Abstract
A 67-year-old woman who had failed two prior anti-incontinence surgeries presented with stress urinary incontinence and intrinsic sphincteric deficiency. Calcium hydroxylapatite (Coaptite®) was injected cystoscopically into the bladder neck and proximal urethra and resolved her incontinence. Seven months later, she presented with difficulty in voiding and a urethral mass. Physical examination revealed a large prolapse of the urethral mucosa obstructing the external urethral meatus. Surgical exploration revealed local migration of calcium hydroxylapatite particles from the site of injection (bladder neck and proximal urethra) to the distal urethra. The prolapsed urethral mucosa was incised and marsupialized. Improper injection techniques likely contributed to urethral prolapse in this complication. Meticulous attention to injection techniques is the key to treatment success of urethral bulking agents, particularly in patients who have a scarred/fixed urethra or have multiple urethral/vaginal surgeries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case report
The patient is a 67-year-old postmenopausal woman with a history of hysterectomy, cystocele repair, who has previously failed a trans-obturator midurethral sling (left in situ), and a subsequent bone-anchored xenograph dermis bladder neck sling. She presented with persistent stress urinary incontinence and intrinsic sphincteric deficiency. Physical examination revealed a fixed urethra. Calcium hydroxylapatite (CaHA, Coaptite®, BioForm Medical Inc.) was injected via a rigid cystoscope into her bladder neck and proximal urethra under local anesthesia. A total of 2 cm3 CaHA was used (1 cm3 on the left side, 1 cm3 on the right side). Her stress urinary incontinence was resolved. Seven months later, she presented with progressive difficulty in voiding and a mass in the urethra. Repeat physical examination revealed a large, 2-cm eversion of the urethral mucosa through the external urethral meatus (urethral prolapse). The urethral lumen was compressed by the prolapsed mucosa (Fig. 1). A whitish hue was visualized underneath the mucosa. The prolapsed mucosa itself did not show erosion or abrasion.
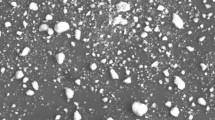
Surgical exploration revealed local migration of the CaHA particles from the injection site to the distal urethra to form a large urethral prolapse. The prolapsed urethral mucosa was incised longitudinally (Fig. 2), and the whitish CaHA beads were explanted. The urethral mucosal edges were then marsupialized to adjacent vaginal mucosa using an interrupted fine absorbable suture (similar to the Spence procedure), at 2-, 4-, 6-, 8-, and 10-o’clock, being careful not to compromise the patency of the meatus. At 1-month follow-up, the prolapse has healed, the meatus was patent without stenosis, and her voiding difficulty has resolved. However, her stress urinary incontinence recurred postoperatively. The patient subsequently had three sessions of repeat CaHA injection and achieved significant improvement of her incontinence without complication.
Discussion
Urethral prolapse is an eversion of the urethral mucosa through the external urethral meatus. The patient in this case had a fixed urethra with intrinsic sphincteric deficiency prior to injection. Seven months later, she presented with a large urethral prolapse. Clearly, the cause of urethral prolapse is iatrogenic. The bulking agent did not stay at its original site of injection (at the bladder neck and proximal urethra) but migrated distally within the 7-month period. This is a case of local migration of injectable material and must be distinguished from distant migration [1, 2] (this is controversial). The large size of the CaHA beads (75 to 125 μm) essentially precluded distant migration.
The true incidence of urethral prolapse formation after bulking agent treatment is unknown. We have performed more than 80 cases of CaHA injections before this complication was encountered. There is only one report each in the literature of urethral prolapse formation after collagen injection [3], carbon-coated beads injection [4], or CaHA injection [5]. We do not believe that this complication is specific for CaHA, since formation of urethral prolapse has been described with other injectable materials. Even though the incidence appears to be rare, this is an important complication to report and to recognize since injection of urethral bulking agents are now commonly used to treat stress urinary incontinence. The development of postoperative voiding symptoms is not uncommon either. A proper pelvic examination should be included as part of the postoperative evaluation if de novo voiding symptoms develop. In this case, the voiding difficulty was due to an obstructing urethral mass (urethral prolapse). This complication may be underreported if the postoperative voiding symptoms are not properly investigated (e.g., with a careful pelvic examination).
Besides stress urinary incontinence, Coaptite® has also been used as a bulking agent to treat vesicoureteral reflux in urology [6–8]. Through a cystoscope and a 21-G needle, CaHA is injected into the bladder submucosa inferior to the refluxing ureteral orifice at the 6-o’clock position. The injectable material positioned submucosally behind the ureter provides the backing necessary to enable its coaptation during bladder filling and contraction. One serious complication of local CaHA migration was reported after 23 injection sessions in 14 children [8, 9]. In that case report, a patient with vesicoureteral reflux was injected with CaHA twice 6 months apart. The bulking agent failed to correct the reflux, so the patient had an open ureteral reimplantation surgery. Three months after the open surgery, CaHA particles (radiopaque) were noted to have migrated proximally along the course of the ureter on a kidney–ureter–bladder radiography image. The patient was subsequently lost to follow-up. She returned 21 months later with severe ureteral obstruction and complete loss of kidney function on the ipsilateral side of the CaHA injection. A computed tomography scan revealed further proximal migration of CaHA to obstruct the midureter at the junction of the iliac vessels [9]. During surgical exploration, the site of the obstructed ureter was surrounded by severely fibrotic tissue/CaHA scars, and it was especially difficult to separate the ureter from the iliac vessels.
Porous granular CaHA has also been used as a bone defect filler material in dental surgery, orthopedic surgery (hip replacement) [10], and orbitocranial reconstructive surgery [11, 12]. The results were excellent with no reported cases of CaHA migration. Collectively, these experiences suggest that the incidence of local CaHA migration is probably low. Nevertheless, submucosal migration of the bulking agent has been reported in isolated cases [3–5, 9].
What factor(s) may predispose patients to form urethral prolapse after bulking agent treatment? Poor injection techniques, such as injecting with excessive force, overdistending the mucosa, or facing the bevel of the needle toward the mucosa rather than away from the mucosa may cause more local tissue trauma and create a wider dissection that separates the submucosa from the underlying periurethral fascia. If the tissue separation is extensive, the beads may dissect along this virtual plane and migrate as a bulk in the early postoperative period before in-growth of host cells around the CaHA beads. This is particularly the case if local factors (e.g., tissue ischemia and significant scarring from previous sling and vaginal surgeries) may have impaired local tissue healing and in-growth of host cells around the injected beads.
Local migration may also occur if the agent is injected at the improper depth. Injecting the agent into the submucosal layer itself helps to keep the agent inside that tissue layer. If the injection is too superficial (into the mucosa), blanching and erosion through the urethral mucosa may occur. If the injection is too deep (beyond the submucosa), migration may occur outside the submucosa. In patients who have an unhealthy urethra (e.g., postmenopausal women with thin urothelial mucosa, postsurgical patients with scarred urethra and obliterated submucosal tissue planes, or postradiation urethra), it can be tricky to define the right depth of injection. This issue is commonly encountered in male patients who presented with postprostatectomy incontinence and a scarred urethra but may also be seen in female patients who had multiple urethral and vaginal surgeries and a scarred/fixed urethra (e.g., in this case).
Having a healthy periurethral tissue enhances the success of bulking agent treatment. With good periurethral support, the agent has a “backboard” to push against and bulk the submucosa centrally to achieve optimal coaptation. The periurethral tissue also provides resistance against longitudinal migration of the bulking agent. Without healthy periurethral “backboard” support, the tendency is to inject too much bulking agent in one session since mucosal coaptation is more difficult to achieve. If the surgeon fails to pay attention to this, the extra trauma to the local tissue and the excess bulk of foreign body may predispose to local migration of the bulking agent.
In summary, meticulous attention to injection techniques is the key to treatment success of urethral bulking agents. This is particularly important in patients who have a scarred/fixed urethra or have multiple urethral/vaginal surgeries. Patients reporting postoperative voiding complaints should have a pelvic examination to rule out obstruction from a urethral prolapse.
Abbreviations
- CaHA:
-
calcium hydroxylapatite (Coaptite®)
References
Pennek J, Brands FH, Senge T (2001) Particle migration after transurethral injection of carbon coated beads for stress urinary incontinence. J Urol 166(4):1350–1353
Ritts RE (2002) Re: particle migration after transurethral injection of carbon coated beads for stress urinary incontinence. J Urol 167(4):1804–1805
Harris RL, Cundiff GW, Coates KW, Addison WA, Bump RC (1998) Urethral prolapse after collagen injection. Am J Obstet Gynecol 187:614–615
Ghoniem GM, Khater U (2006) Urethral prolapse after durasphere injection. Int Urogynecol J Pelvic Floor Dysfunct 17(3):297–298
Palma PC, Riccetto CL, Martins MH, Herrmann V, de Fraga R, Billis A et al (2006) Massive prolapse of the urethral mucosa following periurethral injection of calcium hydroxylapatite for stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 17(6):670–671
Mevorach RA, Hulbert WC, Rabinowitz R et al (2006) Results of a 2-year multicenter trial of endoscopic treatment of vesicoureteral reflux with synthetic calcium hydroxyapatite. J Urol 175(1):288–291
Eryildirim B, Tarhan F, Kuyumcuoglu U et al (2007) Endoscopic subureteral injection treatment with calcium hydroxyapatite in primary vesicoureteral reflux. Int Urol Nephrol 39(2):417–420
Tarcan T, Tinay I, Temiz Y, Simsek F (2007) Long-term results of endoscopic treatment of vesicoueteral reflux with the sub-ureteric injection of calcium hydroxyapatite. Int Urol Nephrol 39(4):1011–1014
Onol FF, Tarcan T, Tinay I et al (2006) Kidney loss due to periureteral fibrosis and ureteral obstruction secondary to migration of subureterically injected calcium hydroxylapatite. J Pediatr Urol 2(5):503–508
Sudo A, Hasegawa M, Fukuda A et al (2007) Acetabular reconstruction using a cementless cup and hydroxyapatite granules. J Arthroplasty 22(6):828–832
Burstein FD, Cohen SR, Hudgins R et al (1997) The use of porous granular hydroxyapatite in secondary orbitocranial reconstruction. Plast Reconstr Surg 199(4):869–874
Tanag MA, Madura T, Yano K et al (2006) Use of calcium phosphate cement paste in orbital volume augmentation. Plast Reconstr Surg 117(4):1186–1193
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lai, H.H., Hurtado, E.A. & Appell, R.A. Large urethral prolapse formation after calcium hydroxylapatite (Coaptite) injection. Int Urogynecol J 19, 1315–1317 (2008). https://doi.org/10.1007/s00192-008-0604-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-008-0604-0