Abstract
This study aimed to establish the prevalence and effect of urinary incontinence on quality of life during pregnancy and after parturition. A prospective cohort of primigravidae was recruited. The Kings Health Questionnaire (KHQ) was self-administered antenatally (34 weeks to term) and postnatally (3 months after delivery). Four hundred ninety-two primigravidae were recruited. The prevalence of urinary incontinence was reported as: pre-pregnancy 3.5% (17/492), antenatal 35.6% (175/492), 3–5 days postpartum 13.7% (51/370) and 3 months postnatal 13.0% (47/362). Most women with urinary incontinence experienced an impact on quality of life antenatally (54.3%) and postnatally (71.1%), although those experiencing an impact usually reported it as ‘a little’ (75.8 and 87.5%). There was a higher prevalence of urinary incontinence after forceps delivery (p<0.05) but not of greater impairment in quality of life (p>0.05). Personal and general health deteriorated postnatally (p<0.05). During pregnancy most women with urinary incontinence experience minimal impact on quality of life. Postnatally, other causes of morbidity may contribute to worsening of general and personal health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower urinary tract symptoms are common during pregnancy and following parturition and factors relating to childbearing are implicated in their development [1, 2, 3, 4, 5]. Urinary incontinence is more common in nulliparous women during pregnancy than in non-pregnant controls [6]. Although new mothers have reported that the physical and emotional consequences of childbearing are a cause for concern [7], the impact of urinary incontinence on general health and quality of life during the antenatal and postnatal periods is largely unstudied.
Assessment of quality of life in women with urinary incontinence has been facilitated by the development of several condition-specific questionnaires with the Kings Health Questionnaire (KHQ), one such instrument that has undergone psychometric tests for reliability, validity and responsiveness to change [8]. The application of quality of life instruments to women with antenatal and postnatal urinary incontinence enables an objective measurement of the impact of symptoms on lifestyle and assesses the severity of the condition at a time when symptoms are common and often arise for the first time.
The aims in undertaking this study were to use the KHQ to examine the effect of urinary incontinence on quality of life in primigravidae during pregnancy and after delivery and to determine whether the type of incontinence, intra-partum events, or co-existing lower urinary tract symptoms affect quality of life in women with urinary incontinence at these times.
Methods
Between August 2000 and June 2001, all primigravidae between 34 and 40 weeks attending antenatal clinics were invited to participate in this prospective study. Ethical approval for the study was obtained from the Research Ethical Committee, University of Ulster in Northern Ireland. All participants signed a consent form. A pilot study (n=50) was carried out to assess the study design. Pilot data was excluded from the final statistical analysis. A research assistant (S.H.) interviewed primigravidae at 34–40 weeks. At interview, women were invited to participate and they self-completed a structured urinary incontinence questionnaire, adapted from a previous study [9]. On the urinary incontinence questionnaire, women were asked if they had experienced any urinary incontinence within the last 3 months and indicated the frequency and circumstances of this symptom. The frequency was defined as ‘never’, ‘sometimes’ (≤1 time per month) or ‘often’ (≥2 times per month) and the circumstances were leakage of urine on coughing, laughing, exercise, lifting, climbing stairs, full bladder, walking, other occasions. They were also asked about the wearing of sanitary protection. Those who reported ‘any’ urinary incontinence within the previous 3 months self-completed the KHQ [8].
At 3–5 days postpartum, women were asked to self-complete the structured urinary incontinence questionnaire in which they were asked if they had experienced any urinary incontinence since delivery [9]. Intrapartum details were obtained from obstetric notes and delivery suite computerised records.
All women were contacted by post at 3 months after delivery. The structured urinary incontinence questionnaire was completed [9] and those with urinary incontinence within the previous 3 months self-completed the KHQ [8]. Non-respondents were sent a postal reminder and were contacted by telephone 4 weeks later. Non-respondents and respondents were compared with regard to age, mode of delivery and prevalence of antenatal or postpartum urinary incontinence.
Data was coded and transferred to the Statistical Package for Social Services (SPSS). Analysis was carried out using analysis of variance (ANOVA) and Kruskall-Wallis tests for parametric and non-parametric interval variables, respectively. The Wilcoxon ranks paired sums test was applied for paired non-parametric categorical data to determine any significant change in antenatal and postnatal domain scores on the KHQ. Logistic regression analysis was performed to determine any association between intrapartum events and urinary incontinence at 3–5 days postpartum and 3 months postnatal. All intrapartum variables (i.e. mode of delivery, length active second stage, length passive second stage, birth weight, episiotomy, pelvic floor exercises) were analysed using a univariate analysis (individual crosstabulation with merging of variables and χ2 p<0.05 taken as significance). Significant variables on univariate analysis were entered into the logistic regression model with urinary incontinence after delivery taken as the dependent variable.
Results
Four hundred ninety-two consecutive women at 34–40 weeks gestation were recruited from antenatal clinics. Mean age 26 (sd 5.26) years. Questionnaires were completed by 75.6% (372/492) women at between 3 and 5 days postpartum and 73.6% (362/492) returned postal questionnaires 3 months after delivery. Non-respondents at 3 months were compared with respondents at 3 months. Women who did not complete the 3-month questionnaire were younger than those completing the questionnaire (mean age 23.4 vs. 26.5 years, p<0.05), although this difference was not clinically significant. There was no significant difference in prevalence of antenatal or postpartum urinary incontinence or mode of delivery between the two groups (p>0.05). Antenatal pelvic floor exercises were performed by 298 (60.6%) women. Performance occurred daily in 156 (54.2%) women, weekly in 98 (34%) women and rarely in 34 (11.8%) women. The prevalence of urinary incontinence antenatally and at 3 months postnatally was not different in those who had performed antenatal pelvic floor exercises (χ2 p =0.33, χ2 p =0.23).
Prevalence of lower urinary tract symptoms
The prevalence of urinary incontinence was reported as follows: pre-pregnancy 3.5% (17/492), antenatal 35.6% (175/492), postpartum 13.7% (51/370) and 3 months postnatal 13.0% (47/362).
Table 1 indicates the prevalence of lower urinary tract symptoms as reported on the KHQ (i.e. for women with urinary incontinence) at 34–40 weeks and at 3 months postnatal. Twenty-two women did not complete the question on type of antenatal urinary incontinence and nine women did not complete the type of postnatal urinary incontinence. LUTs were defined as follows on the KHQ: frequency going to the toilet very often; nocturia getting up at night to pass urine; urgency strong and difficult control of desire to pass urine; urge incontinence urinary leakage associated with a strong desire to pass urine; stress incontinence urinary leakage with physical activity, e.g. coughing, sneezing, running; nocturnal eneuresis wetting the bed at night; and intercourse leakage urinary incontinence with sexual intercourse. Frequent water infections, bladder pain and difficulty passing urine were not defined on the KHQ.
Antenatally 57.3% (101/175) and 3 months postnatally 63.6% (28/44) of women wore pads.
Impact of urinary incontinence on quality of life
The impact of urinary incontinence on antenatal quality of life (QoL) was influenced by the type of urinary incontinence (stress, urge or mixed) and the number of co-existing urinary tract symptoms.
Table 2 illustrates the QoL domain scores on the KHQ for each type of antenatal urinary incontinence. Before delivery (34–40 weeks) primigravidae with mixed urinary incontinence or urge incontinence had QoL scores that were worse than those with stress alone in the physical, sleep and severity domains (Kruskall Wallis p<0.05). This difference was not observed 3 months after delivery (p>0.05). At 34 weeks, domain scores in women with urinary incontinence indicated deterioration in QoL (i.e. higher score) as the number of co-existing lower urinary tract symptoms increased, with the exception of the general and personal health domains (Kruskall-Wallis test p<0.05). This association was not demonstrated 3 months after delivery.
Antenatal and postnatal QoL on KHQ
Table 3 illustrates the QoL domain scores reported on the KHQ in women with antenatal and postnatal urinary incontinence. Although scores in all domains were low before and after delivery, higher scores were noted postpartum in the general health and personal health domains. This indicated that QoL was worse in women with postnatal urinary incontinence compared with those with antenatal incontinence (Wilcoxon paired ranks sums test p<0.05).
Tables 4 and 5 illustrate the descriptive responses on the ten questions in the general and personal health domains.
Table 6 illustrates the descriptive responses on the question asking the effect of bladder symptoms on life during the antenatal and postnatal time.
Intrapartum factors
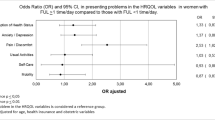
The role of intrapartum events on prevalence of urinary incontinence at 3–5 days postpartum and at 3 months postnatal was studied. At 3–5 days postnatal, prediction of group membership was 86% accurate after any variables were entered into the model and accuracy was 85% after mode of delivery was considered. Associations with urinary incontinence at 3–5 days after delivery were normal delivery (p=0.02), ventouse (p=0.04), forceps (p<0.001) and length of the active second stage (p=0.04) (logistic regression analysis r2=0.09). At 3 months postpartum, prediction of group membership was 86.9% accurate after any variables were entered into the model and accuracy remained at 86.9% after mode of delivery was considered. At 3 months after delivery, forceps was the only significant intrapartum even (p<0.01) (logistic regression analysis r2=0.071). At 3 months, QoL scores on the KHQ were not associated with mode of delivery (p>0.05).
Discussion
In this prospective study we found that 36% of primigravidae reported urinary incontinence during the final trimester and this was most commonly mixed urinary incontinence. For many women urinary incontinence had resolved 3 months after delivery. Comparison with other studies is limited to those reporting prevalence of any urinary incontinence in primigravidae during late pregnancy and at 3 months postnatal [2]. We report an antenatal prevalence that is lower and a postnatal prevalence similar to that previously reported at 3 months [2]. Almost all women with antenatal urinary incontinence also reported frequency and nocturia, with most reporting urgency. Other studies have reported these lower urinary tract symptoms to be very common in pregnancy [1, 5] and this is likely to reflect physiological changes in bladder pressure and volume parameters [10]. We did not assess serial prevalence during pregnancy and we did not report on prevalence of lower urinary tract symptoms in women who were continent, which may differ from the prevalence reported in this study. Recall bias may have been introduced in reporting the pre-pregnancy prevalence and in difficulty differentiating lochia from urinary loss at 3–5 days postpartum.
We assessed the impact of urinary incontinence on quality of life during pregnancy and at 3 months postpartum. Postnatally, there were more women who experienced an impact on their lives compared with antenatally. However, this impact was most commonly reported as ‘a little’ with few reporting ‘at least a moderate’ effect on quality of life. The presence of other lower urinary tract symptoms and the type of incontinence are two factors that might have influenced the impact on quality of life. We found that there was a greater impact on quality of life in women who had other lower urinary tract symptoms and in those with antenatal mixed or urge urinary incontinence compared with those who had stress alone. This might suggest greater impairment in quality of life in primigravidae with detrusor overactivity, although without cystometric diagnosis this is purely speculation. However, women with detrusor overactivity experience greater impairment in quality of life, measured on the KHQ, compared to women with urodynamic stress incontinence [8]. An association between symptom type and impairment was not demonstrated postnatally and this may reflect that almost half of the women with postnatal urinary incontinence did not define the type of incontinence on the KHQ.
We examined the effect of urinary incontinence on antenatal and postnatal activities of daily living. Domain scores were low, suggesting minimal restriction in lifestyle for the specific roles explored on the questionnaire. When we compared antenatal and postnatal activities, only personal health was worse after delivery. Symptom severity scores did not indicate an increase in the severity of incontinence. Given that the total number of women that experienced an effect in the personal health domain was small, the clinical significance of this result is uncertain. However, there was a trend towards poorer general health postnatally and several causes for postnatal morbidity have previously been identified [11]. The responses in the personal health domain on the KHQ relate to relationships and sexual function and responses may have been affected by other morbidity such as perineal pain and postnatal depression. Certainly perineal pain is known to be common after vaginal delivery, with almost 21% of women reporting perineal pain 6–7 months after a normal vaginal delivery [12] and depression has been reported in 17% of women on the Edinburgh Postnatal Depression Scale [13]. Women may have reported how they viewed their quality of life in the personal health domain rather than how it was affected by urinary incontinence. This suggests the need to use a general health questionnaire in parallel with a condition-specific questionnaire.
Using logistic regression analysis, forceps delivery was found to be the only significant risk factor for urinary incontinence 3 months postnatally, although even this was of low predictive value. Few prospective studies examining pelvic floor dysfunction in primigravidae after delivery have applied a multivariate or logistic regression analysis to control for the impact of confounding variables [2, 14]. In Farrell’s study of 595 primiparae, he found that there was an increased risk of stress incontinence (RR 1.5) 6 months after a forceps delivery but this was non-significant when regression analysis was applied [14]. Chaliha reported on 549 primiparous women 3 months after delivery and found that caesarean section was associated with a lower incidence of faecal urgency, although not with stress incontinence [2]. Although we found that 3 months after a forceps delivery there was a higher prevalence of stress incontinence, forceps were not associated with more severe incontinence or a greater effect on activities of daily living where severity was measured on the KHQ and not by quantifying urine loss.
Conclusions
This study suggests that although many women report urinary incontinence during pregnancy, for most women symptoms are mild and do not impair quality of life.
The role of parity on severity of symptoms during pregnancy and after parturition was not assessed. However, we have established a reference point from which to study the effect of higher parity on quality of life at these times.
We have shown that although urinary incontinence usually resolves after delivery, women with urinary incontinence experience deterioration in general and personal health postnatally. This may reflect a lifestyle change after the birth of a first child or other causes for postnatal morbidity in addition to urinary incontinence. Our results suggest that even when a condition-specific questionnaire for urinary incontinence is administered, other unrelated morbidity may influence the questionnaire responses.
References
Cardozo L, Cutner A (1997) Lower urinary tract symptoms in pregnancy. Br J Urol 80[Suppl 1]: 14–23
Chaliha C, Veena K, Stanton SL, Monga A, Sultan AH (1999) Antenatal prediction of postpartum urinary and faecal incontinence. Obstet Gynecol 94:689–693
Nel JT, Dierdericks A, Joubert G, Arndt K (2001) A prospective clinical and urodynamic study of bladder function during and after pregnancy. Int Urogynecol J 12:21–26
Viktrup L, Lose G, Rolff M, Barfoed K (1992) The symptom of stress incontinence caused by pregnancy or delivery in primiparas. Obstet Gynecol 79:945–949
Viktrup L, Lose G, Rolff M, Barfoed K (1993) The frequency of urological symptoms during pregnancy and delivery in primpiparae. Int Urogynecol J 4:27–30
Wijma J, Potters AEW, de Wolf BTHM, Tinga DJ, Aarnoudse JG (2001) Anatomical and functional changes in the lower urinary tract during pregnancy. Br J Obstet Gynaecol 108:726–732
Kline C, Martin D, Deyo R (1998) Health consequences of pregnancy and childbirth as perceived by women and clinicians. Obstet Gynecol 92:842–848
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S (1997) A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol 104:1374–1379
Dolan LM, Casson K, McDonald P, Ashe RG (1999) Urinary incontinence in Northern Ireland—a prevalence study. BJU 89:760–766
Chaliha C, Bland JM, Monga A, Stanton SL, Sultan AH (2000) Pregnancy and delivery: a urodynamic viewpoint. Br J Obstet Gynecol 107:1354–1359
Glazener CMA, Abdalla M, Stroud P, Naji S, Templeton A, Russell I (1995) Postnatal maternal morbidity: extent, causes, prevention and treatment. Br J Obstet Gynaecol 102:282–287
Sleep J, Grant A, Garcia, et al (1984) West Berkshire perineal management trial. BMJ 289:587–590
Brown S, Lumley J (1998) Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol 105:156–161
Farrell SC, Allen VA, Baskett FT (2001) Parturition and urinary incontinence in primiparas. Obstet Gynecol 97:350–356
Acknowledgements
The authors wish to express their gratitude to Mr. Paul Fogarty, Consultant Obstetrician and Gynaecologist, Ulster Hospital, Dundonald, for allowing his patients to be recruited into this study and to the Northern Ireland Mother and Baby Association (NIMBA) for their financial sponsorship of S.H. We also wish to thank all of the women who participated.
Author information
Authors and Affiliations
Corresponding author
Additional information
Editorial Comment: This is a prospective cohort study that establishes the prevalence and effect of urinary incontinence on quality of life during pregnancy and after parturition in primigravid women. It covers new ground in its assessment of the effect on quality of life of urinary incontinence in this group of previously undescribed women. This research lays the foundation for further research into the combined effect of urinary incontinence and other co morbidities on the quality of life of pregnant women and recent parturients
Rights and permissions
About this article
Cite this article
Dolan, L.M., Walsh, D., Hamilton, S. et al. A study of quality of life in primigravidae with urinary incontinence. Int Urogynecol J 15, 160–164 (2004). https://doi.org/10.1007/s00192-004-1128-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-004-1128-x