Abstract
The aim of the study is to illustrate that the midurethral positioning of the tension-free vaginal tape (TVT) may not be necessary to achieve continence. Our secondary aim is to highlight that a fair number of successfully performed TVT procedures do not result in midurethral position of the tape. A review of 31 women who underwent TVT operations and consecutively returned for their follow-up visits from July 2003 to November 2003 was conducted. Their TVT procedures were performed between March 2000 and August 2003. Transperineal three-dimensional ultrasound was used to identify and obtain objective measurements of the position of the TVT tape relative to the urethra. Any patients with significant coexisting vault or uterovaginal prolapse were surgically corrected at the same time. Their stress urinary incontinence was objectively diagnosed by performing urodynamic studies (dual-channel subtraction cystometry, erect stress test) in the outpatient urogynaecology clinic. Postoperatively, patients were reviewed at 1 month and then at 6 months followed by annual reviews subsequently. All women were reassessed at the 6-month follow-up visit with a filling and voiding cystometry to detect recurrent genuine stress incontinence and detrusor instability. Any woman complaining of stress urinary incontinence after that was reassessed with urodynamic studies as mentioned above. The majority of women (67.7%, 21 women) had the TVT tape located in the middle one-third of the urethra; 9.7% (3 women) and 22.6% (7 women) of women had the TVT tape situated in the proximal and distal one-third of the urethra, respectively. Despite this, all 31 women remained continent at their postoperative follow-up visits. The midurethral position of the TVT tape may not be essential in restoring continence. The TVT tape once inserted may not always rest in the midurethral position as described.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The tension-free vaginal taping (TVT) device is a prolene nonabsorbable tape made by Gynaecare, (a division of Ethicon Inc and Johnson & Johnson, Sommerville, N.J., USA) and placed in a suburethral position via a minimally invasive procedure to prevent stress urinary incontinence based on a technique described by Ulmsten [1]. TVT operations have been reported to be an effective surgical treatment of genuine stress urinary incontinence (GSI) [2, 3]. Universally excellent outcomes have been reported with 85% cure rates in stress incontinent patients [4], 74% in stress incontinent patients with previous continence surgery [5] and 82% in intrinsic sphincter deficiency [6]. Comparable efficacy has been reported in a prospective randomized controlled trail comparing Burch colposuspension and TVT [7].
Petros et al. [8, 9] described the support of the midurethra at the insertion point of the posterior pubourethral ligaments. Based on this theory of achieving urinary continence, Ulmsten [1, 2, 10] developed the minimally invasive procedure of TVT that supports the midurethra. The midurethral insertion of the tape was thought to replace the supporting role of the pubourethral ligaments. This is claimed to be the key to restoring continence in TVT procedures. Other authors have also highlighted the importance of the tape being positioned in the midurethra without fixation or elevation of the urethra/bladder neck complex [11, 12] and not positioned near the bladder neck or at the proximal urethra.
Throughout our surgical experience, we have noticed that there is no definitive method of ensuring that the TVT tape is positioned in the midurethra intraoperatively. This combined with the very unique elastic properties of the TVT tape [13] (high elasticity and low stiffness) and the fact that the tape is inserted without fixation in the midurethra may lead to a tendency for the tape to migrate to the proximal [14] or distal third of the urethra rather than resting in the midurethra. A recent study of TVT in vivo using X-ray images demonstrated that the tape may have a tendency to rest in the proximal third of the urethra, rather than directly in the midurethra [15]. Bearing this in mind and the high continence rates achieved with TVT procedures [4, 5, 6, 7], we are of the opinion that the midurethral positioning of the tape may not be such a crucial factor in restoring continence.
Radiological techniques to visualize the lower urinary tract include voiding cystography, micturating cystography, lateral bead chain cystography, dynamic fluoroscopy, videocystourethrography and magnetic resonance imaging. Ultrasound scanning has been shown to be comparable with radiographic contrast medium methods in assessing the pelvic floor prior to and after continence surgery and is increasingly being used as an alternative imaging technique [16, 17]. Ultrasound as part of the diagnostic work-up of stress urinary incontinence and genitourinary prolapse allows for the morphological and dynamic assessment of the lower urinary tract [18]. Perineal ultrasound especially has given good visualization of the bladder, bladder base, urethrovesical junction and the symphysis pubis [19], so much so that postoperative ultrasound allows one to evaluate the outcome of surgery as well as voiding problems and morphological causes of recurrent urinary incontinence or of newly occurring urgency symptoms [18].
Three-dimensional ultrasound may improve the diagnostic outcome of sonography due to the reconstruction of the transverse plane [20]. According to a recently published review in 2003 [18], the use of three-dimensional ultrasound is currently restricted to volume calculation of the urethra [21] and pelvic floor muscle [22].
The primary aim of our study is to show that the midurethral position of the TVT tape may not be necessary to restore continence. Our secondary aim is to highlight that a fair number of correctly performed TVT procedures do not result in midurethral position of the tape
Material and methods
Transperineal three-dimensional ultrasound scans (Combison 530 manufactured by Kretztechnik, Zipf, Austria) were performed on 31 women who underwent TVT operations and consecutively returned for their follow-up visits from July 2003 to November 2003. Their TVT procedures had been performed between March 2000 and August 2003 in KK Hospital, Singapore The ultrasound scans were therefore not performed in the same interval after surgery for each patient. The inclusion criterion for the study was that all women had to have had their stress urinary incontinence treated surgically by the TVT procedure. Any patients with significant coexisting vault or uterovaginal prolapse were surgically corrected at the same time. Their stress urinary incontinence was objectively diagnosed by performing urodynamic studies (dual-channel subtraction cystometry, erect stress test) in the outpatient urogynaecology clinic. We used transperineal three-dimensional ultrasound scans to help in the identification and to obtain objective measurements of the position of the tape relative to the urethra as three-dimensional ultrasound is said to improve the visualization of lower genital tract structures [20] compared to conventional two-dimentional ultrasound.
The TVT procedure was performed with a sagittal incision 1.5 cm long made in the suburethral vaginal wall 1 cm from the external urethral meatus as described by Ulmsten [10]. After paraurethral tunneling, the tape was directed in a cephalad direction through the retropubic space. It was then led through suprapubic skin incisions created 2 cm lateral to the midline on each side. The tape therefore was located in a suburethral position and should be tension free without the need for fixing the tape with sutures. Cohesion of the tape with the surrounding tissues should hold it in place.
The surgery along with the pre- and postoperative assessments were performed by the same urogynaecologist so as to reduce interoperator errors in the study. Postoperatively, patients were reviewed at 1 month and then at 6 months followed by annual reviews subsequently. All women were reassessed at the 6-month follow-up visit with a filling and voiding cystometry to detect recurrent genuine stress incontinence and detrusor instability. Any woman complaining of stress urinary incontinence after that was reassessed with urodynamic studies as mentioned above. Surgery was considered a failure if the patient complained of stress urinary incontinence, had a positive erect stress test or when genuine stress incontinence was objectively diagnosed by urodynamic studies as mentioned earlier on subsequent follow-up visits.
The position of the tapes relative to the urethra as well as the urethral lengths were measured with the aid of transperineal three-dimensional ultrasound scans. The measurements were obtained with the women in the supine position without straining. These measurements were carefully traced by hand and three measurements of each parameter were taken and averaged out to obtain the final value. This was done to reduce the amount of intraobserver error in the measurements.
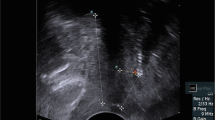
Figure 1a, b illustrates how our relevant measurements were taken and the appearance of the TVT tape on three-dimensional ultrasound scan. The urethral length (A) was obtained by measuring the outer curve of the urethra from the bladder neck to the urethral meatus. The midurethral length (B) was calculated by dividing the urethral length (A) in half. The position of the TVT tape (C) relative to the urethra was similarly obtained by measuring its distance from the bladder neck to its suburethral position by following the outer curve of the urethra. As the TVT tape is >1 cm wide and can affect its classification as being in the proximal, middle or distal one-third of the urethra, a standardized reference point or midpoint on the tape (C) was determined by adding the distance between the TVT tape’s proximal edge (C1) and distal edge (C2) from the bladder neck as mentioned above and dividing this by a factor of 2 (C=[C1+C2]/2). The distance that the TVT tape was located with respect to the midurethral (D) was calculated by subtracting the TVT tape position from the midurethral length (D=B−C) where a positive value and a negative value represented deviation towards and away from the bladder, respectively.
The women were divided into three groups depending on the location of the TVT along the entire urethral length (i.e. TVT tape in the proximal one-third, middle one-third and distal one-third). The intention was to see if there was any association between the position of the TVT tape and the development of GSI postoperatively.
Results
A summary of the characteristics of the patients who were included for our pilot study is shown in Table 1 and Table 2. All of the women had either GSI (93.5%) or occult stress urinary incontinence (SUI, 6.5%). One woman with GSI had concurrent detrusor instability (DI) while another woman with occult SUI had concurrent DI. The various concurrent operations performed in addition to TVT procedures are illustrated in Table 3.
None of the women developed postoperative GSI or reported any subjective SUI postoperatively according to the protocol highlighted above. None of the women developed de novo DI. The median time of follow-up was 14.5 months (range: 5.2–41.9 months).
The median urethral length was 4 cm (range: 2.9–5.0 cm). There were only two women (6.5%) in whom the TVT tape was found exactly at the midurethra. The majority of women (67.7%, 21 women) had the TVT tape located in the middle one-third of the urethra; 9.7% (3 women) and 22.6% (7 women) of women had the TVT tape situated in the proximal and distal one-third of the urethra, respectively.
There were altogether eight women (25.8%) who reported postoperative urgency symptoms. Of these women, three (9.7%) had reported symptoms of urgency before surgery. Further analysis revealed that the TVT tape was found to be in the middle one-third of the urethra in the majority of women with postoperative urgency symptoms (16.1%, five women in total). The TVT tape was located in the middle one-third of the urethra in four women while one woman had the TVT tape located in the distal one-third of the urethra as illustrated in Table 4. The number of women who developed de novo urgency without incontinence was comparable to other studies [23, 24]. There appeared to be no correlation between the occurrence of urgency and the location of the TVT tape along the urethra.
We were concerned that concurrent anterior repair surgery could have an effect on the location of the TVT tape. We therefore further subdivided the women into two groups: those who had concurrent anterior repair procedures and those who did not. In women who had concurrent anterior repair surgery, this was performed first before the TVT procedure and the TVT procedure was performed using a separate incision from the anterior repair procedure. Fifteen women had concurrent anterior repair surgery in addition to the TVT procedures. Of the 16 women who did not have anterior repair surgery, 14 had only TVT procedures performed, 1 had vaginal hysterectomy and another had posterior repair and vaginal hysterectomy in addition to the TVT procedure (Table 5, Table 6). Using Fisher’s exact test, there appears to be no correlation between undergoing anterior repair surgery and the tendency for the TVT tape to be located in a specific location along the urethra (p=0.25).
Discussion
The theory and method of tension-free vaginal taping was first described by Petros and Ulmsten in 1990 [8, 9]. This operative procedure has subsequently been further described in detail by other authors [1, 2, 10, 11, 12]. The emergence of TVT operations as one of the most commonly performed surgical treatments for stress urinary incontinence worldwide remains undisputed. More than 110,000 units have been sold for use in the United States alone with an additional 350,000 units used internationally so far, according to reports from the manufacturer in 2002 [14].
Traditionally, the main support of the urethra and urethrovesical (UV) junction is seen to come from the posterior pubourethral ligaments, extending from the inferior portion of the pubis and attaching to the midurethra. They prevent downward and posterior rotational displacement of the urethra. The hammock of the levator ani muscle, covered by endopelvic fascia, and the pelvic diaphragm support the bladder and urethra in their abdominal positions. The pubourethralis forms a ‘sling’ around the proximal urethra as it passes through the pelvic diaphragm and aids in preventing posterior displacement of the proximal urethra and bladder neck [25].
One theory of incontinence states that the loss of anatomic support, which allows downward and posterior rotational movement of the bladder neck and proximal urethra from their intra-abdominal positions, prevents the concomitant transmission of intra-abdominal pressure to the bladder and continence area and places the urethra in a dependent position with respect to the bladder base [25]. There is in addition a loss of the UV angle so that the base of the bladder and urethra are in line along with funneling of the UV junction. These anatomical changes were seen on cystourethrography in stress urinary incontinent patients more that 50 years ago [26].
The ‘integral theory of urinary continence’ as reported by Petros et al. [8, 9] describes the support of the midurethra at the insertion point of the posterior pubourethral ligaments. According to this theory, incontinence is caused by impaired collagen function causing disruption of the elements necessary to maintain anatomical structures involved in the urethral closure mechanism. These are the pubourethral ligaments, the vaginal insertion of the pubococcygeal muscles and the vaginal support of the urethra. Based on this theory, the TVT procedure was developed as minimally invasive continence surgery on the assumption that the midurethral fixation of the tape would be the decisive factor in restoring continence. The midurethral position of the tape would imitate the function of the pubourethral ligaments to restore normal anatomy and provide for midurethral ‘functional kinking’ [11]. Other authors have also emphasized the importance of midurethral placement of the TVT tape [1, 2, 10, 12].
The importance of the placement of the TVT tape in the midurethral position to achieve continence may not be as crucial based on the results from our pilot study. Despite the varied location of the TVT tape, the women were all continent postoperatively.
The ‘hammock hypothesis’ as described by DeLancey subscribes to the theory that the increase in urethral pressure during times of stress is thought to depend on adequate support of the proximal urethra. As long as the urethral pressure is greater than the intra-abdominal pressure, stress urinary incontinence is prevented and he emphasizes the role this ‘hammock’ contributes to urethral integrity [27]. Our results along with other authors [15, 27], in which some women were able to achieve continence with the TVT tape situated in the proximal one-third of the urethra or the bladder neck, add weight to our theory that the TVT tape does not necessarily need to be in the midurethral position. In these cases, the TVT tape may significantly stabilize the bladder neck [28] and reduce the hypermobility of the UV junction or bladder neck [29, 30] similar to the mechanism of Burch colposuspension and suburethral sling procedures. Lukacz et al. [14] found that the TVT sling provides support, albeit transient, to the proximal half of the urethra during straining.
De Lancey [31] found that the pubourethral ligaments have their insertion in the upper half of the urethra. Others [32] were able to isolate the pubourethral ligaments along the 20th to 60th percentile area of the urethra (where 0% represents the bladder neck and 100% is the external urethral meatus), i.e. the ligaments can extend beyond the midurethra. Recently, Rodriguez and Raz [33] recommended in their study that the placement of a polypropylene sling under the distal urethra is a new, simple, quick, inexpensive and effective method to correct stress urinary incontinence.
Conclusion
Although the number of women in our pilot study was small, and other concurrent surgeries were performed, our results suggest that the midurethral position of the TVT tape may not be necessary to achieve continence. We were also able to illustrate that a fair number of correctly performed TVT procedures do not result in midurethral position of the tape. The authors realize that we need to conduct a longer term study involving more women to support our theory convincingly.
References
Ulmsten UJ, Henrikson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J 7:81–86
Ulmsten UJ, Falconer C, Johnson P et al (1998) A multicenter study of tension-free vaginal tape for surgical treatment of stress urinary incontinence. Int Urogynecol J 9:210–213
Olsson I, Kroon U (1999) A three year postoperative evaluation of tension-free vaginal tape. Gynecol Obstet Invest 48:267–269
Nilsson JCG, Kuuva N, Falconer C, Rezapour M, Ulmsten U (2001) Long term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J 12 [Suppl 2]:S5-S8
Rezapour M, Ulmsten U (2001) Tension-free vaginal tape (TVT) in women with recurrent stress urinary incontinence. A long-term follow up. Int Urogynecol J 12 [Suppl 2]:S9-S11
Rezapour M, Falconer C, Ulmsten U (2001) Tension-free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD). A long-term follow up. Int Urogynecol J 12 [Suppl 2]:S12-S14
Ward K, Hilton P (2002) Prospective multicentre randomised trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. Br Med J 325:67
Petros PE, Ulmsten UJ (1993) An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl 153:1–93
Petros PE, Ulmsten UJ (1990) An integral theory of female urinary incontinence. Acta Obstet Gynecol Scand 69 [Suppl 153]:1–37
Ulmsten UJ, Johnson P, Rezaour M (1999) A three-year follow up of tension-free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol 106:345–350
Falconer C, Ekman-Ordeberg G, Malmstrom A, Ulmsten UJ (1996) Clinical outcome and changes in connective tissue metabolism after intravaginal slingplasty in stress incontinent women. Int Urogynecol J 7:133–137
Fischer A, Meghil S, Arnold B, Hoffmann G (2000) TVT—Implantation nach Ulmsten: Ersatz der defekten Pubourethralligamente als wirksame Maβnahme zur Behandlung der weiblichen Streβharninkontinez. Frauenarzt 41:61–70
Dietz HP, Vancaillie P, Svehla M, Walsh W, Steensma AB, Vancaillie TG (2001) Mechanical properties of implant materials used in incontinence surgery. Neurourol Urodyn 20:530
Lukacz ES, Luber KM, Nager CW (2003) The effects of the tension-free vaginal tape on proximal urethral position: a prospective, longitudinal evaluation. Int Urogynecol J 14:179–184
Kaum HJ, Wolff F (2002) TVT: on midurethral tape positioning and its influence on continence. Int Urogynecol J 13:110–115
Schaer G, Koelbl H, Voigt R et al (1996) Recommendations of the German Association of Urogynaecology on functional sonography of the lower female urinary tract. Int Urogynecol J 7:105–108
Dietz HP, Wilson PD (1998) Anatomical assessment of the bladder outlet and proximal urethra using ultrasound and videourethrocystography. Int Urogynecol J 9:365–369
Tunn R, Petri E (2003) Introital and transvaginal ultrasound as the main tool in the assessment of urogenital and pelvic floor dysfunction: an imaging panel and practical approach. Ultrasound Obstet Gynaecol 22:205–213
Virtanen HS, Kiiholma P (2002) Urogynecologic ultrasound is a useful aid in the assessment of female stress urinary incontinence—a prospective study with TVT procedure. Int Urogynecol J 13:218–223
Tunn R, Bergmann-Hensel U, Beyersdorff D, Heinrich G, Fischer W, Hamm B (2001) Diagnostik von Urethradivertikeln und Peri-urethralen Raumforderungen. Fortschr Rontgenstr 173:109–114
Toozs-Hobson P, Khullar V, Cardozo L (2001) Three-dimensional ultrasound: a novel technique for investigating the urethral sphincter in the third trimester of pregnancy. Ultrasound Obstet Gynecol 17:421–424
Wisser J, Schaer G, Kurmanavicius J, Huch R, Huch A (1999) Use of 3D ultrasound as a new approach to assess obstetrical trauma to the pelvic floor. Ultraschall Med 20:15–18
Sevestre S, Ciofu C, Deval B, Traxer O, Amarenco G, Haab F (2003) Results of the tension-free vaginal tape technique in the elderly. Eur Urol 44:128–131
Buxant F, Roumeguere T, Anaf V, Schulman C, Simon P (2001) A new approach in techniques to treat urinary incontinence: TVT (tension free vaginal tape). Rev Med Brux 22:166–169
Staskin DR, Zimmern PE, Hadley HR, Raz S (1985) The pathophysiology of stress incontinence. Symposium of female urology. Urol Clin North Am 12:271–277
Jeffcoate TNA, Roberts H (1952) Stress incontinence of urine. J Obstet Gynaecol Br Emp 59:685–707
DeLancey JOL (1994) Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis. Am J Obstet Gynecol 170:1713–1723
Atherton M, Stanton S (1999) How does the TVT produce continence? Neurourol Urodyn 18:370–371
Creighton SM, Clark A, Pearce JM, Stanton SL (1994) Perineal bladder neck ultrasound: appearances before and after continence surgery. Ultrasound Obstet Gynecol 4:428–433
Quinn MJ, Beynon J, Mortensen NN, Smith PJB (1989) Vaginal endosonography in the post-operative assessment of colposuspension. Br J Urol 63:295–300
De Lancey J (1986) Correlative study of paraurethral anatomy. Obstet Gynecol 68:91–97
Cruikshank S, Kovac R (1997) The functional anatomy of the urethra: role of the pubourethral ligaments. Am J Obstet Gynecol 176:1200–1205
Rodriguez LV, Raz S (2001) Polypropylene sling for the treatment of stress urinary incontinence. Urology 58:783–785
Baden WF, Walker T (1992) Surgical repair of vaginal defects. Lippincott, Philadelphia
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ng, C.C.M., Lee, L.C. & Han, W.H.C. Use of three-dimensional ultrasound scan to assess the clinical importance of midurethral placement of the tension-free vaginal tape (TVT) for treatment of incontinence. Int Urogynecol J 16, 220–225 (2005). https://doi.org/10.1007/s00192-004-1245-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-004-1245-6