Abstract
Purpose: To determine the efficacy of tension-free vaginal tape (TVT) for the treatment of five sub-types of stress urinary incontinence (SUI).
Materials and methods: A retrospective review was performed from November 1998 to November 2001 on all patients with SUI who underwent a TVT procedure either alone or with other reconstructive pelvic procedures. The patients were subdivided into five categories. Intrinsic sphincter deficiency (ISD) was defined by a maximum urethral closure pressure <20 cm H2O or a mean Valsalva leak point pressure <60 cm H2O above baseline. Urethral hypermobility (UH) was defined by a straining Q-tip angle greater than 30° from the horizontal. Cure was defined as the subjective resolution of SUI without the development of voiding dysfunction or de novo urge incontinence. Improvement was defined as the subjective improvement of SUI without complete resolution or the subjective resolution of SUI occurring with the development of prolonged voiding dysfunction lasting greater than 6 weeks or de novo urge incontinence. Failure was defined as the subjective lack of improvement of SUI, the need for an additional procedure to correct SUI or the need for revision or takedown of the TVT for persistent voiding dysfunction or mesh erosion.
Results: The cure, improvement and failure rates for each of the following groups are respectively as follows: group 1 (+UH, -ISD) (n=121): 101 (83.5%), 13 (10.7%), 7 (5.8%); group 2 (-UH, +ISD) (n=22): 17 (77.3%), 3 (13.6%), 2 (9.1%); group 3 (+UH, +ISD) (n=32): 26 (81.3%), 4 (12.5%), 2 (6.2%); group 4 (-UH, -ISD) (n=25): 21 (84.0%), 3 (12.0%), 1 (4.0%); group 5 (occult SUI) (n=67): 57 (85.1%), 10 (14.9%), 0 (0%).
Conclusion: This study shows that the TVT is effective in treating all five sub-types of SUI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A significant amount of effort is made to classify stress urinary incontinence (SUI) and quantify the severity of disease [1, 2]. In general, SUI is categorized as urethral hypermobility (UH) (types 1 and 2) based on a Q-tip test, ultrasound or video study or intrinsic sphincter deficiency (ISD) (type 3) based on a leak-point pressure or a static maximum urethral closure pressure. Traditionally, these classifications helped to decide the best procedure for each patient. In 1996, Ulmsten et al. introduced the tension-free vaginal tape (TVT) [3]. Without providing any additional support to the bladder neck, it was designed to treat SUI with UH, and has been shown to be as efficacious as more traditional procedures [4]. Studies, however, have shown the TVT to also be effective in treating ISD [5, 6].
This brings to question whether our efforts are futile in trying to quantify UH and urethral function. SUI is a multifactorial condition and current concepts of SUI with UH and ISD are perhaps overly simplistic [7]. We analyze five categories or subtypes of SUI. Our objective is to determine the efficacy of the TVT for the treatment of SUI based on the five subtypes that we have defined.
Materials and methods
A retrospective review was performed on all patients from the senior author’s (MMK) practice who underwent a TVT either alone or with other reconstructive pelvic procedures from November 1998 to November 2001. All patients presented with symptoms of urinary incontinence or pelvic organ prolapse and had a diagnosis of urodynamic SUI. Preoperatively, all patients completed two quality-of-life questionnaires, the Incontinence Impact Questionnaire (IIQ-7) and Urinary Distress Inventory (UDI-6) [8]. A standardized history was obtained at the initial office visit. At this time, a standardized exam using the Baden–Walker system was performed to assess vaginal support, and bladder neck support was assessed utilizing a Q-tip test. Simple uroflowmetry and simple office cystometry were also performed.
On a subsequent visit, all patients had a multichannel urodynamic study consisting of subtracted filling cystometry, measurement of maximum urethral closure pressures, and leak-point pressures in a standardized fashion as well as a pressure flow study. Urodynamic studies were performed with the patient in the sitting position. An 8 Fr dual-sensor microtip transducer catheter with sensors 6 cm apart was used to record vesicle and urethral pressures simultaneously. An 8 Fr single microtip transducer catheter was placed in the vagina, and if the patient had significant pelvic organ prolapse, it was placed in the rectum. After emptying the bladder with a catheter, normal saline was used to fill the bladder at a rate of 55 ml/min. At a bladder volume of 150 ml and at maximum bladder capacity, Valsalva leak-point pressures were measured. If a Valsalva maneuver did not produce urinary leakage, the patient was asked to cough vigorously three times in a row. If no leakage was noted at maximum capacity with provocative maneuvers and the patient had vaginal wall prolapse, the prolapse was reduced with half a speculum. Special care was taken to avoid flattening of the urethrovesical angle or downward traction on the levator muscles. ISD was defined by a maximum urethral closure pressure <20 cm H2O or a mean Valsalva leak-point pressure <60 cm H2O above baseline. UH was defined by a straining Q-tip angle greater than 30° from the horizontal.
Based on these studies, patients who demonstrated SUI were subdivided into the following five categories: Group 1, patients with isolated straining Q-tip >30° and normal urethral function tests (+UH, -ISD); Group 2, patients with isolated ISD and a well-supported bladder neck (-UH, +ISD); Group 3, patients with combined UH and urethral function tests consistent with ISD (+UH, +ISD); Group 4, patients with a well-supported bladder neck and normal urethral function tests (-UH, -ISD); and Group 5, patients with pelvic organ prolapse and occult incontinence in which SUI only occurs when the prolapse is manually reduced (occult SUI). Patients in Group 5 were then further analyzed by subdividing them into Groups 1–4 as just described. Any patient with a follow-up time less than 6 weeks or with an undocumented Q-tip test at the time of the initial examination was excluded from the study.
A TVT suburethral sling was performed on all patients as described by Ulmsten et al.[9], with the exception of minor adjustments made to accommodate those patients undergoing concomitant surgery to treat pelvic organ prolapse. A voiding trial as described by Kleeman et al. [10] was performed on all patients prior to discharge. If patients failed their voiding trial, they were discharged to their homes with a Foley catheter. At a 1-week follow-up visit, if patients still could not spontaneously void, the Foley catheter was either reinserted or the patient was taught how to perform intermittent self-catheterization. Patients were evaluated at 2 and 6 weeks post-operatively and then at 3 months and 1 year. Each patient was also asked to complete the same quality-of-life questionnaires post-operatively.
Outcome measures were categorized as follows: cure was defined as the subjective resolution of SUI without the development of voiding dysfunction or de novo urge incontinence. Improvement was defined as the subjective improvement of SUI without complete resolution or the subjective resolution of SUI occurring with the development of prolonged voiding dysfunction lasting ≥6 weeks or de novo urge incontinence. Failure was defined as the subjective lack of improvement of SUI, the need for an additional procedure to correct SUI or the need for revision or takedown of the TVT for persistent voiding dysfunction or mesh erosion.
To determine if there were any differences in demographics between groups, ANOVA (analysis of variance) was used to evaluate age, BMI and parity and chi-square test was used to evaluate menopausal status, hormone replacement status, and prior incontinence surgery. ANOVA was performed to determine whether there was a statistically significant difference of cure rates between groups. Students paired samples t-test was used to compare the pre- and postoperative scores for the IIQ-7 and the UDI-6. Pearson chi-square analysis was performed to determine if preoperative urinary symptoms (stress or mixed), history of previous anti-incontinence surgery, type of anesthesia (intravenous sedation with local, general, epidural), or anterior colporrhaphy performed in conjunction with the TVT were predictors of the outcome.
Results
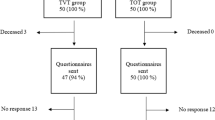
Three hundred and nineteen patients underwent a TVT suburethral sling during the study period. Fiftytwo were excluded (36 for a follow-up time <6 weeks and 16 for an undocumented Q-tip test at the time of the initial exam), leaving a total of 267 patients. Demographic data are summarized in Table 1. There were no significant differences found in demographics based on group with P values as follows: age 0.19, BMI 0.85, parity 0.32, menopausal status 0.45, hormone replacement therapy 0.197 and prior incontinence surgery 0.126. The median follow-up time was 3.0 months with a range from 1.5 to 35 months. Concomitant surgeries were performed on 213 patients (79.8%) at the time of the TVT suburethral sling and are listed in Table 2.
Outcome for each of the five subtypes of SUI is shown in Table 3. There was not a statistically significant difference of cure rates between groups (P=0.796). Of the 33 patients who showed an improvement following the TVT, 18 developed de novo urge incontinence, nine had prolonged voiding dysfunction lasting ≥6 weeks, and six had subjective improvement of SUI without complete resolution. In the failed group, four had no improvement following the TVT. Of these, three had subsequent injection of a bulk-enhancing agent and one had a retropubic urethropexy. There were an additional eight patients who had a takedown or revision of their TVT, six secondary to voiding dysfunction and two secondary to vaginal erosion of the prolene mesh.
Group 5 (occult SUI) consisting of 67 patients was further analyzed by subcategorizing them into Groups 1–4 as previously described. The cured and improved rates for each group, which are summarized in Table 4 were, respectively, Group 1 (n=46): 41 (89.1%), 5 (10.9%); Group 2 (n=4): 2 (50.0%), 2 (50.0%); Group 3 (n=9): 8 (88.9%), 1 (11.1%); and Group 4 (n=8): 6 (75.0%), 2 (25.0%). There were no failures in any of these groups. Pre- and postoperative quality-of-life questionnaires were completed by 189 (70.8%) patients. Table 5 summarizes the overall pre- and postoperative scores for the IIQ-7 and UDI-6 as well as the three subscales of the UDI-6 by subtype of SUI.
Using Pearson chi-square analysis, it was determined that neither preoperative urinary symptoms (stress or mixed), history of previous anti-incontinence surgery, type of anesthesia (intravenous sedation with local, general, epidural), nor anterior colporrhaphy performed in conjunction with the TVT were predictors of outcome. The P values were, respectively, 0.202, 0.213, 0.628, and 0.507.
Discussion
Although the mechanisms of urinary stress incontinence are not fully understood, it is believed to occur either when increases in intra-abdominal pressure are not equally transmitted to the bladder and proximal urethra or when the urethra no longer functions as a sphincter and thus is not able to maintain a water-tight seal. Based on these suspected etiologies, various classifications of SUI have been described [1, 2]. While suburethral slings act as a hammock to stabilize the urethra at rest and compress it with increased abdominal pressure, the proposed mechanism of action of the TVT is to reinforce the pubourethral ligaments at the level of their functional insertions at the midurethra as well as to support the suburethral vaginal wall [3]. However, the true mechanism of action of the TVT remains uncertain.
An analysis of five subtypes of SUI is presented to account for the wide variety of presentations that one may encounter. The authors feel it is more precise to think of SUI as a spectrum of disease with UH (types 1 and 2 incontinence) on one end, and ISD (type 3 incontinence) on the other end. However, certain women do not fall into either category, such as women who have urodynamic SUI with a well-supported bladder neck and normal urethral function tests. Also, a significant number of women with advanced prolapse will have occult incontinence with a reduction maneuver [11]. The overall results of our study, taking into account all five subtypes of stress incontinence, are similar to the long-term follow-up results reported by Nilsson et al. [4].
Although the TVT suburethral sling was originally described as a technique to treat SUI with UH, studies comparing pre- and postoperative Q-tip tests following the TVT showed that cure does not require the correction of proximal UH [12, 13]. This observation has led others to suspect that the TVT may also work well in women who do not meet the criteria for UH. Our results of the TVT for patients with ISD are similar to the success rate of 79% reported by Mutone et al [6].
The incidence of ISD combined with UH may be higher than what was previously thought [14]. The clinical significance of ISD with UH remains unknown. Few studies have looked at surgical cure rates of combined ISD and UH. Rezapour et al. [5] studied 49 patients with ISD, 41 of whom also had UH, after a TVT. They found that 74% were cured, 12% improved, and 14% failed, and that those with an immobile urethra had worse outcomes [5]. Our results indicate the TVT is equally efficacious in treating patients with ISD and UH.
Patients in Group 4 (-UH, -ISD) are interesting because, although they complain of symptoms of urinary incontinence and have urodynamic SUI, they have normal anatomic support and a functional urethra based on physiologic testing. This further illustrates our present lack of understanding of SUI and provides further support that our current means of classifying SUI is overly simplistic. Although fluoroscopy was not done, the patients in Group 4 (-UH, -ISD) most likely have type 1 SUI in which there is minimal UH and normal urethral closure pressures associated with urinary loss. Our study demonstrates that the TVT also works equally well in this group of patients.
Controversy still remains as to whether patients with advanced vaginal wall prolapse, who demonstrate SUI only with reduction of their prolapse, require an anti-incontinence procedure. It is possible that one can cause iatrogenic leakage on exam with reduction of the prolapse either by straightening of the urethrovesical junction or by depressing the levator ani muscles. It is also possible that asymptomatic patients who undergo vaginal surgery for genital prolapse may develop SUI post-operatively due to lack of additional support to the bladder neck, as well as possible periurethral fibrosis, scarring and partial urethral denervation.
Our study supports the findings of Gordon et al. [15] evaluating the outcomes of 30 women with occult SUI following a TVT and prolapse repair [15]. We further analyzed this subgroup of patients with occult incontinence by determining the type of incontinence these patients had based on UH and urethral function tests. Although there were only four patients with occult incontinence who had isolated ISD, only half of these patients were cured following a TVT. This may be a possible predictor for failure following a TVT and should be further explored.
In reviewing a multitude of possible outcome predictors, none were found to be statistically significant. One would intuitively think that those with previous anti-incontinence surgeries would have a greater risk of failure secondary to possible scarring and nerve damage, but this was not found to be a risk factor. One would also think that those with mixed symptoms of urinary incontinence may be more difficult to treat because of the coexisting urge component, but this also was not found to be a predictor of outcome.
There are several strengths to the study. To the best of our knowledge, this is the first study to evaluate the efficacy of the TVT in all five subtypes of SUI that were defined prior to starting the study. The study is also the first to account for the underlying cause of SUI in those with occult urinary incontinence. In trying to determine whether the TVT was effective in treating stress incontinence, we felt it was important to incorporate associated untoward effects of the TVT in our outcome measures, including voiding dysfunction and de novo urge incontinence.
The major limitations of the study include the relatively short follow-up times for some patients and the lack of objective outcome measures. Our outcomes based on subjective symptoms from a chart review used less stringent criteria when compared to other studies that used pad tests and filling cystometry. However, in order to better objectify patients’ symptoms, we compared validated quality-of-life questionnaires pre- and post-operatively. We found statistically significant improvements in all five subgroups, except for the voiding dysfunction subscale of the UDI-6 in Group 4 which showed improvement but did not reach statistical significance.
The study brings out several questions that need to be better addressed through future research. Considering the TVT is effective in treating all types of SUI, how important is it to differentiate UH from ISD? Additionally, how important is it to assess bladder neck mobility, especially considering the fact that the TVT is placed at the level of the midurethra and not at the bladder neck? Based on subjective outcome measures that take into account the development of voiding dysfunction and de novo urge incontinence as well as quality-of-life questionnaires, this study shows that the TVT is effective in patients with varying degrees of ISD, patients with well-supported bladder necks as well as occult incontinence.
References
McGuire EJ, Lytton B, Pepe V et al (1976) Stress incontinence. Obstet Gynecol 47:255–264
Blaivas JG, Olsson CA (1988) Stress incontinence: classification and surgical approach. J Urol 139:727–731
Ulmsten U, Henriksson P, Johnson P et al (1996) An ambulatory surgical approach under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J 7:81–86
Nilsson CG, Kuuva N, Falconer C, et al (2001) Long-term results of the tension-free vaginal (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J 2(Suppl):S5–S8
Rezapour M, Falconer C, Ulmsten U (2001) Tension-free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD)—a long-term follow-up. Int Urogynecol J 2(Suppl):S12–S14
Mutone N, Brizendine E, Hale D (2003) Clinical outcome of tension-free vaginal tape procedure for stress urinary incontinence without preoperative urethral hypermobility. J Pelvic Med Surg 9:75–81
Karram MM (2003) Pathophysiology of genuine stress incontinence: what do we really know? Int Urogynecol J 14:77
Uebersax JS, Wyman JF, Shumaker SA et al (1995) Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Neurourol Urodyn 14:131–139
Ulmsten U, Johnson P, Rezapour M (1999) A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol 106:345–350
Kleeman S, Goldwasser S, Vassallo B et al (2002) Predicting voiding efficiency after surgery for incontinence and prolapse. Am J Obstet Gynecol 187(1):49–52
Grody MH (1998) Urinary incontinence and concomitant prolapse. Clin Obstet Gynecol 41:777–785
Bakas P, Liapis A, Creatsas G (2002) Q-tip test and tension-free vaginal tape in the management of female patients with genuine stress incontinence. Gynecol Obstet Invest 53:170–173
Klutke JJ, Carlin BI, Klutke CG (2000). The tension-free vaginal tape procedure: correction of stress incontinence with minimal alteration in proximal urethral mobility. Urology 55:512–514
Kayigil O, Ahmed S, Metin A (1999). The coexistence of intrinsic sphincter deficiency with type II stress incontinence. J Urol 162:1365–1366
Gordon D, Gold RS, Pauzner D et al (2001). Combined genitourinary prolapse repair and prophylactic tension-free vaginal tape in women with severe prolapse and occult stress urinary incontinence: preliminary results. Urology 58:547–549
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Segal, J.L., Vassallo, B.J., Kleeman, S.D. et al. The efficacy of the tension-free vaginal tape in the treatment of five subtypes of stress urinary incontinence. Int Urogynecol J 17, 120–124 (2006). https://doi.org/10.1007/s00192-005-1371-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-005-1371-9