Abstract
This randomised control trial compares full-length autologous slings (Group A: 81 women) with a modified “sling-on-a-string” (Group B: 84 women) technique for the treatment of stress urinary incontinence (SUI). Primary outcomes are quality of life (QoL) scores; Group A/Group B. The IIQ-7 scores decrease from 1.91/1.85 at baseline to 0.65/0.72 at 12 months and 0.85/0.92 at +5 years. The UDI-6 scores decrease from 1.85/1.61 at baseline to 0.66/0.62 at 12 months and 1.22/1.08 at +5 years. The incidence of SUI is 13% at 3 months but averages 53% at +5 years. Both techniques offer similar improvements. The shorter sling is quicker, less painful and with less hospital readmissions. The ‘sling-on-a-string’ technique is as effective as the standard technique with better short-term sequelae. The incidence of SUI post-autologous slings rises over the long term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are many different surgical procedures that can be employed when treating women with stress urinary incontinence (SUI.). The surgeon is somewhat overwhelmed with choice [1]. Thinking has matured over the years, so that we no longer talk of repositioning the urethra but of providing support or occlusion and being able to achieve these ends using a variety of surgical approaches and materials [2].
Sub-urethral autologous slings have been used since the early 1900s with Aldridge [3] describing the first abdomino–vaginal sling in 1942. Concerns about surgical morbidity, operative time and cosmetic results of slings [4] led to the development of newer sling techniques. The use of fascia enjoyed something of a revival in the 1990s [5–7], but the subsequent advent of mid-urethral tapes driven by the development of TVT™ (Gynecare) has led to a revolution in surgery, such that traditional operations such as the Burch colposuspension and fascial slings are now rarely performed in the UK [8].
A prospective randomised control trial (RCT) was set up in the early 1990s to compare conventional full-length pubovaginal sling technique with a modified “sling-on-a-string” technique. In this paper, we present short-term data as well as medium- and long-term quality of life (QoL) data on the outcomes.
Materials and methods
Population
Women aged 18 years and older with clinically and urodynamically proven SUI who needed corrective surgery were invited to participate. Exclusion criteria included women who refused or were unable to give consent, women with evidence of neurological disease and women with urodynamic evidence of detrusor overactivity (DO) or hypocompliance (assessed urodynamically as a pressure rise of more than 20 cm of H20 at a capacity of 500 ml using a filling speed of 50 ml/min).
Centres
Patients were recruited from three hospitals in South Wales, (UK) over a period of 24 months. The study commenced after review and approval from the appropriate local research ethics committees.
Randomisation
Patients were divided into two groups by an independent randomisation schedule. A computer-generated randomisation schedule was used for each centre and each individual. Remote telephone randomisation by the independent research team was undertaken after obtaining written informed consent.
The study was not blinded because the type of operation performed was obvious to all medical and nursing personnel involved in the assessment.
An independent evaluator was appointed by the funding body to review clinical outcomes at 6 and 12 months into recruitment to ensure that there were no major differences between the two groups.
Procedure
Pre-operative assessment
Patient’s demographic details were recorded. All patients had a vaginal examination to assess for bladder neck mobility, prolapse and obvious incontinence. Patients filled in frequency volume charts (FVC) and underwent videourodynamics (VCMG) and a one-hour pad test. The impact of their incontinence on their QoL was assessed using the Urogenital Distress Inventory (UDI) and the Incontinence Impact Questionnaire (IIQ) [9].
Operative intervention
The investigators at each centre agreed to an operation standard for the two procedures.
Group A: standard pubovaginal sling
A 20 × 1.5 cm strip of fascia was fashioned from a transverse strip of rectus sheath taken through a transverse suprapubic incision. The resultant defect was then closed. After opening of the retropubic space through two laterally placed vaginal incisions, the sling was passed through a tunnel at the level of the bladder neck and sutured with absolutely no tension to the rectus fascia on each side. The abdominal skin incision was then closed.
Group B: “sling-on-a-string”
The technique for this study was similar to that of Group A, except that the length of the sling obtained was between 8–10 cm, thus requiring a smaller skin incision and less fascial dissection. The sling was mounted at each end with no. 1 nylon threads and passed through the retropubic space, as with the standard sling. The nylon threads were then tied over the rectus fascia aponeurosis, again with no tension. The sling being suspended from the rectus fascia like a hammock.
Other procedures, e.g. prolapse repair, perineal repair, abdominoplasty and hysterectomy were permitted and were fully documented. Antibiotic prophylaxis, analgesia and thromboprophylaxis were standardised within each unit.
A post-operative record detailing complications, voiding details and duration of hospital stay was kept for all patients.
Pain scores were recorded on a 4-point scale at 24 h after surgery, days 4/5 and 3 months post-op. Patients were asked about any type of pain as well as specifically about wound and angle pain.
Short-term assessments
Patients were seen at 3, 6 and 12 months. Patients filled in FVC and underwent pad testing. The UDI and IIQ questionnaires were completed. Patients were also asked about adverse events and hospital readmissions. On their questionnaire, there was also a question stating ‘Are you satisfied with your operation? Yes or No.’
Pain scores were again assessed at 3 months.
Medium- and long-term follow-up
Patients were assessed using postal questionnaires. Medium-term follow-up ranged from 25–60 months (average 42 months/3.5 years). Long-term follow-up ranged between 61–89 months (average 74 months/6.2 years).
Quality of life was assessed using UDI-6 and IIQ-7 [10], which had become available since the study commenced, to simplify assessment.
Patients were also asked if they had to perform intermittent self-catheterisation (ISC) or whether they had needed further surgery because of their urinary incontinence.
Outcome measures
Primary
The primary objective was to compare the QoL scores in both groups over time. The aim was to analyse both the overall scores as well as to look for any differences in scoring on the specific questions relating to stress leakage and urgency.
The success rate of our interventions was measured by calculating the recurrence of stress leakage symptoms as reported on the UDI-6.
Secondary
Secondary outcome measures included operative time and complications, pain scores, length of stay and readmission rates, patient satisfaction, pad test results, voiding difficulties as well as the rate of further operative procedures over time.
Statistical analysis
Sample size calculations were performed in 1990s when the study was initiated and were based on available evidence at the time [11, 12]. It was assumed that the standard operation would be 95% successful in alleviating stress incontinence. To detect a clinically significant difference of 15% between the two procedures, a sample size of 164 patients was required (at the 95% significance level with 80% power).
Statistical analysis is based on the intention to operate. The analysis was performed using SPSS and compromises standard procedures including chi-squared tests for comparing categorical data and unpaired t-tests for measurement data.
Results
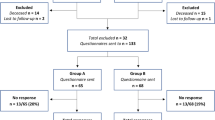
One hundred sixty-eight women were recruited (Fig. 1): 41 at Morriston Hospital (Swansea), 72 at Singleton Hospital (Swansea) and 55 at University Hospital of Wales (Cardiff) over a 2-year period. Three patients did not have urodynamic stress incontinence (USI) on videourodynamic assessment and were, therefore, excluded pre-randomisation. We report on the remaining 165 patients (Fig. 1).
The two groups were matched in demographic details and baseline symptomatology (Table 1). There were no significant differences in the incidence of bladder neck mobility, urogenital prolapse or vaginal scarring between the two groups. Forty-six patients had previously undergone one or more forms of incontinence surgery. Again, these were approximately equally distributed between the two groups (Table 1). Some patients underwent concomitant procedures; these were again similar between both groups.
Primary outcomes
The UDI-6 and IIQ-7 scores were extracted from the long forms [10] to allow comparison over the entire follow-up period. Table 2 shows the significant improvement found in the average scores for both the UDI-6, p = 0.007, and the IIQ-7, p = 0.002 (analysed using repeated measures linear models). The trend over time comprises an initial fall that starts to rise over time. At medium- and long-term follow-up, the trend appears to be a return to baseline, which is more marked in the UDI. The scores, however, are still well below baseline levels and remain statistically significantly different to baseline levels. When both groups are compared, over all the follow-up points, there are similar improvements in scores for the two groups over time (p = 0.414 for group factor for IIQ, p = 0.057 for UDI for the entire profile).
Table 2 highlights the scores obtained for the UDI-6 questions assessing the symptoms of stress leakage and urgency. There is again a significant initial improvement (p < 0.001 for both questions). This improvement again also persists over time to medium- and long-term follow-ups. The trend, however, is a slow rise in scores. There is again no significant difference between groups for the scores obtained for the symptom of stress leakage (p = 0.882) or urgency (p = 0.073) at any of the follow-up points.
The incidence of stress incontinence at our assessment points was calculated using the symptom specific question on the UDI-6. Patients scored the severity of their symptoms on a 4-point scale where 0 score means ‘not at all’. We, therefore, assessed the incidence of stress leakage at our follow-up points by excluding women who scored 0. All other women, even if they only stated that they were ‘slightly’ bothered, were grouped together. This allowed us to calculate the percentage of women suffering any SUI.
To address the issues of non-responders, we analysed the data using three definitions.
-
1.
Intention to treat (ITT): All non-responders were assumed to be treatment failures.
-
2.
Per protocol (PP): Failures were calculated from the patients who actually responded/available data.
-
3.
Best possible (BP): All non-responders were assumed to be cured.
Table 3 shows the incidence of stress leakage at all assessment points. As expected, the baseline incidence is 100% in both groups. This decreases to between 10–21% at 3 months. The incidence of stress leakage continues to gradually rise, so that by long-term follow-up, the incidence of stress leakage is at best 38% (Group A) and 43% (Group B) but could be up to 71% (Group A) and 56% (Group B). Whilst levels do not reach baseline, there appears to be a more worrying trend towards baseline than when looking at the mean scores.
There are no significant differences in the incidence of stress leakage between the two sling techniques at any of the short-term assessment points or at medium-term follow-up; however, non-responders are analysed. At long-term follow-up however, in the ITT arm, Group A—standard slings appear to have a significantly higher failure rate. This may be simply due to the fact that we had more non-responders in Group A than in Group B rather than any clinically significant result.
The pre-operative incidence of urgency symptoms was 86%, based on women scoring >0 for the UDI-6 question on urgency (Table 4). This had decreased to 33% by the 3-month follow-up and was still only 40% by 12 months. By long-term follow-up however, the incidence is nearing baseline levels. Six patients in Group A (7%) and two in Group B (2%) developed de novo urge incontinence.
Secondary outcomes
The operative time was significantly shorter (p = 0.001) for Group B, ‘sling-on-a-string’ (Table 5). The average blood loss in Group B was less than in Group A, although this did not quite reach statistical significance. Two patients were transfused in each group. There were no significant differences in perioperative complications or in mean post-operative length of stay between the two groups (Group A: 6.48 days vs Group B 6.73 days). There were significantly less readmissions related to surgery in Group B in the first 3 months post-operatively.
There was no significant difference in pain scores, or the site of pain, between the two groups at 24 h (Table 6). At days 4–5, women in Group B appear to have an increased incidence of pain, although this does not quite reach statistical significance. In the immediate post-operative period, 75 patients in Group A and 72 patients in Group B used a patient controlled intravenous analgesia technique. In Group A, 11 patients also received intramuscular opiates compared with 17 in Group B. Oral analgesia was recorded for 80 patients in Group A and 83 patients in Group B and was comparable. At 3 months, women in Group B (sling-on-a-string) had significantly less pain, in particular pain at the lateral angles of sling dissection, than the women in Group A.
ISC was taught to 21 patients in Group A and 13 patients in Group B, whilst still in-patients. At the time of discharge, 59 Group A patients and 69 Group B patients were voiding normally. This difference was not statistically significant. There was no significant difference in the incidence of voiding difficulties at 12 months (Table 5). One woman in Group A and four in Group B required the sling to be surgically released. At long-term follow-up, three women from each group performed ISC. One woman in Group B had permanent suprapubic catheter after an augmentation cystoplasty. Similar number of patients in both groups had had further continence procedures performed (Table 5).
Early pad test results are significantly improved compared to baseline, but again, there is no difference between the two groups. No significant differences were observed in the number of patients who were satisfied with the outcome of surgery at 12 months (Table 7).
Discussion
Since this study was initiated, there has been a great deal more interest in sling procedures, which have now been widely adopted as a primary surgical option for treatment of SUI [8, 13]. There are plenty of short-term data on the efficacy of biological slings to support their use [14], but the data are often limited with much of it based on case series or non-RCTs [14, 15]. Long-term data remain scarce [15]. In this paper, we present one of the largest RCTs to date comparing two sling techniques over a long period of follow-up.
The original statistical modelling for this trial was performed in 1994 and was based on an expectation of surgery being 95% successful [11, 12]. This was perhaps a little over ambitious, although papers are still presented quoting success rates of over 90% [16–19]. Our paper suggests success rates of around 87% in the short term. The results in our study being underpowered to answer the primary question, i.e. if there are any differences in outcome between the two sling techniques. Furthermore, over the long-term follow-up period, we lost 23 women (14%) to follow-up. Whilst we believe this is still quite a good response rate for a trial that has now run more than 8 years, it results in the study being underpowered even at the statistical calculations of 1994. Nonetheless, it still remains a large series with a minimum of a 5-year follow-up, and we believe the data presented are still important for clinical practice.
Our data have shown that autologous sling techniques result in significant improvement in QoL scores over long-term follow-up. Although results have reflected a return in incidence of SUI over time, the QoL scores are still much improved from baseline, even after 5 years. When we look at the score obtained for the symptom of stress incontinence, whilst the majority of women pre-operatively were scoring 2–3 (‘moderately’–‘greatly’), at long-term follow-up, the majority were scoring 1 (‘slightly’), i.e. the mean score at long-term follow-up being less than half of the baseline score for the IIQ and symptom of stress leakage. Previous authors who obtained QoL follow-up data also found significant improvement after interventions at follow-up but over a shorter follow-up period: Maher et al. [20]—6 months, Corcos et al. [21]—1 year and Clyne et al. [16] and McBride et al. [19]—2 years. Morgan et al. [22] presented QoL data of a case series of autologous slings with a mean follow-up of 52 months. There was no pre-operative data to compare with however.
The subjective results for this series, however, are not as good as some previously reported [11, 23]. Clyne et al. [16] had a 95% completely dry rate at 6 months. Their sling technique was essentially the same as our long sling, where we achieved a complete continence rate of 82%. Whilst we accept that our results may be the result of less effective surgery, the reason for our poorer results may be our more rigid definition of cure.
There is great difficulty comparing outcomes between papers, as measures of success are not standardised. ‘Cure’ does not necessarily mean ‘dry’ or never incontinent, sometimes it simply reflects improvement [5, 15, 24]. Kobashi and Govier [7] reported a success rate of 85.7% at a mean follow-up of 20.9 months. However, when you look at the completely dry rate this is actually 45%. Bai et al. [18] published an RCT, where at 12 months, pubovaginal sling achieved a continence rate of 93%, whereas tension-free vaginal tape (TVT) and Burch Colposuspension only achieved 87% cure rates. This trial only included 29 autologous slings, and the definition of ‘cure’ included ‘an absence of subjective complaints of leakage’, which is not as rigid as our definition.
This problem is even more pertinent when you look at studies giving long-term follow-up. Morgan et al. [22] reported an 85% cure rate on women followed-up for 5 years. This did, however, include patients who had undergone secondary sling procedures to achieve continence. Maher et al. [20] also followed-up patients for 5 years. They, however, only reported on 13 slings at this stage, and a 69% continence rate and patient satisfaction is quoted.
Despite our women having no evidence of DO on VCMG, the symptom of urgency was common in women both pre- and post-operatively. Our QoL data demonstrate a post-operative improvement in mean score obtained for the symptom of urgency in our patients. This improvement appears to persist over time so that by long-term follow-up, although scores are slowly increasing, they again have not returned to baseline. Most of the published literature on this symptom relates to the de novo rate of urgency [1, 20] rather than any improvement in pre-existing symptoms. Our de novo urgency rate was 4.8%, which is comparable to that found in the literature [1, 14]. Barrington et al. [11] described a 78% improvement in pre-existing urgency symptoms post-autologous sling. Fulford et al. [12] found a 69% improvement, whilst Morgan et al. [22] found pre-operative urge incontinence resolved in 74% of women. We found that 53% of our women were cured of urgency symptoms post-operatively. Our follow-up data extend for significantly longer period of time, and the improvement is maintained. The mechanism of this improvement is unclear. It has been argued that providing bladder neck stability [12] results in less DO, but it may simply be an improvement secondary to a behavioural response; as women feel more confident that they will not leak, so they learn to hold on for longer.
It is difficult from reading the literature to establish whether our incidence of pain, particularly angle pain, is high. The incidence of post-operative pain is often not addressed by authors. We specifically did so because we knew from our clinical practice that it was sometimes a problem. Barrington et al. [11] stated that complications, apart from post-operative pain, were rare but did not state what the incidence was. Wadie et al. [17] found that 7 of 15 women (47%) had wound pain at 6-month follow-up. This, however, did not appear to be as formally assessed as we have done. We believe that our incidence appears high because we specifically asked about it.
The question of how to address non-responders is much debated. Most published papers on incontinence surgery give no information of how they addressed the missing data or the possible bias that this introduces. It may be reasonable to ignore missing data, if you can assume that the data are equally missing in all groups for the same reasons. It may, however, be missing unequally due to patient perceptions of the procedure and success therefore introducing a significant bias.
We addressed the problem by giving a range of possible results, from best to worse possible. This led to a wide range of possible results to interpret. It is impossible to know what our true success rate is. We can only state that it lies somewhere between these values. The impact of assuming all non-responders are failures is highlighted by the fact that the only statistical difference between the groups arose possibly secondary to a higher rate of non-responders in one group rather than due to one sling technique being superior to the other. This finding was also highlighted by Ward et al. [25] in the UK TVT RCT, where they found that in the ITT arm, TVT performed better than colposuspension.
It is often assumed that the long-term outcomes of sling techniques differ little from the short-term outcomes, and that this indicates durability. Indeed, this has been used as a justification for some newer mid-urethral tape procedures not needing long-term data before being widely promoted as a valid surgical choice for women with SUI. The long-term outcome measures in this trial, however, show a gradual increase/return in symptoms. The incidence of symptoms appears to be nearing baseline more rapidly than the average scores for symptoms or QoL. Whilst this means that the effect is maintained by 5 years, the issue of how much longer it remains improved for is unanswered. It may be that autologous slings have a finite life span before patients return to baseline symptoms. This may be a fact off all types of incontinence surgery and makes it all the more imperative that new surgical techniques are able to demonstrate long-term equivalence before widespread adoption. There are no 10- to 15-year follow-up RCTs at present to answer these questions.
Conclusion
Autologous rectus fascial slings are an effective treatment for the management of SUI in women. The modified ‘sling-on-a-string’ technique appears to be as effective as a standard sling in the long term. In view of it being a quicker procedure that causes less post-operative pain, the ‘sling-on-a-string’ should be the preferred autologous sling technique. We have adopted this as our standard autologous sling procedure. The long-term outcomes are acceptable, but there is a trend towards baseline, which cannot presently be compared to any other procedure for stress incontinence. Robust comparisons of new techniques using synthetic and non-autologous biological slings are essential.
References
Royal College of Obstetricians and Gynaecologists (2003) Surgical treatment of urodynamic stress incontinence. Green-top guideline no. 35. October
Abrams P, Hilton P, Lucas M, Smith T (2005) A proposal for a new classification for operative procedures for stress urinary incontinence. BJU Int 96:232–233
Aldridge A (1942) Transplantation of fascia for the relief of urinary stress incontinence. Am J Obstet Gynecol 44:398–441
Bidmead J, Cardozo L (2000) Sling techniques in the treatment of genuine stress incontinence. BJOG 107(2):147–156
Leach GE, Dmochowski RR, Appell RA, Blaivas JG, Hadley HR, Luber KM, Mostwin JL, O’Donnell PD, Roehrborn CG (1997) Female Stress Urinary Incontinence Clinical Guidelines Panel summary report on surgical management of female stress urinary incontinence. J Urol 158(3):875–880
Bemelmans BLH, Chapple CR (2003) Are slings now the gold standard treatment for the management of female urinary stress incontinence and if so which technique? Curr Opin Urol 13:301–307
Kobashi KC, Govier F (2005) The completely dry rate: a critical re-evaluation of the outcomes of slings. Neurourol Urodyn 24:602–605
Department of Health (UK) (2006) Hospital episodes statistics. Department of Health [online]. Available from: URL: http://www.hesonline.nhs.uk
Schumaker SA, Wyman JF, Uebersax JS, McClish D, Fanti JA for the Continence Program in Women (CPW) Research Group (1994) Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Qual Life Res 3:291–306 (Rapid communications of Oxford Ltd, Oxford)
Uebersax JS, Wyman JF, Schumaker SA, McClish D, Fanti JA (1995) Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Neurourol Urodyn 14:131–139
Barrington JW, Fulford SCV, Bales G, Stephenson TP (1998) The modified rectus fascial sling for genuine stress incontinence. J Obstet Gynaecol 18:61–62
Fulford SCV, Flynn R, Barrington J, Appanna T, Stephenson TP (1999) An assessment of the surgical outcome and urodynamic effects of the pubovaginal sling for stress incontinence and the associated urge syndrome. J Urol 162:135–137
Simsiman AJ, Powell CR, Stratford RR, Menefee SA (2005) Suburethral sling materials: best outcome with autologous tissue. Am J Obstet Gynecol 193:2112–2116
National Institute for Health and Clinical Excellence (UK): Interventional procedure guidance 154. Insertion of biological slings for stress urinary incontinence in women. www.nice.org.uk/IPG154
Bezerra CA, Bruschini H, Cody DJ (2005) Traditional suburethral sling operations for urinary incontinence in women. The Cochrane Database of Systematic Reviews (3): CD001754. DOI 10.1002/14651858. CD001754.pub2
Clyne OJ, O’Sullivan O, Flood HD (2005) Pubovaginal sling for urodynamic stress incontinence: effect on patient quality of life. Ir Med J 98(3):75–77
Wadie BS, Edwan A, Nabeeth AM (2005) Autologous fascial sling vs. polypropylene tape at short-term follow-up: a prospective randomised study. J Urol 174:990–993
Bai SW, Sohn WH, Chung DJ, Park JH, Kim SK (2005) Comparison of the efficacy of Burch colposuspension, pubovaginal sling, and tension-free vaginal tape for stress urinary incontinence. Int J Gynaecol Obstet 91:246–251
McBride AW, Ellerkmann RM, Bent AE, Melick CF (2005) Comparison of long-term outcomes of autologous fascia lata slings with suspend tutoplast fascia lata allograft slings for stress incontinence. Am J Obstet Gynecol 192:1677–1681
Maher CF, O’Reilly BA, Dwyer PL, Carey MP, Cornish A, Schulter P (2005) Pubovaginal sling versus transurethral macroplastique for stress urinary incontinence and intrinsic sphincter deficiency: a prospective randomised control trial. BJOG 112:797–801
Corcos J, Collet JP, Shapiro S, Herschorn S, Radomski SB, Schick E, Gajewski JB, Benedetti A, Macramallah E, Hyams B (2005) Multicenter randomised clinical trial comparing surgery and collagen injection for treatment of female stress urinary incontinence. Urology 65(5):898–904
Morgan TO, Westney OL, McGuire EJ (2000) Pubovaginal sling: 4-year outcome analysis and quality of life assessment. J Urol 163:1845–1848
Blaivas JG, Jacobs BJ (1991) Pubovaginal fascial sling for the treatment of complicated stress urinary incontinence. J Urol 145:1214–1218
Hilton P (2002) Trials of surgery for stress incontinence—thoughts on the ‘Humpty Dumpty principle’. BJOG 109:1080–1081
Ward KL, Hilton P, UK & Ireland TVT Trial Group (2004) A prospective multicenter randomised trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol 190:324–331
Acknowledgement
The study was supported by a grant from the Welsh Office of Research and Development.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guerrero, K., Watkins, A., Emery, S. et al. A randomised controlled trial comparing two autologous fascial sling techniques for the treatment of stress urinary incontinence in women: short, medium and long-term follow-up. Int Urogynecol J 18, 1263–1270 (2007). https://doi.org/10.1007/s00192-007-0307-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-007-0307-y