Abstract
Purpose
The purpose of this study was to compare the functional outcomes, activity levels, mortalities, implant survival rates, and complications of total knee arthroplasty (TKA) in patients with rheumatoid arthritis (RA) with those in patients with osteoarthritis (OA) over a minimum 10-year follow-up period.
Methods
Between January 2007 and December 2009, 90 TKAs performed in 57 patients with RA (RA group) were retrospectively reviewed and matched with a control group of 180 TKAs performed in 114 patients with OA. The functional outcomes (Knee Society Score), activity levels (Koval grade), mortalities, implant survival rates, and complications were compared between the two groups with a minimum 10-year follow-up period. The mean follow-up periods were 12.3 years in the RA group and 12.6 years in the OA group.
Results
The mean Knee Society knee scores in the RA and OA groups improved from 37.7 ± 5.4 to 38.2 ± 5.3 preoperatively to 72.9 ± 22.8 to 83.1 ± 11.0 points, respectively, at the final follow-up (p < 0.05). At the final follow-up, 38 of 48 (79.2%) in the RA group and 105 of 109 (96.3%) in the OA group (p < 0.05) were outdoor ambulatory patients. The cumulative mortality rates in the RA and OA groups were 15.8% (9/57) and 4.4% (5/114) (p < 0.05) at the final follow-up, respectively. Kaplan–Meier survivorship analysis with revision of either component as an endpoint in the RA and OA groups estimated 94.4% and 98.3% chance of survival for 10 years, respectively.
Conclusion
TKA in patients with RA had worse functional outcomes and higher mortality over a minimum 10-year follow-up period, compared with TKA in patients with OA.
Level of evidence
IV
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is the most common form of chronic inflammatory joint disease that can destroy cartilage and erode joints, leading to significant pain and functional disability [1]. Its prevalence varies significantly among different populations, ranging from 0.2 to 1.0% [2, 3]. Nearly 28.5 new patients per 100,000 individuals are diagnosed each year in Korea [4].
Current RA medical therapy has markedly improved the function and quality of life in many patients, while they can still face progressive musculoskeletal comorbidity, such as irreversible knee joint destruction. With the increased ages of RA patients, there might be an increase in the number and complications of total knee arthroplasties (TKAs) performed in RA patients.
RA of the knee is different from osteoarthritis (OA) in pathogenesis, prognosis, and medical treatment, resulting in variable expected outcomes after TKA. End-stage knee damage from RA is not a localized problem and is only one component of a systemic disease. These differences affect TKA outcomes [5]. It is reasonable to expect that, as RA progresses, most patients undergoing TKA will experience other joint physical disabilities and complications. Although several studies have reported on TKA results in RA patients, limited data are available on the long-term follow-up outcomes of TKA in patients with RA compared to those with OA [6, 7].
Therefore, the aim of this retrospective case–control study was to compare the functional outcomes, activity levels, mortalities, implant survival rates, and complications of TKA in patients with RA with those in patients with OA over a minimum 10-year follow-up period. Our hypothesis was that TKAs in patients with RA would have poorer clinical outcomes and higher risk of mortality and revision surgery compared to those in patients with OA.
Materials and methods
The design and protocol of this retrospective study were approved by the Institutional Review Board of our hospital, which waived the requirement for informed consent. Between January 2007 and December 2009, a consecutive series of 98 primary TKAs was performed for 63 patients with confirmed diagnoses of RA at our hospital. Of these 63 patients, 6 (8 knees) were excluded from the study due to follow-up loss. The final cohort consisted of 51 females (79 knees) and 6 males (11 knees) (RA group). A total of 33 patients (57.9%) underwent staged bilateral procedures every week. The RA group was matched with a control group at a one-to-two ratio using the propensity score method. The control group was created according to the following matching criteria: sex, age, body mass index, and diagnosis of OA. One-hundred fourteen sex-, age-, body mass index-, and diagnosis-matched patients with OA who had undergone primary TKA between January 2008 and December 2008 (3172 TKAs) at our hospital were used as the control group. In total, 180 TKAs were included in 114 patients (12 men and 102 women) (OA group). Demographic data of sex, age, initial diagnosis, body mass index, pre-operative status as Koval category (activity levels) [8], and pre-operative Knee Society Score (clinical evaluations) [9] were obtained by reviewing medical records (Table 1). The mean follow-up periods were 12.3 ± 1.1 years (range, 10.3–13.9 years) in the RA group and 12.6 ± 0.3 years (range, 12.0–12.9 years) in the OA group.
All surgical procedures were performed by three senior surgeons using the standard medial parapatellar approach, with sacrifice of the anterior and posterior cruciate ligaments in all patients. All patients were treated using the posterior-stabilized Scorpio nonrestrictive geometry (NRG) total knee prosthesis (Stryker Orthopaedics, Mahwah, NJ, USA). All implants were inserted with cement. Patients were mobilized with immediate weight-bearing as tolerated, and active exercise was initiated under supervision of a physiotherapist. Patients underwent clinical and radiographic follow-up at post-operation 2 and 6 weeks; 3, 6, 9, and 12 months; and annually thereafter. During follow-up evaluations, patients who did not return for scheduled visits were contacted by telephone. Two nurses and one private doctor found and visited non-responders.
Clinical results of Knee Society Score were classified as excellent (80–100), good (70–79), fair (60–69), or poor (< 60). Changes in patient activity and mortality within a minimum of 10 years were compared between the two groups. Activity levels were defined as follows: I, independent community ambulatory; II, community ambulatory with cane; III, community ambulatory with walker/crutches; IV, independent household ambulatory; V, household ambulatory with cane; VI, household ambulatory with walker/crutches, and VII, nonfunctional ambulatory [8]. In the analysis, Koval grades I, II, and III cases were classified as outdoor ambulatory patients who can walk outside, whereas Koval grades IV, V, VI, and VII cases were classified as shut-in patients who walk only at home. Radiographic analysis included long-leg standing radiography from the pelvis to the ankle joint for evaluating the axis, weight-bearing anteroposterior view, non-weight bearing anteroposterior view, lateral view at 30° flexion, and skyline view of the patella. Each radiograph was assessed for any radiolucent lines using the Knee Society Roentgenographic Evaluation and Scoring System [10]. Analyses of mortality status and implant survival were conducted using hospital records and/or via interviews with family members. Patients unable to attend follow-up evaluations were interviewed by telephone. During the follow-up evaluations, the same caregiver previously interviewed during the patient’s hospitalization was questioned.
Statistical analysis
To balance the differences in the basic clinical characteristics between the RA and OA groups, the propensity score matching method was used. Propensity scores were calculated for age, sex, body mass index, and diagnosis. RA and OA groups were matched 1:2 based on propensity scores, for which the matching tolerance was 0.01% (Table 2). Cumulative crude mortality rate was calculated at 3, 6, and 10 years and compared between the two groups. Kaplan–Meier survival analysis was performed for both groups for a minimum 10-year follow-up period, using mortality as the primary end point. Additionally, Kaplan–Meier survival analysis was performed for all knees for a minimum 10-year follow-up period with revision of either component as an endpoint. The correlation of survival rates in the groups was tested using the log-rank test. Student’s t-test was used to analyze age and body mass index, and the Mann–Whitney test was used to analyze Koval grade. The chi square test was used to analyze sex, Knee Society knee and function scores, and cumulative mortality. The analyses were carried out using IBM SPSS Statistics software version 18.0 (IBM, Armonk, New York, USA). All reported p values were two-sided, and p < 0.05 was considered statistically significant.
Results
The mean Knee Society knee scores in the RA and OA groups improved from 37.7 and 38.2 points preoperatively to 72.9 and 83.1 points at the final follow-up, respectively (p < 0.05). Mean preoperative function scores in the RA and OA groups improved from 36.4 and 37.1 points to 70.3 and 88.6 points at the final follow-up, respectively (p < 0.05). Better outcomes were observed in the OA group, with significant differences for the Knee Society knee score (p < 0.05) and function score (p < 0.05) (Table 3).
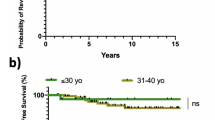
Among 48 surviving patients in the RA group at a minimum follow-up period of 10 years, 38 (79.2%) were outdoor ambulatory, and 10 (20.8%) were shut-in patients (Table 3). However, among 109 surviving patients in the OA group, 105 (96.3%) were outdoor ambulatory, and four (3.7%) were shut-in patients (Table 3). The cumulative mortality rates in the RA and OA groups were 15.8% (9/57) and 4.4% (5/114) at the final follow-up, respectively (p < 0.05) (Fig. 1 and Table 3).
A non-progressive radiolucent line (radiographic demarcation ≥ 2 mm) was observed in one femoral component and two tibial components in the RA group (3.3%) and one femoral and four tibial components in the OA group (2.8%) during serial follow-up. All femoral and tibial components in both groups were well fixed without loosening, and no obvious tibial insert polyethylene wear was observed at the final follow-up.
Regarding postoperative complications, periprosthetic joint infections in the RA and OA groups were observed in four (7.0%) and two patients (1.8%), respectively. All patients were treated by two-stage revision arthroplasty. Aseptic loosening was observed in one patient from each group (1.8%, 0.9%). All cases of aseptic loosening primarily involved the tibial component, and only the tibial component was replaced. No revision surgery was needed for any other reason, such as component malalignment, liner wear, instability, or stiffness. Periprosthetic fracture of the femoral shaft was observed in three patients (5.3%) in the RA group and one patient (0.9%) in the OA group. Kaplan–Meier survivorship analysis with revision of either component as an endpoint in the RA and OA groups estimated 94.4% (95% confidence interval, 91.8% to 98.0%) and 98.3% (95% confidence interval, 97.3% to 99.3%) chances of survival for 10 years, respectively (Fig. 2).
Discussion
The most important finding of this study was that TKAs in patients with RA showed worse functional outcomes and higher rates of mortality and revision owing to periprosthetic infections at a minimum of 10 years of follow-up.
A significant difference was observed between the two groups for the postoperative Knee Society knee score (10.2 points, p < 0.05) and function score (18.3 points, p < 0.05), with better results for the OA group. To draw clinically meaningful interpretation of the change in measures, the minimal clinically important difference (MCID) needs to be applied [11]. The MCID is between 6.1 and 6.4 for the Knee Society knee score and between 5.3 and 5.9 for function score [12]. Therefore, it was concluded that the postoperative clinical outcomes are different between the two groups.
Although several studies have reported good clinical outcomes after TKA in patients with RA [13,14,15], they provided no comparison with other control groups. Kirwan et al. [16] reported greater improvement in pain and function after TKA and total hip arthroplasty in OA patients compared to RA patients at a mean follow-up of 2.5 years. Another study reported that patients with RA had poor functional outcomes compared to those with OA at the 2- and 5-year follow-ups [17]. In this study, over a minimum 10-year follow-up period, functional outcomes might be worsened because of the progression of RA with physical disabilities. Therefore, it is assumed that inferior outcomes of TKA in patients with RA might be related to progression of the disease and the related complications in long-term follow-up.
The present study showed that the revision rate due to infectious cause was higher in RA than in OA patients, but there were no significant differences between the two groups in revision rates due to noninfectious causes such as aseptic loosening. Previous studies have demonstrated that patients with RA are at significantly higher risk of infection following TKA compared with patients undergoing TKA for OA [18, 19]. The increased risk of infection in RA patients can be attributed to the systemic effects of the disease itself and the frequent need for immunosuppressant treatment for RA [20]. The current study revealed a comparative increase in the risk of revision for periprosthetic infection.
In this study, the 15.8% mortality rate after TKA in patients with RA was higher than the 4.4% of patients with OA at a minimum follow-up period of 10 years. The higher mortality rate observed in the RA group compared to the OA group is consistent with the study reported by Mooney et al. [6]. Ohzawa et al. [7] performed a retrospective study using mortality following primary TKA in 134 patients and reported that 57.2% of the patients with RA and 95.5% of the patients with OA were surviving at 9-year follow-up. Patients suffering from RA were shown to have higher rates of pulmonary disease, cardiac morbidity, and higher mortality after surgery [21, 22]. Although direct comparison of mortality between studies is difficult owing to differences in demographic data such as age, sex, medical comorbidity, and ethnic difference, mortality after TKA in patients with RA is higher than that in patients with OA [6, 7, 23].
Interestingly, there were more periprosthetic fractures in the RA group than in the OA group, and all occurred more than 5 years after the index arthroplasty (mean, 6.9 years). The prevalence of osteoporosis in RA patients usually ranges from 15 to 59% [24, 25], and RA is often accompanied by severe osteoporosis. It is presumed that bone loss due to medical treatment and physical impairment in RA patients can result in osteoporosis and related fractures [26]. Surgeons should be aware that patients with RA are likely to be at risk of periprosthetic fracture.
This study has several limitations. First, it was retrospectively designed, and RA disease activity and the status of modern systematic treatments were not routinely documented. Therefore, RA severity could not be correlated with clinical outcomes following TKA even if the modern treatments are associated with better outcomes in the patients. Second, because few patients with confirmed RA underwent TKA at a single center, the results might not be generalizable. Third, in the implant revision rates, there were no significant differences between the two groups in noninfectious causes, such as aseptic loosening. This could be due to the relatively low numbers of revisions in this small sample size study. Lastly, this study was not a single-surgeon series; however, all surgeons were high-volume knee surgeons and used the same surgical technique and consistent perioperative protocols. The strength of this study is that it is the first study with a follow-up of more than 10 years comparing the outcomes between RA and OA in patients receiving a TKA. In our study, patients with RA were found to have lower Knee Society Scores and higher mortality and revision rates after TKA compared to a control group of TKA performed in patients with OA only.
Conclusion
In conclusion, TKA in patients with RA showed worse functional outcomes and higher mortality at a minimum follow-up period of 10 years compared to that in patients with OA. Therefore, the surgeon should accurately explain to RA patients planning to undergo TKA that, compared to OA patients, they are more likely to experience poor outcomes post-surgery.
References
Hawley DJ, Wolfe F (1991) Pain, disability, and pain/disability relationships in seven rheumatic disorders: a study of 1522 patients. J Rheumatol 18:1552–1557
Akhter E, Bilal S, Kiani A, Haque U (2011) Prevalence of arthritis in India and Pakistan: a review. Rheumatol Int 31:849–855
Yamanaka H, Sugiyama N, Inoue E, Taniguchi A, Momohara S (2014) Estimates of the prevalence of and current treatment practices for rheumatoid arthritis in Japan using reimbursement data from health insurance societies and the IORRA cohort (I). Mod Rheumatol 24:33–40
Won S, Cho SK, Kim D, Han M, Lee J, Jang EJ et al (2018) Update on the prevalence and incidence of rheumatoid arthritis in Korea and an analysis of medical care and drug utilization. Rheumatol Int 38(4):649–656
Ravi B, Escott B, Shah PS, Jenkinson R, Chahal J, Bogoch E et al (2012) A systematic review and meta-analysis comparing complications following total joint arthroplasty for rheumatoid arthritis versus for osteoarthritis. Arthritis Rheum 64(12):3839–3849
Mooney L, Lewis PL, Campbell DG, Peng Y, Hatton A (2019) Rates and outcomes of total knee replacement for rheumatoid arthritis compared to osteoarthritis. ANZ J Surg 89:184–190
Ohzawa S, Takahara Y, Furumatsu T, Inoue H (2001) Patient survival after total knee arthroplasty. Acta Med Okayama 55:295–299
Koval KJ, Aharonoff GB, Rosenberg AD, Bernstein RL, Zuckerman JD (1998) Functional outcome after hip fracture. Effect of general versus regional anesthesia. Clin Orthop Relat Res 348:37–41
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Clement ND, MacDonald D, Simpson AHRW (2014) The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(8):1933–1939
Lee WC, Kwan YH, Chong HC, Yeo SJ (2017) The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc 25(11):3354–3359
Rodriguez JA, Saddler S, Edelman S, Ranawat CS (1996) Long-term results of total knee arthroplasty in class 3 and 4 rheumatoid arthritis. J Arthroplast 11:141–145
Schai PA, Scott RD, Thornhill TS (1999) Total knee arthroplasty with posterior cruciate retention in patients with rheumatoid arthritis. Clin Orthop Relat Res 367:96–106
Trieb K, Schmid M, Stulnig T, Huber W, Wanivenhaus A (2008) Long-term outcome of total knee replacement in patients with rheumatoid arthritis. Jt Bone Spine 75:163–166
Kirwan JR, Currey HL, Freeman MA, Snow S, Young PJ (1994) Overall long-term impact of total hip and knee joint replacement surgery on patients with osteoarthritis and rheumatoid arthritis. Br J Rheumatol 33:357–360
Singh JA, Lewallen DG (2013) Better functional and similar pain outcomes in osteoarthritis compared to rheumatoid arthritis after primary total knee arthroplasty: a cohort study. Arthritis Care Res (Hoboken) 65:1936–1941
Cancienne JM, Werner BC, Browne JA (2016) Complications of primary total knee arthroplasty among patients with rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and osteoarthritis. J Am Acad Orthop Surg 24:567–574
Schrama JC, Espehaug B, Hallan G, Engesaeter LB, Furnes O, Havelin LI et al (2010) Risk of revision for infection in primary total hip and knee arthroplasty in patients with rheumatoid arthritis compared with osteoarthritis: a prospective, population-based study on 108,786 hip and knee joint arthroplasties from the Norwegian Arthroplasty Register. Arthritis Care Res (Hoboken) 62:473–479
Carbone J, Pozo N, Gallego A, Sarmiento E (2011) Immunological risk factors for infection after immunosuppressive and biologic therapies. Expert Rev Anti Infect Ther 9:405–413
Pappas DA, Giles JT, Connors G, Lechtzin N, Bathon JM, Danoff SK (2010) Respiratory symptoms and disease characteristics as predictors of pulmonary function abnormalities in patients with rheumatoid arthritis: an observational cohort study. Arthritis Res Ther 12:R104
Salmon JE, Roman MJ (2008) Subclinical atherosclerosis in rheumatoid arthritis and systemic lupus erythematosus. Am J Med 121:S3–S8
Böhm P, Holy T, Pietsch-Breitfeld B, Meisner C (2000) Mortality after total knee arthroplasty in patients with osteoarthrosis and rheumatoid arthritis. Arch Orthop Trauma Surg 120:75–78
Lee JH, Suh YS, Koh JH, Jung SM, Lee JJ, Kwok SK et al (2014) The risk of osteoporotic fractures according to the FRAX model in Korean patients with rheumatoid arthritis. J Korean Med Sci 29:1082–1089
Sinigaglia L, Nervetti A, Mela Q, Bianchi G, Puente AD, Munno OD et al (2000) A multicenter cross sectional study on bone mineral density in rheumatoid arthritis. Italian Study Group on Bone Mass in Rheumatoid Arthritis. J Rheumatol 27:2582–2589
Cortet B, Guyot MH, Solau E, Pigny P, Dumoulin F, Flipo RM et al (2000) Factors influencing bone loss in rheumatoid arthritis: a longitudinal study. Clin Exp Rheumatol 18:683–690
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial association (e.g. consultancies, stock ownership, equity interest, patent, licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethical approval
This study was approved by the Institutional Review Board (IRB) of Himchan hospital, Seoul, Republic of Korea.
Informed consent
All patients provided written informed consent to use their medical records in advance.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baek, JH., Lee, S.C., Kim, JW. et al. Inferior outcomes of primary total knee arthroplasty in patients with rheumatoid arthritis compared to patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 30, 2786–2792 (2022). https://doi.org/10.1007/s00167-021-06675-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06675-9