Abstract
The aim of this study was to determine the short-term prevalence of de novo urinary symptoms after hysterectomy indicated by meno/metrorrhagia or dysmenorrhea/dyspareunia. The study group consisted of 451 women who had had a hysterectomy for reasons of meno/metrorrhagia or dysmenorrhea/dyspareunia. Fifty-three (12%) had a supracervical, 151 (33%) a total abdominal and 247 (55%) a vaginal hysterectomy. As a non-gynecologic background population we enrolled 110 women who had had their gallbladder removed laparoscopically. All women received a postal questionnaire 9–45 months after their operation. Specific questions were asked about their voiding habits, comprising significant stress incontinence, bothersome stress incontinence, significant urge incontinence, bothersome urge incontinence, pollakisuria, nocturia, use of pads, and the feeling of having a hygiene problem. To evaluate de novo symptoms or de novo cure, the women assessed the symptoms before as well as after the operation. Results showed that abdominal hysterectomy lasted longer, had heavier blood loss and required longer hospitalization than did vaginal or supracervical hysterectomy. Women scheduled for a supracervical hysterectomy had preoperatively more significant and bothersome urge incontinence, and postoperatively more significant urge, urgency, and feeling of having a hygienic problem than did women having a vaginal hysterectomy, a total abdominal hysterectomy or a laparoscopic cholecystectomy. When assessing de novo symptoms, supracervical hysterectomy was associated with more urgency and the feeling of having a hygienic problem. Some women experienced de novo cure, but these were almost exclusively in the study group and rarely in the control group. It was concluded that supracervical hysterectomy is related to more urinary symptoms than vaginal or total abdominal hysterectomy. De novo symptoms as well as de novo cure are common, which is why urinary symptoms after hysterectomy must be evaluated over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hysterectomy is a common operation in Denmark [1]. Most operations are performed for benign indications such as leiomyomata, meno/metrorrhagia, genital descensus or pelvic pain. Several studies have focused on the association between hysterectomy and urinary symptoms [2, 3, 4, 5]. It is not clear whether there is a direct pathophysiologic connection between hysterectomy and incontinence, or whether the association is based on a common factor. Furthermore, many women who undergo a hysterectomy also have an operation for uterovaginal prolapse or urinary incontinence, which may influence their continence status.
For urinary incontinence, a distinction is made between different symptoms of leakage. Stress incontinence is defined as urinary leakage associated with an increase in abdominal pressure [3]. Urge incontinence is caused by involuntary detrusor contractions [3]. The different etiologies may indicate different risk factors.
The main purpose of this study was to assess the short-term prevalence of de novo urinary symptoms after a hysterectomy performed for meno/metrorrhagia or dysmenorrhea/dyspareunia, and to compare the prevalence after different modes of hysterectomy.
Study design
The study group consisted of women who had had a hysterectomy at the Departments of Gynecology at Herning, Holstebro or Silkeborg Central Hospitals, Denmark, during the period 1 January 1998 to 31 December 2000. Data on all hysterectomies performed at these departments are collected in a regional database. The database contains information on indications for the hysterectomy, previous gynecologic surgery, BMI, mode of hysterectomy, additional surgery, duration of surgery, blood loss, uterine weight, and length of postoperative stay. From this database a study group was selected according to the following criteria: born after 31 December 1939, operation indicated for meno/metrorrhagia or dysmenorrhea/dyspareunia, previous vaginal delivery and no cesarean section, no previous surgery for vaginal descensus or urinary incontinence, no additional surgery for vaginal descensus or urinary incontinence, and uterine weight <400 g. All women included were Caucasian.
As a background population of women undergoing non-gynecologic surgery we selected all female patients born between1940 and 1965 who had had a laparoscopic cholecystectomy at Holstebro Central Hospital, Denmark, between 1 January 1999 and 31 December 2000. Nulliparae were excluded from the background population.
A postal questionnaire with an accompanying letter explaining the purpose of the study was sent 9–45 months postoperatively to all participants, including the background group. Specific questions were asked about pre- and postoperative voiding habits. The questions comprised stress incontinence, urge incontinence, bothersome stress or urge incontinence, significant incontinence, pollakisuria, nocturia and de novo symptoms or de novo cure. Stress incontinence was defined as involuntary leakage of urine during effort, and urge incontinence was defined as a leakage with a sense of urgency. Significant incontinence was defined as involuntary leakage of urine at least once a week. Bothersome incontinence was defined as significant incontinence and use of devices, decreased social ability, or having a hygienic problem with the incontinence. The questionnaires had previously been validated [6, 7].
If a woman did not return the questionnaire within 3 weeks she was sent a reminder once.
Statistical evaluation was performed by χ2-test, with Yates’ correction for discontinuity or, when appropriate, Fisher’s exact test. Patient characteristics and outcome were tested by analysis of variance (ANOVA) and Neumann-Keuls’ post hoc test. Level of significance was chosen as 5%.
Results
A total of 549 women in the study group and 144 women in the background group received the questionnaire. Questionnaires were returned by 451 (82%) and 110 (76%) women, respectively.
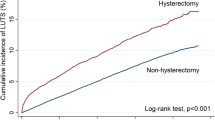
Fifty-three women in the study group had had a supracervical hysterectomy (12%), 151 a total abdominal hysterectomy (33%), and 247 a vaginal hysterectomy (55%). Patient characteristics (Table 1) show that women who had a supracervical hysterectomy were heavier than those otherwise operated on. The operation lasted significantly longer if the woman had a total abdominal hysterectomy. Blood loss and duration of postoperative hospitalization also differed significantly. Tables 2 and 3 show the prevalence of pre- and postoperative urinary symptoms, respectively. Significantly more women had urge incontinence, urgency or bothersome urge before or after supracervical hysterectomy than the other investigated women. Tables 4 and 5 show the prevalence of de novo symptoms or de novo cure after hysterectomy. The use of devices or the feeling of having a hygienic problem were more often experienced as a new problem among women who had had a supracervical hysterectomy rather than a total abdominal hysterectomy. A substantial number of women were cured after their operation, mainly in the hysterectomy group.
We performed a stepwise manual analysis with each incontinence type, bothersome incontinence and urgency separately as dependent variables, and the continuous variables of age, BMI, duration of surgery, preoperative hemoglobin, uterine weight, blood loss and postoperative stay as independent variables. We found that BMI was associated with de novo significant urge incontinence and de novo urgency (r= 0.18 and r= 0.15, both p<0.01), i.e. BMI accounted for 1%–2 % of the variance in these variables. However, BMI was associated with the reported stress incontinence before and after hysterectomy (r= 0.20 and r=0.21, respectively, both p<0.01), and similarly, for the reported urge incontinence before and after hysterectomy (r=0. 17 and r= 0.20, respectively, both p<0. 01). No single factor was found to be associated with de novo urgency in the supracervical hysterectomy group. BMI was found to be marginally associated with de novo urge incontinence (r=0. 28, p<0. 06). The results are interpreted to mean that owing to the association of BMI with incontinence in itself, the de novo symptoms tend to be so as well, irrespective of operation type. The findings are adjusted for the effects of weight/BMI.
Discussion
The main objectives of this study were to assess the effect of hysterectomy on urinary incontinence and to compare different modes of hysterectomy in this respect.
The bladder and urethra are closely related to the uterus. It has been assumed that total abdominal hysterectomy in particular may contribute to urinary incontinence because of damage to the pelvic floor innervation and to pelvic fibromuscular structures [8]. The newer literature, however, conflicts on the prevalence of urinary sequelae after hysterectomy. In a comprehensive review Brown et al. found that hysterectomy significantly increases the prevalence of later urinary incontinence, and the authors argue that all patients should be informed of this risk before accepting a hysterectomy [4]. In accordance with this, Van der Vart et al. found an increased risk of urge incontinence, especially bothersome urge incontinence [3]. In vitro studies based on urodynamics have shown a correlation between hysterectomy and incontinence [9, 10]. On the other hand, Kjerulff et al. and Bhattacharya et al. also concluded that women who had undergone a hysterectomy for non-malignant indications experienced improved urinary incontinence during the first 2 years after surgery [11, 12]. Thaker et al., in a prospective, randomized study from 2002, concluded that neither total nor subtotal hysterectomy adversely affects pelvic organ function at 12 months [13].
Others have shown that there is no persistently negative effect from non-radical hysterectomy on the function of the lower urinary tract [14].
Only a few other studies have made a distinction between total abdominal, supracervical and vaginal hysterectomy when investigating de novo urinary symptoms. According to Kilku et al., supracervical hysterectomy gave better results than total abdominal hysterectomy with respect to urinary incontinence [15]. In another study, total abdominal hysterectomy influenced bladder storage function less than did vaginal hysterectomy [16]. From a theoretical point of view, dissection of the bladder from the cervix may damage detrusor innervation, which is why supracervical hysterectomy should protect these structures [4].
All clinical studies of hysterectomy and urinary incontinence, including the present one, have some inherent selection bias, as women scheduled for total abdominal, supracervical or vaginal hysterectomy differ significantly in patient characteristics [4]. For example, obese women tend to undergo a supracervical or vaginal hysterectomy and not a total abdominal hysterectomy. Some differences in patient characteristics between the hysterectomy groups are also risk factors for urinary incontinence, such as obesity, nulliparity and cesarean delivery [17, 18, 19, 20, 21]. A simple comparison between the prevalence of postoperative urinary incontinence in different hysterectomy groups is therefore not possible, unless the preoperative prevalence of urinary incontinence is known.
In the present study, surprisingly, we found a significantly increased preoperative prevalence of bothersome urge as well as bothersome stress incontinence in women who had had a supracervical hysterectomy compared to women who had had a total abdominal or vaginal hysterectomy. This may be partly explained by the different patient characteristics in spite of markedly restricted selection to the study group, but our study design did not allow us to investigate this. Postoperatively, supracervical hysterectomy continued to be associated with an increased prevalence of some urinary symptoms, especially urge incontinence. When investigating de novo symptoms, women who had a supracervical hysterectomy still had an increased prevalence of urgency and use of devices, and they claimed significantly more often that they felt their new urinary symptoms to be a hygienic problem.
Furthermore, we showed some prevalence of de novo cure of urinary symptoms after any kind of hysterectomy. Whether this is based on surgery or reflects an inconstancy of urinary symptoms over time is unknown. However, hysterectomized women tended to experience de novo cure more often than did cholecystectomized women. This supports the view that hysterectomy in some women reduces their incontinence on a short-term basis. As women with a uterine weight exceeding 400 g were excluded from our study, de novo cure is hardly likely to be caused by simple pressure reduction.
A retrospective investigation of urinary symptoms may include significant recall bias [22]. As we primarily investigated a difference in symptoms, the relevance of this recall bias is minimized. We furthermore introduced a background population of cholecystectomized women to control for a possible difference in recall bias between gynecologic and non-gynecologic patients. No difference in recall bias was shown. To minimize bias based on selection our study group was heavily selected on patient characteristics known to influence continence status. On this background we regard our data as valid.
In conclusion, we found a significantly higher prevalence of preoperative as well as de novo urinary symptoms in women who had had a supracervical hysterectomy than in women who had had a total abdominal or vaginal hysterectomy. The prevalence of urinary symptoms after hysterectomy must be evaluated over time, as de novo symptoms and de novo cure are common.
References
Mouridsen L, Jørgensen P (1983) Urological problems and hysterectomy (in Danish). Ugeskr Laeger 145/14:1062–1064
Roovers JPWR, Van der Bom JG, Van der Vart CH, Fousert DMM, Heintz PM (2001) Does mode of hysterectomy influence micturition and defecation? Acta Obstet Gynecol Scand 80:945–951
Van er Vart CH, Van der Bom JG, De Leeuw JRJ, Roovers JPWR, Heintz APM (2002) The contribution of hysterectomy to the occurrence of urge and stress urinary incontinence symptoms. Br J Obstet Gynaecol 109:149–154
Brown J, Sawaya G, Thom DH, Grady D (2000) Hysterectomy and urinary incontinence: a systematic review. Lancet 356:535–539
Milsom I, Ekelund P, Molander U, Arvidson L, Areskoug B (1993) The influence of age, parity, oral contraception, hysterectomy and menopause on the prevalence of urinary incontinence in women. J Urol 149:1459–1462
Rasmussen KL, Hansen V, Madzak F, Ljungström B, Lauszus FF (2001) Feeling of illness after hysterectomy. Women’s own assessment (in Danish). Ugeskr Laeger 163:7040–7042
Knudsen HJ, Rosgaard A, Rasmussen KL (2001) Vaginal hysterectomy in non-prolapsed uterus (in Danish). Ugeskr Laeger 163:2133–2135
Smith PH, Ballantyne B (1968) The neuroanatomical basis for denervation of the urinary bladder following major pelvis surgery. Br J Surg 55:929–932
Morgan JL, O’Connell HE, McGuire EJ (2000) Is intrinsic sphincter deficiency a complication of simple hysterectomy? J Urol 164:767–769
Demirci F, Ozden S, Alpay Z, Demirci ET (1999) The effect of abdominal hysterectomy on bladder neck and urinary incontinence. Aust NZ J Obstet Gynaecol 39:239–242
Kjerulff KH, Langenberg PW, Greenaway L, Uman J, Harvey L (2002) Urinary incontinence and hysterectomy in a large prospective cohort study in American women. J Urol 167:2088–2092
Bhattacharya S, Mollison J, Pinion S et al. (1996) A comparison of bladder and ovarian function two years following hysterectomy or endometrial ablation. Br J Obstet Gynaecol 103:898–903
Thaker R, Ayers S, Clarkson P, Stanton P, Manyonda I (2002) Outcomes after total versus subtotal abdominal hysterectomy. N Engl J Med 347:1318–1325
Vierhout ME (2001) Influence of nonradical hysterectomy on the function of the lower urinary tract. Obstet Gynecol Surv 56:381–385
Kilkku P (1985) Supravaginal uterine amputation versus hysterectomy with reference to subjective bladder symptoms and incontinence. Acta Obstet Scand 64:375–379
Vervest HAM, Van Venrooij GEPM, Barents JW, Haspels AA, Debruyne FMJ (1989) Non-radical hysterectomy and the function of the lower urinary tract. Acta Obstet Gynecol Scand 68:221–229
Thom D, Brown JS (1998) Reproductive and hormonal risk factors for urinary incontinence in later life: A review of the clinical and epidemiologic literature. J Am Geriatr Soc 46:1411–1417
Brown J, Seeley DG, Fong J, Black DM, Ensrud KE, Grady D (1996) Urinary incontinence in older women: who is at risk? Obstet Gynecol 87:715–721
Samuelsson E, Victor A, Svärdsudd K (2000) Determinants of urinary incontinence in a population of young and middle-aged women. Acta Obstet Gynecol Scand 79:208–215
Thom DH, Van den Eeden SK, Brown JS (1997) Evaluation of parturition and other reproductive variable as risk factors for urinary incontinence in later life. Obstet Gynecol 90:983–989
Kjerulff KH, Langenberg PW, Rhodes JC, Harvey LA, Guzinski GM, Stolley PD (2000) Effectiveness of hysterectomy. Obstet Gynecol 95:319–326
Alling Møller L, Lose G, Jørgensen T (2000) Risk factors for lower urinary tract symptoms in women 40–60 years of age. Obstet Gynecol 96:446–451
Author information
Authors and Affiliations
Corresponding author
Additional information
Editorial Comment: This paper provides the readership with some interesting descriptive data regarding urinary symptoms after various forms of hysterectomy. One must be careful in the interpretation of these data, given that most of them were collected based on the subject’s memory of symptoms they had both before their surgery and as late as 3.5 years after their surgery. Furthermore, it is clear that the supravaginal group was a different subgroup of patients prior to surgery, in that they were heavier and had a higher baseline level of overactive bladder symptoms. What is clear is that urinary symptoms may vary after hysterectomy. From these data we can infer that symptoms can both improve and worsen. No mention is made of oophorectomy or the menopausal state of these women before and after surgery, and I wonder what effect this may have on their bladder symptoms. Further research into this interesting question is certainly warranted.
Appendix
Appendix
Questionnaire
Regarding involuntary urination and removal of the uterus
The questionnaire consists of two parts: The first part reflects on how you are feeling today whereas the second part reflects on how you felt prior to the removal of the uterus.
The questionnaire is to be answered by marking the statement which best describes your situation.
Part one
First part of the questionnaire reflects on involuntary urination today
-
1.
Do you experience involuntary urination when coughing, sneezing or lifting a heavy weight without having felt an urge to urinate?
-
No, never
-
Yes, less than once a week
-
Yes, approximately once a week
-
Yes, several times a week
-
Yes, daily
-
-
2.
Do you experience involuntary urination when having felt an urge to urinate you have been unable to control it until you reach the toilet?
-
No, never
-
Yes, less than once a week
-
Yes, approximately once a week
-
Yes, several times a week
-
Yes, daily
-
-
3.
When experiencing an urge to urinate are you able to control it until you reach the toilet?
-
No, never
-
Yes, less than once a week
-
Yes, approximately once a week
-
Yes, several times a week
-
Yes, daily
-
-
4.
How often do you urinate during 24 hours a day?
-
6 times max
-
6–10 times
-
More than10 times
-
-
5.
Do you get up during the night to urinate?
-
No
-
Yes, once or twice
-
Yes, three times or more
-
-
6.
Do you use any devices due to the involuntary urination?
-
No
-
Yes, panty shields (No. each 24 hours :__)
-
Yes, diapers (No. each 24 hours :__)
-
Yes, other devices (what other devices? __________________________________)
-
-
7.
If you are experiencing involuntary urination do you consider it to be a hygienic problem?
-
No
-
Yes, but a minor problem
-
Yes, a major problem
-
-
8.
If you are experiencing involuntary urination does it prevent you from engaging in activities you would otherwise take part in (i.e. exercising or riding the bus)?
-
Yes
-
No
-
Part Two
Second part of the questionnaire reflects on the involuntary urination prior to removal of your uterus.
-
1.
Prior to the hysterectomy did you experience involuntary urination when coughing, sneezing, lifting a heavy weight without having felt an urge to urinate?
-
No, never
-
Yes, less than once a week
-
Yes, approximately once a week
-
Yes, several times a week
-
Yes, daily
-
-
2.
Prior to the hysterectomy, did you experience involuntary urination when having felt an urge to urinate you were unable to control it until you reached the toilet?
-
No, never
-
Yes, less than once a week
-
Yes, approximately once a week
-
Yes, several times a week
-
Yes, daily
-
-
3.
Prior to the hysterectomy did you experience an urge to urinate which you were able to control until you reached the toilet?
-
No, never
-
Yes, less than once a week
-
Yes, approximately once a week
-
Yes, several times a week
-
Yes, daily
-
-
4.
Prior to the hysterectomy how often did you urinate during 24 hours a day?
-
6 times max
-
6–10 times
-
More than 10 times
-
-
5.
Prior to the hysterectomy how often did you get up during the night to urinate?
-
Never
-
Once or twice
-
Three times or more
-
-
6.
Prior to the hysterectomy did you use any devices due to the involuntary urination?
-
No
-
Yes, panty shields (No. each 24 hours :__)
-
Yes, diapers (No. each 24 hours :__)
-
Yes, other devices (what other devices? __________________________________)
-
-
7.
Prior to the hysterectomy did you regard the involuntary urination as a hygienic problem?
-
No
-
Yes but a minor problem
-
Yes a major problem
-
-
8.
If you were experiencing involuntary urination did it prior to the hysterectomy prevent you from engaging in activities you would otherwise take part in (i.e. exercising or riding the bus)?
-
Yes
-
No
-
Rights and permissions
About this article
Cite this article
Neumann, G., Olesen, P.G., Hansen, V. et al. The short-term prevalence of de novo urinary symptoms after different modes of hysterectomy. Int Urogynecol J 15, 14–19 (2004). https://doi.org/10.1007/s00192-003-1105-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-003-1105-9