Abstract
The purpose of this study is to evaluate the ability of preoperative urodynamic urethral function parameters to predict the success rate of transobturator slings (TOS). Seventy women urodynamically diagnosed with stress incontinence with urethral hypermobility underwent a Monarc™ TOS (American Medical Systems, Minnetonka, USA). Postoperative continence status was correlated with preoperative urodynamic urethral function parameters. Mathematical modeling was used to determine whether urodynamic parameters can be used to predict postoperative continence. Average follow-up was 8.1 (6–12) months; 56 (80%) patients were continent based on a standardized stress test and subjective report. The median Valsalva leak point pressure at 150 cc (VLPP150) in the failures and successes was not different (p = 0.12). The median VLPP at cystometric capacity (VLPPcap) in the failures was 32 cmH2O compared to 71 cmH2O in the successes (p < 0.001). The maximum urethral closure pressure (MUCP) had a median of 20 cmH2O in the failures and 45 cmH2O in the successful patients (p < 0.001). No correlation existed between the degree of urethral hypermobility, as measured by the cotton swab test, and surgical success (p = 0.17). There was no correlation between level of preoperative urethral function and persistent overactive bladder symptoms, post-void residual, voids/day, and nocturia. Using a combined model, the cutoff values of VLPPcap > 60 cmH2O and MUCP > 40 cmH2O were the most predictive of surgical success, revealing a sensitivity of 83% (0.55, 0.95) and specificity of 79% (0.67, 0.88). A combination of urodynamic parameters can be used to predict continence rates after a TOS. A TOS should be used with caution in women with impaired urethral function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The most recent decade has seen a revolution in the surgical treatment of stress incontinence (SI) with the introduction of minimally invasive sub-urethral sling techniques. The tension-free vaginal tape procedure (TVT), first described by Ulmsten in 1995 (TVT, Gynecare, Ethicon, New Brunswick, NJ, USA), is the most widely used and studied of these techniques [1]. A 5-year follow-up demonstrated an objective and subjective cure rate of 84.7%; 10.6% were significantly improved, and 4.7% were considered failures [2]. However, the retropubic, blind upward vaginal passage of the metal needles has generated concerns regarding the safety profile of this procedure [3]. Major vascular and nerve injuries, bladder perforations, as well as bowel perforations with associated deaths have been reported [4–9]. Voiding dysfunction after TVT is also not uncommon with postoperative de novo urinary urgency reported in 5–15% of patients and transient urinary retention occurring in up to 17% of patients [10].
Alternative minimally invasive surgical approaches for SI have been developed in an attempt to avoid the complications associated with TVT. A new approach using a transobturator needle passage for tape placement has been described [11]. To date, very few bladder injuries and no visceral or major vascular injuries have been reported [12]. Moreover, the increased safety may not have compromised efficacy, with recent studies reporting short-term cure rates greater than 90% [11, 13]. Transient voiding dysfunction after the transobturator sub-urethral tape procedure appears to be lower, with de Tayrac et al. [13] reporting a 13.3% rate of transient urinary retention for TOS compared to 25.8% for TVT in a recent prospective, randomized trial.
The lower rate of reported voiding dysfunction is likely due to the more obtuse sub-urethral angle created by the TOS tape. Unlike the narrow support angle provided by retropubic slings such as TVT, the TOS forms a flat platform of support, thus being less likely to obstruct the urethra. This may be preferable for the treatment of a woman who has uncomplicated SI with an intact urethral sphincter. However, in a patient with a compromised urethral sphincter as well as a lack of urethral support, a certain degree of obstruction may be required.
The concept of utilizing urodynamic parameters of urethral sphincteric function to predict anti-incontinence surgery outcomes is not new [14]. Tests of both passive urethral function [maximal urethral closure pressure (MUCP)] and dynamic sphincter function [Valsalva leak point pressure (VLPP)] are routinely performed during urodynamic assessment. Cutoff values for either test are not universally agreed upon. Nevertheless, an assessment of urethral sphincteric function is routinely achieved during urodynamics and has been used for surgical procedure selection.
The aim of this study was to evaluate the efficacy of the Monarc™ TOS for the treatment of SI according to the level of urethral function based on preoperative urodynamic testing [urodynamic study (UDS)].
Materials and methods
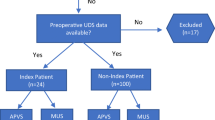
The initial 70 consecutive women who underwent treatment for SI with urethral hypermobility by a Monarc™ transobturator Subfascial Hammock (American Medical Systems, Minnetonka, MN, USA) were studied in a retrospective fashion. All surgeries were performed by a single surgeon (GWD). Due to the short learning curve for performance of a TOS, it was not deemed necessary to exclude the initial cases. Institutional review board approval was obtained, and the Urogynecology database was queried for the desired variables. All subjects had a thorough preoperative evaluation including a history, physical exam, UDS, standardized standing cough stress testing with 150–300 cc bladder volume, 3-day voiding diary, and if indicated, cystoscopy.
UDS measures included post-void residual (PVR), multichannel cystometrogram, VLPP testing at 150 cc (VLPP150) and at maximum cystometric bladder capacity (VLPPcap), MUCP at bladder capacity, uroflowmetry or pressure voiding studies, and determination of urethral mobility via a cotton swab test. Prolapse to, or beyond the introitus, was reduced with a speculum for testing. Air-charged catheters were used for urodynamic testing, and VLPP values were recorded as abdominal pressure at urine loss during strong Valsalva efforts, with the urethral catheter removed. Observation of urine/fluid loss at the external urethral meatus was used to record the VLPP value.
For study inclusion, SI was defined in a patient who demonstrated objective leakage with an increase in abdominal pressure during urodynamic testing. Women with a “Q-tip” angle of ≤30 degrees as well as urodynamically demonstrated detrusor overactivity were excluded from this review.
The Monarc™ transobturator sling (TOS) was performed in a standard fashion, and concomitant procedures were performed as indicated. Placement of the tape was performed using a Kelly clamp held between the urethra and the tape in a vertical position, while the plastic envelope surrounding the tape was removed. Cough testing was not performed. Cystoscopy was performed in all cases.
Follow-up visits were scheduled at 2 weeks, 6 weeks, 3 months, 6 months, and yearly. Data was analyzed once 70 sequential patients had reached at least the 6-month follow-up visit.
Outcomes were recorded at the last follow-up visit using standardized questionnaire and physical exam. Measures included subjective complaints of SI symptoms, pad usage, overactive bladder (OAB) symptoms, voids/day, episodes of nocturia, cough stress test results, and PVR. Success was defined as subjective reporting of absence of stress continence and a negative standing cough stress test with at least 150 cc of urine in the bladder, performed in the office.
To assess differences between subjects with persistent SI symptoms and asymptomatic patients postoperatively, VLPP150, VLPPcap, and MUCP values were compared using the Wilcoxon rank sum test. A two-sided, two-sample t test was used to compare the degree of urethral mobility and surgical outcomes. All tests were conducted at the 5% significance level.
Using independently significant factors (VLPPcap and MUCP), a surgical outcome model was created to identify what degree of urethral function was associated with increased TOS sling failures. Failure was defined as persistent SI symptoms and/or a positive cough stress test at the last postoperative visit. The sensitivity, defined as the probability that a person with a failed surgery would be identified by a specific cutoff value of VLPPcap and MUCP, and specificity, defined as the probability that a successful surgery would be identified by a specific cutoff value of VLPPcap and MUCP levels, were calculated separately. The VLPPcap and MUCP results were then paired in all possible combinations. The most relevant results were superimposed on a graph of surgical outcomes. Confidence intervals (95%) for the sensitivity and specificity were calculated for all combinations of VLPPcap and MUCP levels.
Results
The 70 SI patients had an average age of 60.9 (range, 30–92) years and a mean parity of 2.3 (0–9). The average last follow-up visit was 8.1 months (6–12). These patients used a mean of 3.8 (0–10) pads/day, voided 6.1 (3–11) times/day, and had an average of 1.8 (0–6) episodes of nocturia/day. Preoperatively, 31 (44.3%) patients complained of mixed incontinence symptoms, 15 (21.4%) complained of SI symptoms alone, and 10 (14.3%) complained of OAB symptoms. Fourteen (20%) subjects had “occult” SI, with no incontinence symptoms being reported with the prolapse unreduced. All had urodynamically confirmed SI without detrusor overactivity. Concomitant procedures performed included cystocele repair (29), vault suspension (33), enterocele repair (32), rectocele repair (45), hysterectomy (18), salpingo-oophorectomy (7), and Lefort colpocleisis (9).
There were no operative complications, including bladder or urethral perforations, mesh erosions, infections, or other healing complications. Additionally, no patients had significant voiding dysfunction after surgery, including abnormal urinary stream, elevated PVR, urinary frequency, or urgency symptoms. In addition, no subjects reported postoperative OAB symptoms. In this series, preoperative PVR averaged 66.1 ml, and postoperative PVR averaged 30.5 ml (p = 0.37).
Fifty-six (80%) women reported complete stress continence and had a negative cough stress test. Postoperative urodynamics were not performed. Thus, the classification of surgical failure was based on subjective reporting and a standardized stress test. No difference in outcome was noted when the initial few patients operated on were compared to later patients, confirming the short learning curve for this technique. Overall, 80% of subjects enrolled were considered cured of SI.
The median VLPP150, VLPPcap, and MUCP of successes and failures were calculated (Table 1). The median VLPP150 in the failures was 131 cmH2O, compared to no leakage with a Valsalva maneuver with 150 cc in the bladder in the successful procedures (p = 0.12). The median VLPPcap in the failures was 32 cmH2O compared to 71 cmH2O in the successes (p < 0.001), and the MUCP had a median of 20 cmH2O in the failures and a median of 45 cmH2O in the successful patients (p < 0.001).
In more simplistic terms, using traditional urodynamic cutoff values, the failure rate with MUCP ≤ 20 cmH2O was 54.5% compared to 13.6% with a MUCP > 20 cmH2O (p = 0.006). With a VLPP150 ≤ 60 cmH2O, the failure rate was 35.7% compared to 16.1% above 60 cmH2O (p = 0.11), and at VLPPcap ≤ 60 cmH2O, the failure rate was 38.7% compared to 5.1% above (p < 0.001). None of the occult incontinence subjects developed postoperative SI symptoms. Further, patients with preoperative mixed incontinence findings did not appear to be at higher risk for persistent SI symptoms, with persistent symptoms in 14.3% of the mixed subjects and 17.5% of SI only subjects.
The mean cotton swab angle in the successful surgeries was 73.1°, and the mean in the failures was 65.6°. The relationship between cotton swab angle and persistent incontinence was not significant (p = 0.17, Fig. 1). This relationship held true using both mean and median values for analysis. Additionally, the effectiveness of the sling did not appear different when the TOS was performed alone or with concomitant procedures with a failure rate of 25% performed alone and 16.1% performed in conjunction with other procedures.
Using persistent SI, based on our definition of cure, as the measure of surgical failure, a predictive surgical outcome model was created. VLPP150 and cotton swab angles were dropped from the analysis as they were not predictive.
To more specifically identify at what level of urethral function most failures occurred, the failure rate at different levels of the urethral assessment variables (VLPPcap and MUCP) were separately calculated at 20 cmH2O increments (Table 2). Within the range of concern, the sensitivity and specificity of VLPPcap and MUCP were then calculated in 10 and 5 cmH2O increments, respectively. These results were paired in all possible combinations, and the joint sensitivity and specificity were calculated (Table 3).
The cutoff values of VLPPcap ≤ 60 cmH2O and MUCP ≤ 40 cmH2O were the most predictive, revealing a sensitivity of 83% (0.55, 0.95) and specificity of 79% (0.67, 0.88). The failure rate of a TOS for patients below these levels was 45.5% and above was 4.2%. The more commonly used cutoff points of VLPPcap ≤ 60 cmH20 and MUCP ≤ 20 cmH2O were also analyzed for comparison. These points gave a sensitivity of 50% (0.25, 0.75) and a specificity of 95% (0.86, 0.98). The failure rate was 66.7% below the traditional cutoff and 9.8% above.
A graphical plot of surgical outcomes with associated VLPPcap and MUCP levels was created, and the above relevant cutoff points were superimposed (Fig. 2). All but two failures fell within the intersection of the VLPPcap = 60 cmH2O and MUCP = 40 cmH2O, with both of those falling below MUCP = 40 cmH2O. Thus, the success rate of TOS above these cutoff values is 95.8%.
Discussion
The TOS was developed in an attempt to improve the safety profile of minimally invasive sub-urethral slings for the treatment of female stress urinary incontinence. Once healing is completed, the TOS tape extends horizontally between the pubic rami, forming a platform of mid-urethral support, which may be less occlusive than retropubic slings and have less of an impact on voiding function [14]. This fact may, however, affect surgical success rates. No patients in this study had significant voiding dysfunction after the procedure, and no subject required prolonged catheterization. Postoperatively, there were no differences in PVR based on degree of urethral function, nor was there a significant difference from preoperative values. Likewise, median voids/day or episodes of nocturia were not different from preoperative values.
Noting high incontinence rates in women with poor preoperative urethral function, we attempted to better predict failure by developing a surgical outcome model. The three common urodynamic tests used to assess urethral function are the cotton swab test (“Q-tip” test), MUCP, and VLPP. The cotton swab test and VLPP with 150 cc in the bladder were not predictive of surgical outcomes and were dropped from further analysis. The data were analyzed to determine if a given combination of VLPPcap and MUCP values could preoperatively predict TOS success or failure. Traditional cutoff points of VLPPcap ≤ 60 cmH20 and MUCP ≤ 20 cmH2O correctly identified 6 of the 12 failures. A VLPPcap ≤ 60 cmH2O and MUCP ≤ 40 cmH2O was a better model with 10 of the 12 failures in this series falling below the intersection of these cutoffs. This translated into a failure rate of 45.5% below and 4.2% above a VLPPcap of 60 cmH2O and a MUCP of 40 cmH2O.
Correction of SI via a TOS approach does not appear to be dependent on the degree of urethral hypermobility, as long hypermobility is present, as we did not test it in women without urethral hypermobility. In this series, Q-tip angle values did not correlate with success or failure, as urodynamic parameters did.
The TOS tape’s final position as that of a horizontal platform of urethral support is in contrast to the more occlusive “U”-shaped support provided by retropubic slings. In the population of patients with poor urethral sphincter function, this lack of urethral occlusion may be detrimental. Short-term follow-up of this cohort of patients supports this hypothesis, as success rates were high for patients with a normally functioning urethra (95.8%) based on static and dynamic parameters and were low (54.5%) for women with a certain degree of urethral compromise.
Patients with significant urethral sphincter impairment are recognized as a challenging population to treat using any technique, but a retropubic sling that can be tensioned may be a preferable surgical approach. TVT® has reported cure rates of 74% and significant improvement of 12% at 4 years for intrinsic sphincter deficiency (ISD) [15]. With a follow-up of 3.5 years, Prolene patch sub-urethral slings have reported success or substantial improvement rates of 80% for patients with ISD [16]. Other traditional sling procedures also have reported cure rates for ISD of 73 to 100% [17]. While the reported cure rates of these procedures are lower for ISD than for stress urinary incontinence with intact urethral sphincter function, they are markedly better than the 54.5% success rate we are reporting for a TOS with a VLPPcap ≤ 60 cmH20 and a MUCP ≤ 40 cmH20.
There are a number of limitations to this study. VLPP assessments in our urodynamics laboratory are routinely performed at 150 cc and bladder capacity. We are cognizant that there is a wide array of VLPP testing techniques, as there is no accepted standard. A significant correlation between surgical outcomes and VLPP150 was not noted. This specific finding and a determination of the most appropriate bladder volume to perform a VLPP, in general, require further investigation. This series was retrospective, patients had different follow-up intervals, and the TOS results were not directly compared to other surgical procedures in a randomized manner. The follow-up period was relatively short with an average of 8.1 months. In addition, outcomes were assessed clinically, and no urodynamic testing was performed postoperatively. The number of patients (70) was also limited. However, the follow-up period and number of patients was adequate to establish statistical significance.
A prospective randomized trial comparing TOS to other anti-incontinence procedures such as a retropubic sling would be necessary to confirm our observations.
Conclusions
Urodynamic assessment of urethral sphincter function may be helpful in identifying patients at a higher risk of surgical failure. Based on our data, we have stopped using a TOS in women with a MUCP ≤ 40 cmH2O and VLPPcap ≤ 60 cmH2O.
References
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J 7:81–86
Nilsson CG, Kuuva N, Falconer C et al (2001) Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J (Suppl 2):S5–S8
Pelosi MA II, Pelosi MA III (2003) New transobturator sling reduces risk of injury. OBG Manage 15(7):17–38
Peyrat L, Boutin JM, Bruyere F et al (2001) Intestinal perforation is a complication of TVT procedure for UI. Eur Urol 39:603–605
Walters MD, Tulikangas PR, LaSala C et al (2001) Vascular injury during tension-free vaginal tape procedure for stress urinary incontinence. Obstet Gynecol 98:957–959
Zilbert AW, Farrell SA (2001) External iliac artery laceration during tension-free vaginal tape procedure. Int Urogynecol J 12:141–143
Vierhout ME (2000) Severe hemorrhage complicating TVT: a case report. Int Urogynecol J 12:139–140
Brink DM (2000) Bowel injury following insertion of TVT. S Afr Med J 90:450–452
Shobeiri SA, Garely AD, Chesson RR (2002) Recognition of occult bladder injury during the tension-free vaginal tape procedure. Obstet Gynecol 99:1067–1072
Wang KH, Neimark M, Davila GW (2002) Voiding dysfunction following TVT procedure. Int Urogynecol J 13(6):353–357
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of urinary stress incontinence in women. Prog Urol 11(6):1306–1313
Boyles SH, Edwards R, Gregory W, Clark A (2007) Complications associated with trans-obturator sling procedures. Int Urogynecol J 18(1):19–22
de Tayrac R, Deffieux X, Droupy S, Chauveaud-Lambling A, Calvanese-Benamour L, Fernandez H (2004) A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol 190(3):602–608, (retracted)
Sand PK, Bowen LW, Panganiban R, Ostergard DR (1987) The low pressure urethra as a factor in failed retropubic urethropexy. Obstet Gynecol 69(3):399–402
Rezapour M, Falconer C, Ulmsten U (2001) Tension-free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD)—a long-term follow-up. Int Urogynecol J 12(Suppl):S12–S14
Raders JL, Aguirre O, Davila GW (2004) Polypropylene patch sling for the treatment of intrinsic sphincter deficiency. J Pelvic Med Surg 10(Suppl):S63
Haab F, Trockman BA, Zimmern PE, Leach GE (1997) Results of pubovaginal sling for the treatment of intrinsic sphincter deficiency determined by questionnaire analysis. J Urol 158:1738–1741
Author information
Authors and Affiliations
Corresponding author
Additional information
G. Willy Davila is a consultant to American Medical Systems.
Rights and permissions
About this article
Cite this article
Guerette, N.L., Bena, J.F. & Davila, G.W. Transobturator slings for stress incontinence: using urodynamic parameters to predict outcomes. Int Urogynecol J 19, 97–102 (2008). https://doi.org/10.1007/s00192-007-0393-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-007-0393-x