Prophylaxis” arm would be only slightly favored (No Prophylactic Antibiotics = 0.985 vs. Prophylactic Antibiotics = 0.983). We believe that lower UTI is not a trivial event and can lead to significant pain and discomfort as well as lead to serious systemic illness.
Discussion
The most important finding of this study is that use of prophylactic antibiotics in women performing CISC for voiding dysfunction after POP/UI was favored for the prevention of UTI in a decision analysis model. Since a randomized clinical trial of prophylactic antibiotics for this scenario has not been performed, decision analysis modeling allows us to estimate the outcomes of a trial based on reported occurrences of events such as UTI or complications. Sensitivity analysis allows us to evaluate the model through all clinically plausible ranges of probabilities, verifying a robust model and results.
In addition to estimating results of this clinical scenario from the published literature, we are using this model to “predict” the outcomes and evaluate the value of a clinical trial of prophylactic antibiotics in our population of POP/UI surgical patients prior to actually performing the study. Decision analysis modeling can help us detect particular issues or potential complications to be aware of prior to the actual clinical study. From this model, we believe that complications from prophylactic antibiotics will not be a limiting factor in evaluating true clinical usefulness of antibiotics in this scenario.
As mentioned, UTI is the most common complication following surgery for POP/UI. With rates reported between 32–48%, it makes clinical sense to evaluate treatment strategies to prevent development of UTI, especially in an at risk population due to required catheter use [1, 2]. UTI can cause both minor bothersome symptoms such as dysuria and frequency as well as serious sequelae such as pyelonephritis and septicemia. It has been estimated that bacteriuria can progress to UTI in 25% of cases and bacteremia in 1–4% [13]. Catheter-related infections carry an almost threefold risk of mortality even when controlling for comorbid conditions [14]. Prevention of UTI in patients performing CISC would significantly reduce morbidity and potentially, although rare, mortality.
UTI prevention with use of a catheter is difficult because indwelling transurethral and suprapubic catheters develop and extraluminal and intraluminal biofilm, an amalgamation of microbial organisms that produce a surrounding extracellular matrix consisting primarily of polysaccharide materials [15, 16]. It is likely that catheters used for CISC develop a similar biofilm over the course of use. While CISC catheters are not continuously indwelling, they are typically used multiple times a day and up to 1 week before disposal. Antimicrobials are often unsuccessful in eradicating this biofilm because the extracellular matrix resists diffusion of the drug [15, 16]. The biofilm can spread to the bladder surface and can grow thick enough to obstruct the lumen on the catheter [15]. It is standard of care to teach the patient “clean” and family members “sterile” technique for performing catheterization to prevent bacterial inoculation. Other preventative measures that are often used include acidification of the urine and the use of silver-coated catheters.
Perioperative intravenous antibiotics have been shown to be beneficial in reducing catheter-associated bacteriruia [17–19] and preventing symptomatic UTI in catheterized patients within the first 24 h after abdominal hysterectomy [20]. However, daily oral prophylactic antibiotic use for prevention of catheter-associated UTI is very controversial [21], and the prolonged use of prophylactic antibiotics in catheterized patients carries both potential risks and benefits. Gribble et al. found that sulfamethoxazole/trimethoprim (SMX/TMP) decreased bacteriuria and UTI rates in patients performing CISC [4]. However, Mohler et al. found no difference in bacteriuria or UTI rates between patients performing CISC and randomized to either SMX/TMP versus placebo [5]. Duffy et al. compared nitrofurantoin prophylaxis with placebo in a double-blind crossover study and found a decrease in development of bacteriuria but no effect on UTI [6]. In a POP/UI surgical population, Rogers et al. found that nitrofurantoin reduced the incidence of both symptomatic UTI and positive urine cultures in women with a suprapubic catheter placed intraoperatively for management of postoperative voiding dysfunction [22].
Nitrofurantoin is generally a well-tolerated, relatively inexpensive, and effective antibiotic, which makes it a good candidate for a prophylactic agent. The most common adverse reactions are nausea, headache, and flatulence [23]. Rare serious reactions such as chronic pulmonary reactions, hepatic injury, and peripheral neuropathy can occur in patients on long-term (typically >6 months) nitrofurantoin therapy [23, 24]. Potential hypersensitivity or allergic reactions to nitrofurantoin include rash, angioedema, and anaphylaxis, all of which can be severe [23–25].
There are several limitations to our study. Decision analyses are useful in guiding clinical decisions when there is a paucity of good clinical information. Decision analytic models are based on parameter estimates obtained from the medical literature or, in the absence of evidence, estimated within reasonable clinical bounds. The results of a model could be questioned as unreliable if key elements cannot be estimated by robust evidence. Sensitivity analyses are very valuable in identifying variables of key interest if they influence the results of the model. Conversely, sensitivity analyses can provide reassurance that the probabilities, even in only estimated by consensus, do not affect the results of the model. In our model, the key variables identified through sensitivity analyses were derived from the medical literature and parameter estimates derived by consensus did not have an effect on the results of the model. Overuse of antibiotics is a ubiquitous problem, and it has been estimated that 75% of the western world’s use of antimicrobials may be unnecessary [26]. Recommendations have been made to substantially decrease the use of unnecessary antibiotics [27]. Because antibiotic resistance and antibiotic-associated morbidity and mortality are realities; we believe prophylactic use of antibiotics should be based on medical evidence. In the absence of, or prior to, the results of clinical trials, medical decision analysis methods allow us to support our clinical decisions based on available evidence.
References
Albo ME, Richter HE, Brubaker L, Norton P, Kraus S, Zimmern PE et al (2007) Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med 356:2143–2155
Anger JT, Litwin MS, Wang Q, Pashos CL, Rodriguez LV (2007) Complications of sling surgery among female medicare beneficiaries. Obstet Gynecol 109:707–714
Niel-Wise BS, van den Broek PJ (2006) Antibiotic policies for short-term catheter-bladder drainage in adults. Cochrane Database Syst Rev 4:1–17
Gribble MJ, Puterman ML (1993) Prophylaxis of urinary tract infection in persons with recent spinal cord injury. Am J Med 95:141–152
Mohler JL, Cowen DL, Flanigan RC (1987) Suppression and treatment of urinary tract infection in patients with an intermittently catheterized neurogenic bladder. J Urol 138:336–340
Duffy L, Smith AD (1982) Nitrofurantoin macrocrystals prevent bacteriuria in intermittent self-catheterization. Urology 20:47–49
Bakke A, Vollset SE (1993) Risk factors for bacteriuria and clinical urinary tract infection in patients treated with clean intermittent catheterization. J Urol 149:527–531
Clarke SA, Samuel M, Boddy SA (2005) Are prophylactic antibiotics necessary with clean intermittent catheterization? A randomized controlled trial. J Ped Surg 40:568–571
Johnson HW, Anderson JD, Chambers GK, Arnold WJD, Irwin BJ, Brinton JR (1994) A Short-term study of nitrofurantoin prophylaxis in children managed with clean intermittent catheterization. Pediatrics 93:752–755
Schlager TA, Anderson S, Trudell J, Hendley JO (1998) Nitrofurantoin prophylaxis for bacteriuria and urinary tract infection in children with neurogenic bladder on intermittent catheterization. J Pediatr 132:704–708
Gold MR, Franks P, McCoy KI, Fryback DG (1998) Toward consistency in cost-utility analyses: using national measures to create condition-specific values. Medical Care. 36(6):778–792
Erickson P, Wilson R, Shannon I (2000) Years of healthy life. Healthy People 2000 Statistical Notes. National Center for Health Statistics, Hyattsville
Saint S, Chenowith CE (2003) Biofilms and catheter-associated urinary tract infections. Infect Dis Clin N Am 17:411–432
Platt R, Polk F, Murdock B, Rosner B (1982) Mortality associated with nosocomial urinary-tract infection. N Engl J Med 307:637–642
Liedl B (2001) Catheter-associated urinary tract infections. Curr Opin Urol 11:75–79
Trautner BW, Darouiche RO (2004) Catheter-associated infections. Arch Intern Med 164:842–850
Britt MR, Garibaldi RA, Miller WA, Hebertson RM, Burke JP (1977) Antimicrobial prophylaxis for catheter-associated bacteriuria. Antimicrob Agents Chemoter 11:240–243
Shapiro M, Simchen E, Izraeli S, Sacks TG (1984) A multivariate analysis of rsik factors for acquiring bacteruria in patients with indwelling urinary catheters for longer than 24 hours. Infect Control 5:525–532
Van Der Wall E, Verkooyen RP, Mintjes-de Groot J, Oostinga J et al (1992) Prophylactic ciprofloxacin for catheter-associated urinary-tract infection. Lancet 339:946–951
Jaffe R, Altaras M, Fejgin M, Ben-Aderet N (1985) Prophylactic single-dose co-trimoxazole for prevention of urinary tract infection after abdominal hysterectomy. Chemotherapy 31:476–479
Niel-Wise BS, van den Broek PJ (2005) Urinary Catheter policies for long-term catheter-bladder drainage. Cochrane Database Syst Rev 1:1–26
Rogers RG, Kammer-Doak D, Olsen A, Thompson PK, Walters MD, Lukcz ES, Qualls C (2004) A randomized, double-blind, placebo-controlled comparison of the effect of nitrofurantoin monohydrate macrocrystals on the development of urinary tract infections after surgery for pelvic organ prolapse and/or stress urinary incontinence with suprapubic catheterization. Am J Obstet Gynecol 191:182–187
Guay DR (2001) An update on the role of nitrofurans in the management of urinary tract infections. Drugs 61:353–364
Shah RR, Wade G (1989) Reappraisal of the risk/benefit of nitrofurantoin: Review of toxicity and efficacy. Adverse Drug React. Acute Poisoning Rev 8:183–201
Davey R (1986) Macrodantin: A Cautionary tale. The Medical Journal of Australia 145:476–477
Wise R, Hart T, Cars O, Streulens M et al (1998) Antimicrobial resistance: Is a major threat to public health. BMJ 317:609–610
Schwartz B, Bell DM, Hughes JM (1997) Preventing the emergence of antimicrobial resistance: A Call for action by clinicians, public health officials, and patients. JAMA 278:944–945
Dobbs SP, Jackson SR, Wilson AM, Maplethorpe RP, Hammond RH (1997) A prospective, randomized trial comparing continuous bladder drainage with catheterization at abdominal hysterectomy. Br J Urol 80:554–556
Naik R, Maughan K, Nordin A, Lopes A, Godfrey KA, Hatem MH (2005) A prospective randomized controlled trial of intermittent self-catheterisation vs. supra-pubic catheterization for post-operative bladder care following radical hysterectomy. Gynecologic Oncology 99:437–442
Jannelli ML, Wu JM, Plunkett LW, Williams KS, Visco AG (2007) A randomized controlled trial of clean intermittent self-catheterization versus suprapubic catheterization after urogynecologic surgery. Am J Obstet Gynecol 197:72.e1–72.e4
Schiotz HA, Tanbo TG (2006) Postoperative voiding, bacteriuria and urinary tract infection with Foley catheterization after gynecological surgery. Acta Obstetricia et Gynecologica 85:476–481
Schiotz HA, Guttu K (2002) Value of urinary prophylaxis with methenamine in gynecologic surgery. Acta Obstet Gynecol Scand 81:743–746
Lowder JL, Burrows LJ, Howden NLS, Weber AM (2007) Prophylactic antibiotics after urodynamics in women: a decision analysis. INt urogynecol J 18:159–164
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sutkin, G., Lowder, J.L. & Smith, K.J. Prophylactic antibiotics to prevent urinary tract infection during clean intermittent self-catheterization (CISC) for management of voiding dysfunction after prolapse and incontinence surgery: a decision analysis. Int Urogynecol J 20, 933–938 (2009). https://doi.org/10.1007/s00192-009-0885-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-0885-y