Abstract
This study aimed to evaluate the responsiveness of the electronic Personal Assessment Questionnaire-Pelvic Floor (ePAQ-PF) in women undergoing surgery for pelvic floor disorders. Fifty-four women undergoing tension-free vaginal tape (TVT) and 47 women undergoing prolapse surgery completed ePAQ-PF at baseline and 3 months postoperatively. Responsiveness was calculated using effect sizes, standardized response means, responsiveness statistic, and minimally important difference. In the TVT group, the largest effect sizes were seen in the urinary domains for stress urinary incontinence (2.4), quality of life (2.2), and overactive bladder (0.9). In the prolapse group, the largest effect sizes were seen in the vaginal domains for prolapse (2.1) and quality of life (1.0). ePAQ-PF is responsive to change in women undergoing TVT or prolapse surgery in the salient and expected domains of stress incontinence and prolapse and quality of life and can be recommended for outcome measurement in this context.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorders encompass a broad spectrum of conditions relating to urinary, bowel, vaginal, and sexual function. Although generally benign, these conditions often impact substantially on women’s quality of life. Two of the most common conditions are urinary incontinence and vaginal prolapse, which can lead to embarrassment, low self-esteem, and poor body image [1]. Many women avoid physical and social activities and sexual intimacy and report loss of self-control and independence as well as sexual and relationship problems [2–3]. The accurate assessment and measurement of symptoms relating to pelvic floor disorders is essential for clinical diagnosis and monitoring of outcome [4]
The electronic Personal Assessment Questionnaire-Pelvic Floor (ePAQ-PF) was designed to measure symptoms and their impact upon quality of life in women with pelvic floor disorders. It was originally developed following a period of data collection using a battery of paper questionnaires. This proved burdensome and unrewarding for patients and clinicians in routine practice and the chore of manual data entry prompted the development of an interactive electronic system, allowing direct database entry via a touch-screen computer interface. The original 14-domain version underwent psychometric testing in primary and secondary care, where it was found to be valid, reliable, and acceptable [5]. Since this initial validation study, a further five domains have been added (irritable bowel, dyspareunia, vaginal capacity, urinary voiding, and general sex life). Recent tests of data quality on this version of ePAQ-PF supported its 19 domain structure, reliability, and validity [6].
Responsiveness is an essential quality of any health-related quality-of-life (HRQOL) measure and refers to the ability of an instrument to detect change over time. When used to measure health status before and after change, responsiveness is a reflection of how well the differences between questionnaire scores reflect the true change that has occurred [7]. It also provides evidence of an instruments validity as it should confirm that anticipated responses arise in accordance with corresponding changes in health [8].
The responsiveness of an instrument is ideally evaluated using a therapy of known effectiveness [8–9]. Tension-free vaginal tape (TVT) for the treatment of stress incontinence and surgical repair of prolapse are two of the most frequently carried out urogynecological procedures, both having good evidence of efficacy [10–13]. The TVT is currently the most popular surgical procedure and, along with its derivatives, has largely replaced colposuspension for primary incontinence surgery.
The aim of this study was to establish the responsiveness of ePAQ-PF in women undergoing surgical treatment of incontinence and prolapse and thereby determine the suitability of the instrument as an outcome measure in this context.
Materials and methods
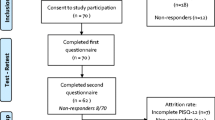
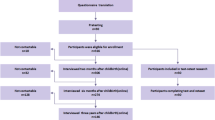
Fifty-four women undergoing TVT and 47 undergoing prolapse surgery were included in the study. In order to provide sufficient data for analysis, all prolapse surgical data were included in the sample. The prolapse procedures performed in this study included anterior repair (n = 13), anterior repair and vaginal hysterectomy (n = 12), anterior repair + posterior repair (n = 5), posterior repair (n = 9), posterior repair + sacrospinous fixation (n = 3), abdominal sacrocolpopexy (n = 2), and vaginal hysterectomy (n = 1). Women undergoing combined prolapse and incontinence surgery were excluded to avoid contamination.
ePAQ-PF is routinely administered to patients attending the Urogynecology Unit of the Jessop Wing, Sheffield Teaching Hospitals NHS Foundation Trust. Patients completed the questionnaire using a touch-screen computer as part of their initial assessment and again on attending for follow-up 3 months postsurgery. The final two items in the questionnaire seek consent for data to be used: (1) for service evaluation “Are you willing to allow confidential use of your answers in order to evaluate the care you receive?” yes/no and (2) for questionnaire evaluation “Are you willing to allow confidential use of your answers to check how this questionnaire is working?” yes/no. Only women who answered in the affirmative to both items on both ePAQ-PF completions were included in the analysis.
Statistical analyses
ePAQ-PF comprises four dimensions: urinary, bowel, vaginal, and sexual. These dimensions consist of 35, 33, 22, and 28 items, respectively. Within each dimension are four to five scored domains, each comprising three to seven items. All items included in a domain are scored between 0 and 3 (0 indicating best and 3 worst health status). Domains are scored by dividing the sum total of item scores by the total possible score (3 × total number of domain items). This value is then multiplied by 100 to transform it onto a scale of 0 to 100 (0 indicating best and 100 worst health status).
Numerous methods are available to determine the responsiveness of an instrument. As there is no gold-standard approach, it has been recommended that multiple methods are employed [14–15]. Five different statistical analyses were used to evaluate the responsiveness of ePAQ-PF, including: (1) distribution-based methods ((a) effect size, (b) standardized response means, (c) significance of change, (d) responsiveness statistic) and (2) anchor-based methods ((e) minimally important difference (MID)). All statistical analyses were performed using SPSS (version 14).
Effect size
Effect sizes (ES) are one of the most commonly used methods for interpreting change in questionnaire scores [16] and are an estimation of the magnitude of change in health status over time [17]. ES is calculated by measuring the difference between the means pre and posttreatment and dividing this value by the standard deviation of the pretreatment score [18]. Changes in health status are thus translated into a standard unit of measurement aiding interpretation. Accepted ES values are 0.20 (small), 0.50 (moderate), and 0.80+ (large) [19]. A small effect size implies that treatment has little influence on the health status of patients in that specific domain.
Standardized response mean
The standardized response mean (SRM) is similar to ES. However, to calculate the SRM, the mean change in scores (i.e., between baseline and follow-up) is divided by the standard deviation of change in score [20]. This differs from the calculation of the effect size which involves dividing by the SD of the pretreatment score.
Significance of change
The mean changes in domain scores were calculated for women who reported being “better” following surgery on the patient global rating question (see below). Due to the small numbers of women who reported feeling “no better” following surgery (TVT n = 3, prolapse n = 1), significance of change scores were not calculable
Responsiveness statistic
The responsiveness statistic compares subjects who report improvement following intervention on a patient global rating question, with those who report no improvement. It is derived by dividing the mean change in score for patients reporting improvement with the SD of scores from those who report no improvement [21]. A responsiveness statistic value ≥1 indicates that an instrument is highly responsive to change, although a value between 0.20 and 1 indicates an acceptable level of responsiveness [22]. In the present study, a responsiveness statistic could not be calculated for women undergoing prolapse surgery, as only one patient reported “no improvement” in health status.
Minimally important difference
The MID places the magnitude of change in health status in a context that is meaningful for clinicians and patients, i.e., does the observed change in the patient’s health status reflect a trivial or clinically significant impact on quality of life? [23]. MID is an “anchor-based” method as an independent measure or “anchor” is used to interpret the meaning of a degree of change. Although different methods have been postulated for calculating MID, one of the most commonly used methods is based on a patient global rating question [14, 23]. In this study, the global rating question was derived from question 2 of the generic Short Form 36 questionnaire (SF-36) where patients were asked if they felt either (1) much better, (2) somewhat better, (3) about the same, (4) somewhat worse, or (5) much worse following treatment. In the SF-36, this compared health with health 1 year ago. However, in this study, this time frame was modified to take account of the different temporal nature of the study and just asked following treatment. The MID was then estimated by subtracting the amount of change experienced by those patients who reported that they felt “somewhat better” at time 2 and reporting the mean change in each dimension [24].
Results
The mean age of women in the prolapse group was 60.5 years (range 35.1 to 79.2). The mean age of the women in the TVT group was 49.9 years (range 35.8 to 70.3). Responses to the patient global rating question in the ePAQ are summarized in Table 1. Most women felt either “much better” or “somewhat better” following surgery with no patients reporting that they felt “much worse” 3 months after treatment.
TVT: effect size and SRM
Preoperative and postoperative domain scores for the 54 women who underwent TVT are shown in Table 2, with ES and SRM values given for each domain. The highest preoperative mean scores (indicating worst health status) were evident for the stress urinary incontinence (SUI) and urinary quality-of-life (U-QOL) domains. These two domains also showed the greatest change in mean score and the largest ES and SRM values following treatment. The lowest levels of change were seen in the bowel domains (constipation, evacuation, and sex), which also displayed the lowest values for ES and SRM.
Prolapse surgery: effect size and SRM
Preoperative and postoperative mean scores, mean score changes, and ES and SRM values for all 47 women undergoing prolapse surgery are shown in Table 3. As expected, the domains with the highest mean score were prolapse and V-QOL. These domains also had the largest ES and SRM values. The bowel domains for constipation and evacuation showed the lowest levels of change as well as having the lowest ES and SRM values, indicating that prolapse surgery had least effect on health status in these areas.
Significance of change: improved after treatment
The effect size and significance of change scores between time 1 and time 2 were derived for women who had undergone TVT (Table 4) and prolapse surgery (Table 5) who reported themselves to be “much better” or “somewhat better” on the patient global rating question.
A comparison of mean domain scores from baseline to follow-up revealed an improvement in all domains of ePAQ-PF. These changes were statistically significant for all the scales in the questionnaire except four domains in the bowel dimension (irritable bowel syndrome (IBS), constipation, evacuation, and continence). As expected, the largest improvements in health status were found for the scales SUI and U-QOL (as evident from ES statistics). The SRM results were comparable to those found using ES calculations. Although general sex life had the highest SRM value (6.4), the next largest improvements in health status were observed for the SUI and U-QOL.
Similarly, for patients who felt “much better” or “somewhat better” after prolapse surgery, a comparison of mean scores between baseline and follow-up revealed an improvement in all ePAQ-PF domains and these changes (with the exception of bowel domains for constipation and evacuation) were all statistically significant.
Responsiveness statistic
Change scores for the ePAQ-PF for all patients were compared with patient’s own judgement of health status as reported by their answers to the patient global rating question. In the TVT group, change scores for overactive bladder (p < 0.05) and stress urinary incontinence (p < 0.01) were significantly correlated with the responses to the transition question. In the prolapse group, five of the domains were significantly correlated with women’s own view of their health status (as measured by the patient global rating question) including urinary voiding (p < 0.05), bowel quality of life (p < 0.05), vaginal prolapse (p < 0.05), sex vaginal (p < 0.05), and dyspareunia (p < 0.05).
The responsiveness statistic was calculated for the ePAQ-PF domains in women in the TVT group only (Table 6). The responsiveness statistic could not be calculated for the prolapse group, as only one patient reported feeling “about the same” following surgery. Only three women reported feeling “about the same” following TVT surgery. For the capacity, prolapse, and sex bowel domains, there were insufficient data to calculate the mean score change and standard deviation for these patients. Values for the responsiveness statistic ranged from −0.2 for the sex vaginal and dyspareunia domains to 11.3 for the SUI domain.
Minimally important difference
The minimally important differences for patients feeling “somewhat better” after TVT surgery indicated how large a domain score change might be before clinical improvement is seen (Table 6). The results of the minimally important difference calculations indicate that small improvements in subjective health status on the SUI and U-QOL domains in the urinary dimension were equivalent to a 43.6% and 54.7% improvements in scale scores, respectively. As expected, the minimally important differences were smaller for the IBS and sex and bowel domains (TVT surgery does not aim to treat these conditions) and a small improvement in self-reported health status was equivalent to only a 2.8 increase in these scores for both of these domains.
Discussion
This study was carried out in order to determine the responsiveness of ePAQ-PF in the context of corrective surgery for stress urinary incontinence and vaginal prolapse. The results indicate that ePAQ-PF is responsive to change in health status following TVT in the expected and salient domains of stress urinary incontinence and quality of life (in the urinary dimension) and following prolapse surgery in the domains of prolapse and quality of life (in the vaginal dimension). The instrument therefore appears to be suitable for use as an outcome measure in this context.
As expected, for all women who underwent TVT, the SUI domain had the highest mean score at baseline and therefore was the symptom most negatively impacting on HRQOL in this cohort. In relation to those women undergoing prolapse surgery, the prolapse domain had the highest mean score and was the symptom most negatively impacting on health status. In addition, the effect sizes and SRMs were most responsive in these domains (SUI and U-QOL for TVT surgery and prolapse and V-QOL for the prolapse surgery group) thus indicating that the interventions had the greatest influence on health status in these areas. This compares well with previous studies on the effectiveness of TVT [25–26].
Reassuringly, most women felt that treatments for these two common pelvic floor conditions had a positive impact on their health status, with 95% of women who underwent TVT and 96% of women who underwent prolapse surgery reporting themselves as “better” on the patient global rating question. This was supported by the significance of change scores which showed that with the exception of IBS, constipation, and evacuation (in the bowel dimension) a significant improvement in health status between baseline and follow-up was observed. Similarly, in the prolapse group, a significant improvement in health status was seen in all ePAQ-PF domains following prolapse surgery other than for two domains (sex and bowel and bowel evacuation, p > 0.05).
The most significant domain changes following treatment were in the direction clinically expected. The responsiveness statistics were largest for SUI and U-QOL at 11.3 and 2.4, respectively. Thus, patients who reported being “somewhat better” generally had substantial change in these domain scores.
The finding that bowel symptoms were less prevalent in both groups and showed less change following TVT or prolapse surgery group is unsurprising. TVT does not aim to treat bowel symptoms and most procedures for prolapse in this cohort addressed anterior compartment or apical defects rather than posterior compartment defects. Nonetheless, significant improvements were seen in bowel continence and quality of life following prolapse surgery in women who reported improvement in their condition. This may be due to patients undergoing rectocele repair, which is known to improve bowel symptoms [27].
Given the uniformity of structure and the standardized four-point response scale used throughout ePAQ-PF, these results may well prove to be generalizable to other domains of the instrument and other interventions and therefore allow the detection of changes in bowel and sexual function (and the respective quality-of-life domains within these dimensions). Although further work will be needed to confirm this, the bowel dimension of ePAQ-PF is based on the Birmingham Bowel and Urinary Symptoms Questionnaire (Birmingham Bowel and Urinary Symptoms Questionnaire-Q), both of which have demonstrated good responsiveness in a cohort of 630 women undergoing hysterectomy [28].
A limitation of the present study is the small dataset on which it is based. The number of women who reported “no improvement” following both forms of surgery was small. However, it has been suggested that only relatively small datasets are required to examine instrument responsiveness. For example, in a study using the Asthma Quality-of-Life Questionnaire, looking at minimally important difference, complete data were only available for 37 subjects [29]. Similarly, the responsiveness of the Acromegaly Quality-of-Life Questionnaire was based on a sample of only 36 patients [30]. It would also be useful to evaluate the performance of the questionnaire following interventions impacting on other aspects of pelvic floor symptomatology (e.g.. overactive bladder, bowel evacuation, and vaginal capacity) as well as conservative interventions for bowel bladder, vaginal, and sexual disorders, which are generally recommended prior to invasive treatment but where outcomes may be less profound than with surgery.
Conclusions
In the context of pelvic floor disorders, when the primary goals of an intervention are the relief of symptoms, restoration of function, and improving quality of life, a responsive patient-based measure of health is required in order to adequately and meaningfully measure outcome.
Pelvic floor disorders should not be regarded as “all or nothing” phenomena, rather a spectrum ranging from the absence of any symptoms or QOL impairment to devastating symptoms leading to social withdrawal and isolation. Prolapse is a common condition and a degree of vaginal laxity may be regarded as normal in parous women. Certainly, mild and even moderate degrees of the condition do not necessitate treatment. A measure of symptom severity and impact is therefore essential in the context of initial assessment and measuring change.
ePAQ-PF provides 19 scored domains, all of which may be directly relevant to women undergoing treatment for prolapse or incontinence. In its salient urinary, bowel, vaginal, and sexual domains, ePAQ-PF is responsive to change in women undergoing TVT or prolapse surgery and can be recommended as an outcome measure in this context. Other ePAQ-PF domains, such as vaginal capacity, urinary voiding function, and bowel evacuation, may also be highly relevant, both preoperatively and postoperatively for these procedures.
ePAQ-PF may be recommended for use in clinical monitoring, research, service evaluation, and audit, particularly when a patient’s view of her condition and quality of life are considered important. ePAQ-PF is suited to the constraints of clinical practice and the authors recommend its use in outcome research when assessing the effects of interventions for these conditions.
References
Eva UF, Gun W, Preben K (2003) Prevalence of urinary and fecal incontinence and symptoms of genital prolapse in women. Acta Obstet Gynecol Scand 82:280–286
Pauls RN, Silva WA, Rooney CM, Siddighi S, Kleeman SD, Dryfhout V, Karram MM (2007) Sexual function after vaginal surgery for pelvic organ prolapse and urinary incontinence. Am J Obset Gynecol 197(622):e1–e7
Rogers RG, Kammerer-Doak D, Darrow A, Murray K, Qualls C, Olsen A, Barber M (2006) Does sexual function change after surgery for stress urinary incontinence and/or pelvic organ prolapse? A multicenter prospective study. Am J Obstet Gynecol 195:e1–e4
Ghoniem G, Stanford E, Kenton K, Achtari C, Goldberg R, Mascarenhas T, Parekh M, Tamussino K, Tosson S, Lose G, Petri E (2008) Evaluation and outcome measures in the treatment of female urinary stress incontinence: International Urogynecological Association (IUGA) guidelines for research and clinical practice. Int Urogynecol J Pelvic Floor Dysfunct 19:5–33
Radley SC, Jones GL, Tanguy EA, Stevens VG, Nelson C, Mathers NJ (2006) Computer interviewing in urogynaecology: concept, development and psychometric testing of an electronic pelvic floor assessment questionnaire in primary and secondary care. Br J Obstet Gynaecol 113:231–238
Jones GL, Radley SC, Lumb J, Jha S (2008) Electronic pelvic floor symptoms assessment: tests of data quality of ePAQ-PF. Int Urogynecol J Pelvic Floor Dysfunct 19:1337–1347, Epub ahead of print
Bowling A (2005) Measuring health—a review of quality of life measurement scales, 3rd edn. Open University Press, Milton Keynes
Fayers PM, Machin D (2007) Quality of life—the assessment, analysis and interpretation of patient-reported outcomes, 2nd edn. Wiley, Chichester
Guyatt G, Walter S, Norman G (1987) Measuring change over time: assessing the usefulness of evaluative instruments. J Chron Dis 40:171–178
McCracken GR, Henderson NA, Ashe RG (2007) Five year follow-up comparing tension-free vaginal tape and colposuspension. Ulster Med J 76:146–149
Nygaard IE, McCreery R, Burbaker L et al (2004) Abdominal sacral colpopexy in 163 women with posthysterectomy vaginal vault prolapse and enterocele: evolution of operative techniques. J Reprod Med 37:323–327
Ward KL, Hilton P, UK and Ireland TVT Trial Group (2004) A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol 190:324–331
Ward KL, Hilton P, UK and Ireland TVT Trial Group (2008) Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow up. BJOG 115:226–233
Walters SJ, Brazier JE (2003) What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health Qual Life Outcomes 1:4
Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR, Clinical Significance Consensus Meeting Group (2002) Methods to explain the clinical significance of health status measures. Mayo Clin Proc 77:371–383
Lydick E, Epstein RS (1993) Interpretation of quality of life changes. Qual Life Res 2:221–226
Lohr KN, Aaronson NK, Alonso J, Burnam MA, Patrick DL, Perin EB (1996) Evaluating quality of life and health status instruments: development of scientific review criteria. Clin Ther 18:979–992
Kazis L, Anderson J, Meenan R (1989) Effect sizes for interpreting changes in health status. Med Care 27:178–189
Cohen J (1977) Statistical power analysis for the behavioural sciences. Academic, New York
Jenkinson C (1994) Measuring health and medical outcomes. UCL Press, London
Guyatt GH, Eagle DJ, Sackett B (1993) Measuring quality of life in the frail elderly. J Clin Epidemiol 46:1433–1444
Colwell H, Mathias SD, Pasta DJ, Henning JM, Steege JF (1998) A health-related quality of life instrument for symptomatic patients with endometriosis: a validation study. Am J Obset Gynecol 179:47–55
Hajiro T, Nishimura K (2002) Minimal clinically significant difference in health status: the thorny path of health status measures? Eur Respir J 19:390–391
Guyatt GH, Feeny D, Patrick D (1991) Proceedings of the international conference on the measurement of quality of life as an outcome in clinical trials: postscript. Controlled Clin Trials 12:266s–269s
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anaesthesia for treatment of female urinary incontinence. Int Urogynecol J pelvic Floor Dysfunct 7:81–86
Ward K, Hilton P, United Kingdom and Ireland Tension-free Vaginal Tape Trial Group (2002) Prospective multicentre randomised trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ 325(7355):67, 13
Gustilo-Ashby AM, Paraiso MF, Jelovsek JE, Walters MD, Barber MD (2007) Bowel symptoms 1 year after surgery for prolapse: further analysis of a randomised trial of rectocele repair. Am J Obstet Gynecol 197:76.e1–e5
Hiller L, Bradshaw HD, Radley SC, Radley S (2007) Criterion validity of the BBUSQ-22: a questionnaire assessing bowel and urinary tract symptoms in women. Int Urogynecol J Pelvic Floor Dysfunct 18(10):1133–1137, Oct
Juniper EF, Guyatt GH, Willan A, Griffith LE (1994) Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol 47:81–87
Badia X, Webb SM, Prieto L, Lara N (2004) Acromegaly quality of life questionnaire (AcroQoL). Health Qual Life Outcomes 2:13, 27
Acknowledgments
We would like to thank all the women who completed the ePAQ-PF and we are grateful for their support in enabling the instrument to be used as part of their routine clinical care.
Conflicts of interest
G.L.J., J.L., and A.F. have no conflicts of interests to declare. S.C.R. is a director of EPAQ systems Ltd., a recently formed NHS spinout technology company
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jones, G.L., Radley, S.C., Lumb, J. et al. Responsiveness of the electronic Personal Assessment Questionnaire-Pelvic Floor (ePAQ-PF). Int Urogynecol J 20, 557–564 (2009). https://doi.org/10.1007/s00192-008-0790-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-008-0790-9