Abstract
Introduction
A study was performed to determine which patients’ characteristics before tension-free vaginal tape (TVT) for stress incontinence are predictive of a failed outcome.
Methods
A prospective cohort of 305 women with urinary stress incontinence underwent a TVT procedure in a teaching hospital. TVT was considered successful when the patient was fully satisfied and no leakage was seen at the standardized stress test. Logistic regression analysis examined the relationship between outcome and 32 pre-, intra-, and postoperative patient characteristics. All operations were done by trainees under supervision and assistance.
Results and conclusions
Eighty one percent was successfully treated. Independent predictors of TVT failure were previous surgery for incontinence (P = 0.006), >2 pads/diapers per day before treatment (P = 0.012), chronic use of psychotropic medication (P = 0.012), and a more advanced age of the patient (P = 0.005). Postoperative urgency was independently related to preoperative urgency (P < 0.001). Independent predictors of postoperative dissatisfaction were urgency symptoms (P < 0.001) and the need for a re-intervention (P < 0.001).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence is the most common form of incontinence affecting women [1, 2]. In 1995, Ulmsten and Petros described a sub-urethral sling procedure whose effects mimic those of the functionally intact vaginal hammock and pubo-urethral ligament, thereby restoring support and achieving closure of the urethra when intra-abdominal pressure increases [3]. This tension-free vaginal tape (TVT) procedure, whereby a thin polypropylene mesh tape is placed directly under the mid-uretha, is as effective as the open colposuspension [4, 5]. It causes less morbidity and is cost effective when compared to the Burch colposuspension [6]. Therefore, the tension-free sling procedure has become the gold standard. More than 700 peer-reviewed articles about TVT have been published and, some months ago, the manufacturer of the tape announced that 1 million TVT procedures had been performed worldwide.
Despite the abundant literature pertaining to the subject, clinical trials assessing factors predictive of therapy response and articles about teaching TVT to trainees are rather few. The main purpose of this study was to determine, in a hospital where trainees perform the procedures, which patients’ characteristics predict failure of the TVT.
Patients and methods
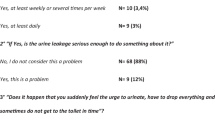
Between 1 January 2000 and 31 December 2005, 305 women with urinary stress incontinence who had a TVT (Gynecare Inc, Ethicon) were included in the study. Preoperatively, the patients’ main complaint was a urinary stress incontinence which they experienced as a social or hygienic nuisance and which was objectively demonstrated by urodynamics. All women had a bladder capacity of at least 300 ml and a residual urine volume after micturition of less than 100 ml. Sixteen women who had also undergone a TVT during the study period were excluded either because they suffered from a neurological disease, were demented or institutionalized (n = 10), or because they had not shown up at the first postoperative visit (n = 6). Before surgery, all patients had a standardized questionnaire, a cystometry (to exclude an overactive bladder), and a stress test. The latter was proceeded as follows: the woman, who was sitting upright, was instructed to cough vigorously after 300 ml of fluid had been instilled into the empty bladder and the catheter had been removed. Involuntary leakage from the urethra synchronous with coughing was diagnostic for a positive stress test [2]. Distinction was made between leakage on the first cough or after repetitive coughing. A flowmetry completed the urodynamics. ‘Urgency’ was considered as a sudden desire to void with a fear of leakage but without loss of urine. Before therapy, the patient recorded the use of pads. Pad use and cough tests were not test–retested by us. Others have found those outcome measures to be reliable, reproducible, and appropriate for clinical trials [7, 8].
All operations were performed by trainees in either gynecology (n = 14) or urology (n = 7) under the supervision and the assistance of a single uro-gynecologist. The TVT technique we applied was that of professor Ulmsten’s [6] except that we used regional or general instead of local anesthesia. A cystoscopy was carried out during the procedure immediately after the retropubic insertion of both trocars. Postoperative voiding dysfunction was defined as a post voiding residual urine volume of more than 100 ml, requiring prolonged transurethral, suprapubic, or intermittent self-catheterization.
The patients were then seen 2 months after surgery; a standardized history was taken, the bladder filled (300 ml), and a stress test followed by a flowmetry was performed. Cystometry was executed in women with de novo urgency. The patients’ assessment was carried out by the first author with the aid of a continence nurse.
Successful therapy was defined as a truly satisfied woman (i.e., ‘urinary incontinence is no longer a problem and further treatment is not warranted’) and a negative stress test at follow-up. All other situations (satisfied with positive stress test, unsatisfied with either negative or positive stress test) were considered to be failures. Then, women were seen again, 1 year after surgery.
The continuous variables, pertaining to the patients, were compared with the Student t test and the non-parametric Mann–Whitney U test. Categorical variables were compared with chi-square tests (Pearson with continuity correction, Fisher exact test). The level of statistical significance was set at a probability value of <0.05. Interrelations between risk factors were assessed with forward stepwise logistic regression analysis, with a threshold of 5% for the inclusion of additional prediction into the model.
Results
Of the 305 women who were included, 59 (19%) did not meet the criteria for a successful outcome; 24 of these, though they had a positive stress test after the TVT, were nevertheless satisfied, the incontinence substantially being reduced to an acceptable degree. The remaining 35 women were not satisfied; 16 of them had a positive stress test and 19 a negative one. Reasons for not being satisfied in this latter group were the presence of disturbing urgency (13×), persistent voiding difficulties (4×), and persistent pain suprapubic or in the groin (2×).
Baseline characteristics of the successfully treated women were compared with those in whom therapy had failed (Table 1). Older women, housewives, those with a history of urological or gynecological surgery, those taking medication for cardiovascular or psychic ailments, and those with a more severe incontinence (pads use/cough test) were significantly less often successfully treated (Table 1). The highest level of success was achieved in women who, before TVT, did not leak at first cough (91% success) or did not use a protective garment daily (88% success). The lowest success rates were seen in women who had an immobile (scarred) urethra on Q tip (45% success) or who had a history of suprapubic anti-incontinence surgery (51% success). Women who, before TVT, had to wear diapers or more than two pads per day as well as those who had urgency symptoms before surgery were also less successfully treated (60% and 64% success, respectively).
Bladder perforation occurred 47 times in 41 women (14%). In six women, perforation was bilateral. Seventeen women had a bladder injury on the right and 18 on the left side. Most perforations (74%) complicated placement of the second trocar, the first one being in situ and 61% (n = 25) of the perforations occurred during the trainees’ first five operations. There were no differences in perforation rate between gynecological and urological trainees. We did not prolong bladder drainage after perforation but, when bleeding occurred after removal of the perforating trocar, we irrigated the bladder before reinserting the trocar. Logistic regression analysis showed that the body mass index was the only patient-related risk factor which predicted accidental bladder perforation (OR 0.89; 95% CI 0.82–0.96, p < 0.005). Not one suprapubic catheter was placed during the TVT procedure.
Hospital stay was limited to one day in 248 women (81%). Reasons for prolonged hospitalization (>1 day) were concomitant vaginal surgery (n = 25), voiding dysfunction (n = 20), retropubic hematoma (n = 4; surgical drainage was required in one case), a hematoma in the posterior compartment after posterior repair that necessitated drainage and blood transfusion (n = 1), pain in the groin (n = 3), heart failure (n = 1), social reasons (n = 2), and a suspected compartment syndrome of the leg (n = 1).
Maximal flow rate was significantly lower after TVT which means that the procedure also causes some obstruction (Table 1). Immediate voiding dysfunction occurred in 28 women (9.2%) of whom 12 received a suprapubic catheter and two applied intermittent self-catheterization. Four women were re-admitted shortly after being discharged for urinary retention (n = 2), wound abscess (n = 1), or suprapubic catheter complication (n = 1). Seven women needed re-admission at a later moment (all <3 months after TVT placing) for trans-vaginal cutting (n = 5) or readjusting (n = 2) of the tape due to obstructed voiding, urge, and/or micturition pain. None of these seven women, in whom tension of the tape was released, became stress incontinent again. Remarkably, all but one tape releases were performed in the first 50 women who were operated upon. For later TVT procedures for patients under spinal anesthesia, we no longer applied the cough-stress test. No patient experienced long-term voiding difficulty but for one who continued to resort to self-catheterization intermittently.
Before therapy, 88 women had complained of urgency (Table 1). At the first postoperative visit, 29 of these (33%) still had urgency. Twelve women (5.5%) developed de novo urgency of which five showed detrusor overactivity.
Hospital stay and intra- or postoperative complications had no influence on success or failure of the TVT procedure (Table 1).
Up to now, we are not aware of any tape erosion in this series.
Because baseline characteristics influence each other, we carried out a stepwise logistic regression analysis (Table 2). Four independent predictors were found. There is a poorer outcome with TVT in case of previous surgery for incontinence, use of more than two pads or diapers per day before TVT, and psychotropic drug therapy or increasing age (Table 2). Logistic regression showed that preoperative urgency (P < 0.001) and increasing age (P = 0.009) were independent predictors for having urgency at follow-up evaluation. The postoperative patients’ dissatisfaction was, according to logistic regression analysis, more strongly related to urgency (P < 0.001) and to the necessity of re-intervention (P < 0.001) than to psychotropic medication (P = 0.064).
Unsatisfied women were mainly treated with PFMT (stress/urge) and/or with anti-cholinergic drugs (urge). At 1-year follow-up, of those who were cured, 94% remained that way, with minor leakage being experienced by 6%.
Discussion
Overall, our success rate is in line with that mentioned in a meta-analysis of the literature [9]. Our specific purpose, however, was to identify clinical factors that influenced TVT outcome in a teaching setting where all procedures are performed by supervised trainees. The severity of symptoms, expressed by a greater number of pads used, was a significant predictor of a poorer outcome. The presence of an immobile urethra and previous surgery for incontinence, both of which often are associated with more severe incontinence, were also predictors of a less favorable outcome. More severe incontinence is seen in intrinsic urethral sphincter deficiency, which is the consequence of urethral sphincter damage with scarring and denervation. Other studies [10–12] analyzed risk factors for failure and gave similar results. Lee et al. [10], who assessed 138 TVT procedures carried out on South Korean women, found that those with severe incontinence, a low urethral pressure, and a high BMI had a lower cure rate. Meschia et al. [11], studying 325 consecutive Italian patients, associated TVT failure with a low urethral mobility and with recurrent stress incontinence, both being manifestations of urethral damage. A study from Japan [12] including 151 women revealed that the TVT operation had a significantly lower cure rate in women with an immobile, low pressure urethra. However, TVT outcome in 703 Swedish incontinent women was only influenced by the type of incontinence; in women with mixed symptoms, the cure rate was 55% compared to 81% in women with genuine stress incontinence [13]. A Dutch multi-center study [14], comprising 809 patients, showed that the inexperience of the surgeon with the TVT procedure and general anesthesia had a small, though significant, negative effect on the outcome. Finally, another Dutch study of 198 TVT procedures was unable to demonstrate any factor that influenced outcome [15].
We found that the cure rate decreased with every increase by 10 years of the age of the women. This is in line with a Swedish study of 970 patients [16]. Older women possibly have a higher prevalence of chronic disease such as diabetes and COPD or of chronic constipation. Others found similar [17, 18] cure in elderly women compared to younger ones. Therefore, nobody doubts that the TVT procedure is still worthwhile in elderly women [16–18].
This is the first study to report that, in this setting, women taking antidepressant or anxiolytic drugs had a lower chance of being cured. Women on psychotropic medication had a lower cure rate, presumably because they objectively failed (i.e., had a positive stress test) and not because they were dissatisfied. Yet, in women who were treated by PFMT, the same was found [19]. Here, a low adherence to therapy was responsible for the less favorable results [19].
Becoming fully continent after TVT is not synonymous with being satisfied. A number of operated women still leaked postoperatively but were satisfied. These were mostly women with severe incontinence who experienced substantial improvement, the incontinence being reduced to an acceptable degree. This corroborates the finding that women can cope with a certain degree of incontinence for which therapy is not warranted [20]. On the contrary, a number of women who had become continent were not satisfied at all, mainly because of urgency. Likewise, in a South Korean multi-center study [10], urgency was the only factor predictive of patients’ satisfaction at 5-year follow-up. In a study from California, dissatisfied patients either tended to have overactive bladder symptoms or voiding difficulties, or they required sling release [21], much the same as what we found. In brief, postoperative urgency is as bothersome for the patient as the preoperative urinary stress incontinence [22].
The complications of TVT surgery we encountered in our study are comparable with those reported in the literature [9, 23] except for the incidence of bladder perforation. We had 14% perforations. In a meta-analysis of 2,379 TVT placements, bladder perforation occurred in 4.7% and a perforation rate of more than 10% is barely reported [9] except during the learning phase of the procedure. Lebret et al. [24] found that six senior surgeons perforated the bladder in 22% of the first 50 TVT procedures but in only 6% of the second 50. Undoubtedly, there is a learning curve as the incidence of bladder perforation decreases with increasing surgical experience [23–27]. Not surprisingly, there is a higher than expected perforation rate in hospitals where trainees carry out the TVT operations [25, 26]. The rate of bladder perforation was 34% in a US teaching hospital where 23 residents performed the TVT procedures [25]. In another US study of TVT surgery done by residents in training, accidental cystotomy supervened in 14% of the cases [26]. McLennan and Melick noticed that 37% of the perforations were missed on cystoscopic inspection by the residents [25]. We did not register the number of perforations that were missed but observed that trainees in gynecology missed a perforation mainly due to their inexperience in interpreting cystoscopy. Trainees in urology missed perforations mainly because they tended to judge too quickly before the bladder mucosa was completely unfolded. However, these observations were speculative since they were not based on a chart review. In our series, the BMI was inversely related to the risk of bladder perforation. This was an unexpected finding for which we have no explanation even though others [25] made the same observation. Our study showed that cystotomy did not negatively affect the TVT outcome, confirming similar conclusions from studies conducted in the USA and Israel [26, 28].
Finally, we found that tape release for refractory voiding difficulty was also related to a learning curve since six out of seven releases pertained to the first 50 patients. In a French study [24], dysuria and urinary retention more frequently affected the first 50 patients (20%) than the 50 operated on thereafter (6%).
Methodological strengths of our study include its prospective design, the consecutive recruitment within a limited time frame of unselected women complaining of urinary stress incontinence, the relatively large sample size, and the small number of patients lost to follow-up. Our study would certainly be strengthened by the use of a comparison group, either by surgeon (trainee versus attending or urologist versus gynecologist) or by source population (this patient group versus a community-based population).
The cure rate of 305 women with stress incontinence who underwent a TVT procedure by trainees under supervision is eight out of ten. The cure rate of stress incontinence after TVT is substantially lower with a greater severity of incontinence (reflecting the level of urethral damage), with increasing age and with chronic use of psychotropic drugs. Patients’ dissatisfaction is mainly caused by postoperative urgency. Due to a learning curve, bladder perforation is more frequent than generally reported in the literature. We use these data to realistically inform our patients.
Abbreviations
- TVT:
-
Tension-free vaginal tape
- PFMT:
-
Pelvic floor muscle exercises
References
Brocklehurst JC (1993) Urinary incontinence in the community: analysis of a Mori poll. BMJ 306:832–834
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al (2002) Standardization of terminology of lower urinary tract function. Neurourol Urodyn 21:167–178
Ulmsten U, Petros P (1995) Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol 29:75–82
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7:81–86
Ward K, Hilton P (2002) United Kingdom and Ireland Tension-free Vaginal Tape Trial Group. Prospective multicentre randomised trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ 325:67
Wu JM, Visco AG, Weidner AC, Myers ER (2007) Is Burch colposuspension ever cost-effective compared with tension-free vaginal tape for stress incontinence? Am J Obstet Gynecol 197:62.e1–62.e5
Groutz A, Blaivas JG, Chaikin DC, Resnick NM, Engleman K, Anzalone D et al (2000) Noninvasive outcome measures of urinary incontinence and lower urinary tract symptoms: a multicenter study of micturition diary and pad tests. J Urol 164:698–701
Swift SE, Yoon EA (1999) Test–retest reliability of the cough stress test in the evaluation of urinary incontinence. Obstet Gynecol 94:99–102
Parsons M, Cardozo L (2005) The use of TVT for urodynamic stress incontinence. The evidence for urology, edited by C. Dawson & G. Muir. TFM Publishing: Shrewsbury, UK, 241–252
Lee K-S, Choo M-S, Doo CK, Han D-H, Lee Y-S, Kim JY, Kim WS, Jung HC (2007) The long term (5-years) objective TVT success rate does not depend on predictive factors at multivariate analysis. A multicentre retrospective study. Eur Urol 53:176–183
Meschia M, Pifarotti P, Gattei U, Bertozzi R (2007) Tension-free vaginal tape: analysis of risk factors for failures. Int Urogynecol J 18:419–422
Ohkawa A, Kondo A, Takei M, Gotoh M, Ozawa H, Kato K et al (2006) Tension-free vaginal tape surgery for stress urinary incontinence: a prospective multicentered study in Japan. In J Urol 13:738–742
Ankardal M, Heiwall B, Lausten-Thomsen N, Carnelid J, Milsom I (2006) Short- and long-term results of the tension-free vaginal tape procedure in the treatment of female urinary incontinence. Acta Obstet Gynecol Scand 85:986–992
Schraffordt Koops SE, Bisseling TM, van Brummen HJ, Heintz AP, Vervest HA (2006) What determines a successful tension-free vaginal tape? A prospective multicenter cohort study: results from The Netherlands TVT database. Am J Obstet Gynecol 194:65–74
Withagen MI, Milani AL (2007) Which factors influenced the result of a tension-free vaginal tape operation in a single teaching hospital? Acta Obstet Gynecol Scand 86:1136–1139
Hellberg D, Holmgren C, Lanner L, Nilsson S (2007) The very obese woman and the very old woman: tension-free vaginal tape for the treatment of stress urinary incontinence. Int Urogynecol J 18:423–429
Pugsley H, Barbrook C, Mayne CJ, Tincello DG (2005) Morbidity of incontinence surgery in women over 70 years old: a retrospective cohort study. BJOG 112:786–790
Walsh K, Generao SE, White MJ, Katz D, Stone AR (2004) The influence of age on quality of life outcome in women following a tension-free vaginal tape procedure. J Urol 171:1185–1188
Cammu H, Van Nylen M, Blockeel C, Kaufman L, Amy JJ (2004) Who will benefit from pelvic floor muscle training for stress urinary incontinence? Am J Obstet Gynecol 191:1152–1157
Jolleys JV (1988) Reported prevalence of urinary incontinence in women in a general practice. Br Med J 296:1300–1302
Davis TL, Lukacz ES, Luber KM, Nager CW (2004) Determinants of patient satisfaction after the tension-free vaginal tape procedure. Am J Obstet Gynecol 191:176–181
Holmgren C, Nilsson S, Lanner L, Hellberg D (2007) Frequency of de novo urgency in 463 women who had undergone the tension-free vaginal tape (TVT) procedure for genuine stress urinary incontinence—a long-term follow-up. Eur J Obstet Gynecol Reprod Biol 132:121–125
Abouassaly R, Steinberg JR, Lemieux M, Marois C, Gilchrist LI, Bourque J-L et al (2004) Complications of tension-free vaginal tape surgery: a multi-institutional review. BJU Int 94:110–113
Lebret T, Lugagne PM, Hervé JM, Barré P, Orsani JL, Yonneau L et al (2001) Evaluation of tension-free vaginal tape procedure. Its safety and efficacy in the treatment of female stress urinary incontinence during the learning phase. Eur Urol 40:543–547
McLennan MT, Melick CF (2005) Bladder perforation during tension-free vaginal tape procedures. Analysis of learning curve and risk factors. Obstet Gynecol 106:1000–1004
LaSala CA, Schimpf MO, Udoh E, O’Sullivan DM, Tulikangas P (2006) Outcome of tension-free vaginal tape procedure when complicated by intraoperative cystotomy. Am J Obstet Gynecol 195:1857–1861
Schraffordt Koops SE, Bisseling TM, Heintz AP, Vervest HA (2005) Prospective analysis of complications of tension-free vaginal tape from The Netherlands Tension-free Vaginal Tape Study. Am J Obstet Gynecol 193:45–52
Gold RS, Groutz A, Pauzner D, Lessing J, Gordon D (2007) Bladder perforation during tension-free vaginal tape surgery: does it matter? J Reprod Med 52:616–618
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cammu, H., Van Den Abbeele, E., Nagel, H. et al. Factors predictive of outcome in tension-free vaginal tape procedure for urinary stress incontinence in a teaching hospital. Int Urogynecol J 20, 775–780 (2009). https://doi.org/10.1007/s00192-009-0851-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-0851-8