Abstract
The objectives of this study are to determine whether patients with overactive bladder (OAB) and nocturia achieved relief of their nighttime voiding symptoms when treated with solifenacin and whether having nocturnal polyuria (NP) affected that response. The patients pooled from four phase III clinical trials were evaluated for reductions in nocturia episodes after treatment with solifenacin (5 or 10 mg) or placebo. A second analysis was performed in patients with and without NP. The patients treated with solifenacin experienced statistically significant reductions in nocturia episodes; median reductions were −35.5% for 5 mg of solifenacin and −36.4% for 10 mg of solifenacin compared with −25.0% for placebo, and significantly more patients treated with solifenacin vs placebo achieved a mean nocturic frequency of ≤1 episode/night. Solifenacin significantly reduced nocturia episodes only in patients without NP (mean change was −0.61 episodes/night for both doses compared with −0.43 episodes for placebo). Solifenacin significantly improved nocturia symptoms only in OAB patients without NP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nocturia is defined by the International Continence Society (ICS) as the complaint that an individual has to wake at night one or more times to void [1]. The cause of nocturia in a given patient may be challenging to diagnose or multifactorial in nature. Nocturia can have several etiologies, including nocturnal overproduction of urine (nocturnal polyuria [NP]), low bladder capacity (including overactive bladder [OAB]), and a combination of NP and low bladder capacity. Causes of NP include renal conditions, congestive heart failure, diabetes mellitus or insipidus, cerebrovascular damage, third space fluid resorption, fluid shifts, medications such as diuretics, sleep disorders or apnea, and behavioral or environmental factors.
Nocturia is greatly under-reported by both physicians and patients and commonly is perceived as a normal part of the aging process [2, 3]. It is a condition that often is trivialized, and its consequences are greatly underestimated [2]. Living with nocturia diminishes overall well-being, vitality, and productivity and is associated with impairment of somatic and mental health as well as increased sick leave [4, 5]. Health-related quality-of-life surveys showed that the quality of life decreased with increase in the number of voids per night and reductions in the number of hours slept, with men and women affected equally [6]. Nocturia is an important risk factor for nighttime falls in the elderly [7] and is associated with increased overall mortality in patients voiding at least three times nightly [8].
OAB has been defined by the ICS as a symptom complex that includes urinary urgency, with or without urge incontinence, usually accompanied by urinary frequency and nocturia [9]. When OAB is the underlying cause of, or contributor to the nocturia, treatment directed at the bladder overactivity may provide nocturia relief.
Although anticholinergic treatments are commonly prescribed by clinicians for patients with OAB that includes nocturia, there are very few published data to support this practice. Based on the relationship between OAB and nocturia, we hypothesized that patients with nocturia and OAB would respond to treatment with antimuscarinic agents. The antimuscarinic agent, solifenacin, has been shown to be efficacious in reducing incontinence, urgency, and frequency and increasing volume voided per micturition in four placebo-controlled phase III clinical trials [10–12]. A subset analysis employing pooled data was used to assess changes in nocturia symptoms in patients treated with solifenacin versus placebo. As the nocturia experienced by patients in this pooled population had multiple etiologies, additional ad hoc analyses were performed based on whether or not patients had NP at baseline. We reasoned that patients with NP would be less likely to experience an improvement in nocturia from antimuscarinic treatment compared with patients without NP.
Materials and methods
Analyses were performed on data from four 12-week phase III clinical trials consisting of 3,298 randomized patients. All four studies had similar protocols, inclusion criteria, and demographics thus enabling the pooling of data. In these studies, patients with symptoms of OAB (≥8 daily voids with ≥1 episode of incontinence and/or ≥1 episode of urgency per 24 h) completed the consecutive 3-day voiding diaries. The patients were randomized to one of the three treatment regimens: 10 mg of solifenacin (all four trials), 5 mg of solifenacin (two trials), or placebo. A single within-study cohort treated with tolterodine 2 mg bid (n = 266) was not included in the analysis because the study was not powered for this arm.
The participants in the four trials consisted of men and women at least 18 years of age with a mean of eight or more micturitions per 24 h and a mean of one or more incontinence or urgency episodes per 24 h based on a 3-day micturition diary period. The patients completed a 3-day micturition diary at baseline and at weeks 4, 8, and 12. The patients recorded the date and time of each episode, whether or not they voided, the presence of urgency and/or of incontinence, the volume voided (for 2 of the 3 days), and whether or not the episode interrupted their sleep. The time of rising from, and retiring to, bed also were reported for each day of the diary period.
A nocturnal void included any void that occurred after the subject went to bed, and nocturia was defined as ≥1 voiding episode per night, which the study participant indicated was responsible for an interruption of sleep. This was determined in the voiding diary, which contained a check box for the patients to mark if they believed that their sleep was disturbed by the need to void. The mean change in nocturia episodes from baseline to week 12 were calculated using last observation carried forward (LOCF). Treatment group comparisons were based on an analysis of covariance (ANCOVA) model with terms for treatment group, center, and baseline nocturic frequency included as covariates. Treatment group comparisons of percent change are based on van Elteren’s test [13] using standardized mid-ranks and stratified by pooled center.
The proportion of subjects with at least a 50% reduction in nocturia was calculated. Treatment group comparisons were based on Fisher’s exact test.
Responders in the nocturia cohort were defined as patients who had ≥1 episode/24 h at baseline and <1 episode/24 h at end point. Participants with <1 episode/24 h are, by definition, experiencing at least one night in three that is not disturbed by nocturia. Treatment group comparisons of the percent of responders also were based on Fisher’s exact test.
The second ad hoc analysis was performed on patients who provided diary data at their 12-week visit (LOCF was not applied to this analysis) to evaluate the response to solifenacin in two groups, those with NP and those without NP. Patients were considered to have NP based on a definition that takes into account the exact number of hours spent asleep and the fraction of urine output expected during that time as described by Weiss and Blaivas [14]: nocturnal urinary volume > (number of hours of sleep/24) × 24 h urinary volume. Nocturnal diuresis rate and total daily diuresis rate were defined as nocturnal voided volume/nocturnal void time and total voided volume/total void time, respectively. The nocturnal voided volume included all nocturnal voids and first void of the next diary day. Total voided volume included all voids after the first void upon waking through the first void of the next diary day. Nocturnal void time was the time in minutes between bedtime and the first void time of the next day. Total void time was the time in minutes between first void time and the first void time of the next day. For patients with and without NP at baseline, changes from baseline to week 12 in the number of nocturia episodes per 24 h were calculated. Treatment group comparisons of the change from baseline were based on a ranked ANCOVA model with terms for treatment group and baseline in the model.
Results
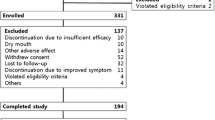
Of the 3,032 randomized patients in the pooled population, 2,534 patients (84%) reported nocturia as a symptom at baseline and were included in this analysis. Of these, 1,005 were treated with placebo, 494 were treated with 5 mg of solifenacin, and 1,035 were treated with 10 mg of solifenacin. The patients treated with solifenacin experienced statistically significant reductions in the number of nocturia episodes per 24 h (Fig. 1; Table 1). In addition, a significant percentage of subjects treated with solifenacin achieved a 50% or greater reduction in nocturia.
Sixty-two percent (997/1,599) of the patients reporting nocturia were classified as having NP. The patients without NP at baseline who were treated with 5 or 10 mg of solifenacin experienced a greater mean reduction of 0.61 ± 1.05 (range from −4.0 to 3.5) from baseline in nocturia episodes (P = 0.026 for the 5-mg dose and P = 0.006 for the 10-mg dose) than patients taking placebo (mean change −0.43 ± 1.01, range from −3.0 to 3.0; Table 2).
A statistically and clinically significant greater percentage of patients with >1 nocturia episode nightly reported ≤1 episode of nocturia after solifenacin treatment as compared with patients receiving placebo. For patients in the 5- and 10-mg solifenacin treatment groups, 45% (159/355; P = 0.004) and 44% (298/679; P = 0.001) of patients, respectively, reported ≤1 nocturia episode at end point versus 35% (228/647) of patients taking placebo. When this responder analysis was performed on the subcohort of patients without NP, significance was confirmed in favor of the solifenacin treatment. Among patients without NP, 63% (P = 0.018 vs placebo) and 61% (P = 0.013 vs placebo) in the two treatment arms (5 and 10 mg of solifenacin, respectively) reported ≤1 episode of nocturia at study end in comparison to 45% of patients in the placebo group.
As clinically expected, participants with NP experienced more episodes of nocturia at baseline (mean 2.33 ± 1.54, 2.32 ± 1.31, and 2.27 ± 1.40 for the subjects in the placebo, 5-mg treatment group, and 10-mg treatment group, respectively, range 0.5–15.0 episodes nightly) than participants without NP (mean 1.70 ± 0.99, 1.66 ± 0.88, and 1.66 ± 0.95 for the subjects in the placebo, 5-mg treatment group, and 10-mg treatment group, respectively, range 0.5–7.0 episodes nightly). In patients with NP, there was a mean reduction from baseline in nocturic frequency of 0.72 ± 1.15 (range from −3.5 to 3.5) and 0.68 ± 1.16 (range from −4.5 to 3.0) nightly episodes after 12 weeks of treatment with 5 and 10 mg of solifenacin, respectively. These reductions were not statistically or clinically different when compared with the placebo group with NP (mean change −0.64 ± 1.29, range from −5.0 to 5.5; Table 2). These findings are consistent with the supposition that solifenacin treatment would not provide significant reductions in nocturia episodes for patients whose OAB is complicated by NP.
Discussion
Overall, our analysis confirmed a statistically significant reduction in episodes of nocturia after 12 weeks of solifenacin treatment for the full cohort reporting nocturia at baseline, with 45% of patients achieving a clinically significant end point, i.e., an average of ≤1 nocturia episode nightly. The most important clinical finding from this analysis may be that solifenacin provided significant nocturia relief for patients with OAB and nocturia that was not complicated by NP, with more than 60% achieving an average of ≤1 nocturic episode nightly by study end. Patients with NP did not experience significant improvement in their nocturic frequency. The finding that 62% of the patients in the present study reporting nocturia were further classified as having NP coincides with a recently published study [15] in which a similar proportion of women who complained of nocturia and OAB symptoms were further classified as having NP (56%; 31/55). An earlier publication suggested that 43% (83/194) of their study population experienced nocturnal overproduction of urine [16].
There have been prior studies describing nocturia relief with anticholinergic treatment [17–20]. One small study compared behavioral interventions and treatment with an immediate-release oxybutynin, reporting reductions in episodes of nocturia: The authors reported statistically significant but clinically insignificant reductions in nocturia both in patients receiving oxybutynin (P = 0.007) and in those receiving behavioral interventions (P < 0.001), compared to patients receiving placebo. Mean reductions of 0.2 episodes in nocturia were reported for patients in the drug treatment group versus reductions of −0.1 episodes for patients receiving placebo [17].
Another, post hoc analysis from a trial of an immediate-release tolterodine included data on changes in episodes of nocturia: Results were presented using responder rates, characterized as patients reporting ≥2 nighttime voids at baseline and ≤2 nighttime voids after treatment, and the majority of patients responded to therapy based on this definition [18].
Three multicenter, double-blind, placebo-controlled studies of patients with OAB symptoms evaluated treatment with darifenacin (7.5 or 15 mg qd) for 12 weeks. In this pooled analysis, the number of “nocturnal awakenings” per week was examined as a secondary efficacy variable. A nonsignificant reduction in “nocturnal awakenings” was observed in darifenacin-treated patients compared with patients administered placebo [19]. The lack of significant findings may have been due to the inclusion of patients with nocturia with NP and without NP.
A single placebo-controlled trial of darifenacin administered at three dosing strengths (7.5 mg, 15 mg, and 30 mg qd) utilized the same definition of “nocturnal awakenings” to evaluate changes from baseline with treatment. The magnitude of the reductions in nocturia were larger, (−1.9, −1.7, and −2.0 per week with increasing dose) and reached statistical, but probably not clinical significance, for all dosing groups [20].
There are limitations to this secondary analysis. Nocturia was not a study inclusion criterion, and, on average, the participants did not have a large number of nocturia episodes (mean of 1.8 for the placebo and 10-mg treatment groups and 2.0 for the 5-mg treatment group at baseline). Therefore, demonstrating effects on nocturia was difficult, and investigators relied upon patient-based reporting of nocturia episodes and the reasons for sleep interruption. Importantly, we acknowledge that there remains variability in the accepted diagnosis of NP and the definitions of NP and nocturia for evaluation in clinical trials.
Despite these limitations, we did find that solifenacin treatment significantly improved nocturic frequency in patients without NP, suggesting that screening for NP may enhance clinical care for the patient with troublesome nocturia. Findings from this initial analysis, coupled with the lack of consensus regarding definitions of nocturia in the clinical trial literature, underscore the need for further research in this important area.
Future studies could record baseline disease states (such as metabolic conditions, congestive heart failure, obstructive sleep apnea, or diabetes) to further evaluate the relationships between specific pathological conditions underlying nocturia and responses to antimuscarinic treatment. Patients also could be divided into groups before treatment is administered based on whether the apparent underlying cause of nocturia is polyuria, NP, or OAB. More precise identification of patients with nocturia who would be likely to benefit from antimuscarinic treatment will enable clinicians to make informed prescribing decisions.
References
van Kerrebroeck P, Abrams P, Chaikin D et al (2002) The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:179–183
Lundgren R (2004) Nocturia: a new perspective on an old symptom. Scand J Urol Nephrol 38:112–116
Svatek R, Roche V, Thornberg J, Zimmern P (2005) Normative values for the American Urological Association Symptom Index (AUA-7) and short form Urogenital Distress Inventory (UDI-6) in patients 65 and older presenting for non-urological care. Neurourol Urodyn 24:606–610
Asplund R, Marnetoft SU, Selander J, Akerstrom B (2005) Nocturia in relation to somatic health, mental health and pain in adult men and women. BJU Int 95:816–819
Kobelt G, Borgstrom F, Mattiasson A (2003) Productivity, vitality and utility in a group of healthy professionally active individuals with nocturia. BJU Int 91:190–195
Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E (2003) The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA. BJU Int 92:948–954
Stewart RB, Moore MT, May FE, Marks RG, Hale WE (1992) Nocturia: a risk factor for falls in the elderly. J Am Geriatr Soc 40:1217–1220
Asplund R (1999) Mortality in the elderly in relation to nocturnal micturition. BJU Int 84:297–301
Abrams P, Cardozo L, Fall M et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178
Cardozo L, Lisec M, Millard R et al (2004) Randomized, double-blind placebo controlled trial of the once daily antimuscarinic agent solifenacin succinate in patients with overactive bladder. J Urol 172:1919–1924
Chapple CR, Rechberger T, Al-Shukri S et al (2004) Randomized, double-blind placebo- and tolterodine-controlled trial of the once-daily antimuscarinic agent solifenacin in patients with symptomatic overactive bladder. BJU Int 93:303–310
Gittelman M, Chu F, Klimberg I, Fincher R, Smith N, Tempel D, Ridge S (2003) Two randomized, double-blind, placebo-controlled, parallel-group, fixed-dose, multicenter studies assess the efficacy and safety of daily oral administration of 10 mg YM905 (solifenacin succinate; Vesicare®) versus placebo in male and female subjects with overactive bladder. Poster presented at the American Urological Association Annual Meeting; April 26–May 1, 2003; Chicago, IL (on behalf of the YM905 Study Group)
van Elteren PH (1960) On the combination of independent two-sample tests of Wilcoxon. Bull Inst Int Stat 37:351–361
Weiss JP, Blaivas JG (2000) Nocturia. J Urol 163:5–12
Drake NL, Flynn MK, Romero AA, Weidner AC, Amundsen CL (2005) Nocturnal polyuria in women with overactive bladder symptoms and nocturia. Am J Obstet Gynecol 192:1682–1686
Weiss JP, Blaivas JG, Stember DS, Brooks MM (1998) Nocturia in adults: etiology and classification. Neurourol Urodyn 17:467–472
Johnson TM II, Burgio KL, Redden DT, Wright KC, Goode PS (2005) Effects of behavioral and drug therapy on nocturia in older incontinent women. J Am Geriatr Soc 53:846–850
Kreder KJ Jr, Brubaker L, Mainprize T (2003) Tolterodine is equally effective in patients with mixed incontinence and those with urge incontinence alone. BJU Int 92:418–421
Chapple C, Steers W, Norton P et al (2005) A pooled analysis of three phase III studies to investigate the efficacy, tolerability and safety of darifenacin, a muscarinic M selective receptor antagonist, in the treatment of overactive bladder. BJU Int 95:993–1001
Hill S, Khullar V, Wyndaele JJ, Lheritier K (2005) Dose response with darifenacin, a novel once-daily M(3) selective receptor antagonist for the treatment of overactive bladder: results of a fixed dose study. Int Urogynecol J Pelvic Floor Dysfunct 17(3):239–247
Acknowledgement
The authors would like to thank Linda Gorman, Ph.D. and Ellen Lewis, Ph.D. of Envision Pharma for their assistance with the writing and preparation of this manuscript. Funding for the analysis of this data was provided by Yamanouchi Pharma America (now Astellas) and GlaxoSmithKline.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brubaker, L., FitzGerald, M.P. Nocturnal polyuria and nocturia relief in patients treated with solifenacin for overactive bladder symptoms. Int Urogynecol J 18, 737–741 (2007). https://doi.org/10.1007/s00192-006-0239-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-006-0239-y