Abstract
Purpose
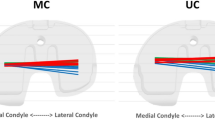
A new CR TKA design with concave medial and convex lateral tibial polyethylene bearing components was introduced recently to improve functional outcomes. This study aimed to investigate in-vivo articular contact kinematics in unilateral asymmetrical tibial polyethylene geometry CR TKA patients during strenuous knee flexion activities.
Methods
Fifteen unilateral CR TKA patients (68.4 ± 5.8 years; 6 male/9 female) were evaluated for both knees during sit-to-stand, single-leg deep lunges and step-ups using validated combined computer tomography and dual fluoroscopic imaging system. Medial and lateral condylar contact positions were quantified during weight-bearing flexion activities. The Wilcoxon signed-rank test was performed to determine if there is a significant difference in articular contact kinematics during strenuous flexion activities between CR TKA and the non-operated knees.
Results
Contact excursions of the lateral condyle in CR TKAs were significantly more anteriorly located than the contralateral non-operated knee during sit-to-stand (3.7 ± 4.8 mm vs − 7.8 ± 4.3 mm) and step-ups (− 1.5 ± 3.2 mm vs − 6.3 ± 5.8 mm). Contact excursions of the lateral condyle in CR TKAs were significantly less laterally located than the contralateral non-operated knee during sit-to-stand (21.4 ± 2.8 mm vs 24.5 ± 4.7 mm) and single-leg deep lunges (22.6 ± 4.4 mm vs 26.2 ± 5.7 mm, p < 0.05). Lateral condyle posterior rollback was not fully restored in CR TKA patients during sit-to-stand (9.8 ± 6.7 mm vs 12.9 ± 8.3 mm) and step-ups (8.1 ± 4.8 mm vs 12.2 ± 6.4 mm). Lateral pivoting patterns were observed in 80%, 73% and 69% of patients during sit-to-stand, step-ups and single-leg deep lunges respectively.
Conclusion
Although lateral femoral rollback and lateral pivoting patterns were observed during strenuous functional daily activities, asymmetric contact kinematics still persisted in unilateral CR TKA patients. This suggests the specific investigated contemporary asymmetrical tibial polyethylene geometry CR TKA design evaluated in this study does not fully replicate healthy knee contact kinematics during strenuous functional daily activities.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cruciate retaining total knee arthroplasties (TKAs) were designed to improve proprioception, restore femoral rollback and reproduce physiological knee biomechanics through the preservation of the posterior cruciate ligament (PCL) [22, 26]. It was suggested that CR TKA has the potential to improve functional outcomes and patient satisfaction [20]. However, in-vivo fluoroscopic analyses have demonstrated that CR TKA does not fully restore healthy knee kinematics in terms of femoral rollback, axial femoral rotation and knee joint rotational center [5, 28].
An asymmetrical tibial polyethylene bearing geometry CR TKA design was recently introduced to optimize knee biomechanics. However, there is a paucity of data available in the literature regarding the ability of the contemporary CR TKA design to fully restore native knee kinematics during functional daily activities. This study hypothesized that the newly designed asymmetrical tibial polyethylene bearing geometry CR TKA with its novel design features has the potential to restore in-vivo articular contact kinematics of the healthy knee during strenuous functional daily activities including step-ups, single-leg deep lunges and sit-to-stand utilizing a validated dual fluoroscopic imaging system (DFIS).
Methods
Patients
Fifteen well-functioning unilateral CR TKA patients were included in this study with the institutions’ Internal Review Board approval (Table 1). Patients underwent unilateral CR TKA (Journey II Total Knee System, Smith and Nephew, Memphis, TN, USA). The average follow-up time was 24.5 months (± 12.6, range 13–42). All patients in this study presented no radiographic signs of osteoarthritis in the contralateral non-operated knee. At the latest follow-up, there was no postoperative implant malalignment on radiographs in this cohort of patients. All patients demonstrated a satisfactory range of knee motion during a physical examination, with an average range of motion for knee flexion of 98.4° (SD 6.8°). All patients in this study also had an intact knee ligament and meniscal condition in the contralateral non-operated knee.
All CR TKA prostheses were implanted by a single surgeon. All surgeries were performed with a standard medial parapatellar approach, aiming for a neutral mechanical coronal limb alignment. Only the deep fibers of medial collateral ligament were released routinely to correct varus alignment. The femur was cut at 5° of valgus with 3° of external rotation. On the tibial side, care was taken to use a retractor to recreate the anatomic slope (as per manufacturer recommendation). Component trialing was performed to ensure balanced flexion and extension gaps. Third-generation cementation technique was used, cleaning the bone thoroughly through the use of pulse lavage, vacuum mixing of cement, and pressurized injection with cement gun.
Dual fluoroscopic imaging analysis
Patients underwent computer tomography (CT) scans (Sensation 64; Siemens; Germany) from pelvis to ankles bilaterally to generate 3D surface models of the CR TKA and the contralateral native knee. All patients performed sequential, step-ups, single-leg deep lunges and sit-to-stand (STS) under synchronized DFIS surveillance (BV Pulsera, Phillips Medical, USA) [3, 13]. The two-dimensional dynamic fluoroscopic images and the three-dimensional (3D) TKA Computer-Aided Design (CAD) models were imported into a customized program in MATLAB (MathWorks®, Natick, MA, USA) [27]. The position of each TKA component in 3D space was determined with a previously published protocol [3, 14] by performing optimal matching of TKA CAD model projections with the dynamic fluoroscopic TKA images (Fig. 1). The accuracy of the DFIS is 0.9 mm (SD 1.1 mm) in translation and 0.6° (SD 0.8°) [16]. The repeatability of the DFIS technique is less than 0.8 mm and 0.6° in position and orientation for the measurement of in-vivo kinematics in static and dynamic positions [16].
The medial and lateral anterior–posterior positions of the femoral condyles were measured by tracking the lowest point on the medial and lateral femoral condyles with respect to the tibia [9]. A coordinate system (origin in the center of the tibial plateau) on the tibial plateau was created to allow the quantitative description of contemporary CR TKA articular contact kinematics (Fig. 2). The mean contact position of the CR TKA and contralateral non-operated knees during functional activities were projected on the tibial plateau surfaces [9, 15].
3D component orientation analysis
Femoral and tibial component alignment was defined in concordance with previous literature [23]. In terms of the femoral component, the valgus angle was defined as the angle in the coronal plane from the axis formed by the lowest points on each of the condyles of the native femur [23]. For the tibial component, valgus was defined as the angle in the coronal plane from the axis formed by the centers of the circles fitted to the tibial plateau to the axis formed by the centers of the circles fitted to the tibial plateau [23].
Statistical analysis
The Wilcoxon signed-rank test was performed to determine if there is a significant difference in articular contact kinematics during strenuous flexion activities between the contemporary CR TKA design and the non-operated knees (α = 0.05) [21]. A multiple linear regression model was employed to assess the effect of 3D component orientation on in-vivo articular contact kinematics.
Results
Clinical outcome scores
At an average follow-up time of 24.5 months (± 12.6, range 13–42), the patient cohort reported the following patient-reported outcome measures: KOOS-PS (61.8 ± 10.3), PROMIS SF Physical (40.1 ± 9.7), PROMIS SF Mental (49.2 vs ± 8.8) and Physical SF 10A (43.7 ± 10.3).
In-vivo articular contact kinematics during sit-to-stand
Contact excursions of the lateral condyle in CR TKAs were significantly more anteriorly located than the contralateral non-operated knee from 9° to 40° of knee flexion (4.0 mm [IQR: 2.6; 5.6] vs − 7.3 mm [IQR: 5.0; 9.1], p < 0.05) as well as from 76° to 90° of knee flexion (− 4.8 mm [IQR: − 2.1; − 8.1] vs − 11.2 mm [IQR: 6.9; 14.4], p < 0.05) during STS (Figs. 3, 4). Articular contact excursions of the medial condyle were significantly more anteriorly located than the contralateral non-operated knee (2.4 mm [IQR: 1.5; 3.7] vs − 6.8 mm [IQR: − .4; − 9.5], p < 0.05) throughout the entire range of flexion angles during STS (Figs. 3, 4). Lateral condyle posterior rollback was not fully restored in CR TKA patients (9.1 mm [IQR: 5.2; 13.3] vs 12.9 mm [IQR: 6.6; 18.3]. Lateral pivoting patterns were observed in 80% (12/15) of patients.
Lateral and medial condyle anterior–posterior (AP) excursion, lateral-medial (LM) excursion, and femoral axial rotation exhibited in CR TKAs and the contralateral non-operated knees during sit-to-stand. The solid lines represent the median and the shaded areas represent the interquartile ranges. Black bars on the horizontal axex (Knee Flexion) indicate statistical significance difference between limbs
In-vivo articular contact kinematics during step-ups
Similar to the articular contact excursions observed during STS, contact excursions of the lateral condyle in CR TKAs were significantly more anteriorly located than the contralateral non-operated knee from 9° to 26° of knee flexion (− 1.9 mm [IQR: 0.6; − 3.8] vs − 6.0 mm [IQR: − 3.1; − 9.0], p < 0.05) as well as from 34° to 51° of knee flexion (− 4.4 mm [IQR: − 1.3; − 6.8] vs − 9.2 mm [IQR: 4.0; 12.7], p < 0.05) during step-ups (Figs. 5, 6). CR TKA experienced significantly more femoral external rotation than the contralateral non-operated knees (7.8 mm [IQR: 5.9; 10.1] vs 2.5 mm [IQR: 0.5; 5.1], p < 0.05) during step-ups (Figs. 5, 6). Lateral pivoting patterns were observed in 73% (11/15) of patients.
Lateral and medial condyle anterior–posterior (AP) excursion, lateral-medial (LM) excursion, and femoral axial rotation exhibited in CR TKAs and the contralateral non-operated knees during step-ups. The solid lines represent the median and the shaded areas represent the interquartile ranges. Black bars on the horizontal axex (Knee Flexion) indicate statistical significance difference between limbs
In-vivo articular contact kinematics during single-leg deep lunge
Articular contact excursions of the medial condyle were significantly more anteriorly located than the contralateral non-operated knee (3.9 mm [IQR: 2.3; 4.8] vs − 3.0 mm [IQR: 0.3; − 5.2], p < 0.05) throughout the entire range of knee flexion angles during single-leg deep lunges (Figs. 7, 8). Contact excursions of the lateral condyle in CR TKAs were significantly less laterally located than the contralateral non-operated knee (21.5 mm [IQR: 17.9; 24.4] vs 25.0 mm [IQR: 21.3; 27.7], p < 0.05) from 36° to 44° of knee flexion during single-leg deep lunges (Figs. 7, 8). Lateral pivoting patterns were observed in 69% (9/13) of patients.
Lateral and medial condyle anterior–posterior (AP) excursion, lateral-medial (LM) excursion, and femoral axial rotation exhibited in CR TKAs and the contralateral non-operated knees during single-leg deep lunges. The solid lines represent the median and the shaded areas represent the interquartile ranges. Black bars on the horizontal axex (Knee Flexion) indicate statistical significance difference between limbs
3D component orientation analysis
The femoral component demonstrated 0.8° ± 1.4° of internal rotation, 1.6° ± 2.0° of valgus and 2.5° ± 1.6° of posterior tilt. The tibial component showed 0.7° ± 3.1° of external rotation, 1.7° ± 1.8° of valgus and 3.3° ± 2.7° of posterior tilt. There was no significant correlation between femoral component alignment and in-vivo articular contact kinematics during single-leg deep lunge (Table 2). Similarly, there was no significant correlation between tibial component alignment and in-vivo articular contact kinematics during single-leg deep lunge (Table 2).
Discussion
The most important finding of the present study is that the contemporary asymmetrical tibial polyethylene bearing geometry CR TKA design does not fully replicate healthy knee contact kinematics during strenuous functional daily activities.
The contemporary CR TKA design did not demonstrate the same magnitude of femoral rollback compared to the contralateral non-operated knee. This is in agreement with other studies in the literature, demonstrating that mimicking the amount of femoral rollback that occurs during flexion is difficult to achieve with CR TKA designs [10, 17, 19]. Horiuchi et al. [11] evaluated a previous generation symmetrical CR TKA design (NRG CR TKA – Stryker Orthopaedics, Mahwah, New Jersey, USA) with a single anterior/posterior and medial/lateral radius to replicate physiologic femoral rollback. However, the study findings demonstrated that the CR TKA design was unable to restore posterior femoral rollback during weight-bearing knee flexion. Mikashima et al. [18] investigated a symmetric CR TKA design (Foundation and 3D Knee – DJO Surgical, Austin, Texas, USA) with a posterior lateral sulcus to simulate anterior cruciate ligament (ACL) function, however, the study results showed that the knee replacement did not restore native knee femoral rollback. As femoral rollback plays an important role in attaining high degrees of knee flexion [30], the retention of the PCL in the contemporary CR TKA has been suggested to improve knee kinematics [8]. Although our study demonstrated that physiological posterior femoral translation was retained the contemporary CR TKA design, the medial sulcus of the contemporary CR TKA may prevent additional posterior translation of the femur during knee flexion.
The contemporary CR TKA design did not reach comparable levels of posterior femoral translations when compared to the contralateral non-operated knee. However, contact kinematics such as lateral femoral condyle rollback as well as lateral pivoting patterns more closely approximated in vivo kinematics of the native knee [25]. Several other previous CR TKA designs have attempted to accomplish these physiologic kinematics through asymmetric tibial inserts and manipulation of the femoral condyles radii [6, 7], however, these knee implants failed to fully restore native knee kinematics and in some cases exhibited considerable pivoting variability. The improved lateral femoral anteroposterior rollback of the contemporary CR TKA design during the early phase of STS, single-leg deep lunge and steps-ups may be attributed to the posterior sloping of the lateral tibial plateau. Similar to the native knee, the contemporary CR TKA design demonstrated the majority of its posterior displacement on the lateral component within the first half of the strenuous activities investigated in this study. In contrast to anteroposterior contact kinematics, the contemporary asymmetrical tibial polyethylene bearing geometry CR TKA demonstrated significant medial/lateral asymmetries of the lateral compartment throughout the entire range of flexion angles. This may be attributed to the lack of the ACL, with medial displacement of contact points on the lateral component having been demonstrated in previous CR TKA designs [5, 25, 29]. Additionally, similar observations were made by Defrate et al. [7] in ACL-deficient patients.
The results of the current study need to be interpreted in light of several potential limitations. Firstly, we analyzed the articular contact kinematics between CR TKA and the contralateral non-operated, as there was no preoperative data available for comparisons. However, all patients in this study presented no radiographic signs of osteoarthritis in the contralateral non-operated knee. Secondly, all patients in the current study had a single asymmetrical tibial polyethylene bearing geometry CR TKA design with relatively short follow-up time. Thus, the findings of this study may not be generalized to different types of asymmetrical tibial polyethylene bearing geometry CR TKA system. Thirdly, the quantification of articular contact kinematics utilizes the center of two circles of each tibial plateau for the native knee, while the center of the curves of the baseplate were used for the implanted side. In patients with poorly aligned (translation and/or rotation) tibial baseplates, this may lead to inaccuracies as this would lead to the comparison of different landmarks. However, in addition to the proper alignment of all TKA components in our study cohort, this methodology has been used extensively in previous literature to quantify in-vivo articular contact kinematics in TKA patients [1, 2, 5]. Fourth, although patient-reported outcome measures are becoming an increasingly important tool for the assessment of functional outcomes, this study did not have complete data for patient-reported outcome measures for all patients [4, 12, 23]. Therefore, future studies may investigate the effect of in-vivo knee kinematics on patient-reported outcomes. Lastly, this study is limited by a small sample size; however, many studies using dual fluoroscopic imaging technology have this limitation [23,24,25], most likely due to the challenges associated with the use of this experimental technique.
Conclusion
In conclusion, the specific contemporary asymmetrical tibial polyethylene bearing geometry CR TKA design evaluated in this study demonstrated significant asymmetries in anterior–posterior and medial–lateral translations of the femoral condyles in addition to a loss in femoral posterior rollback during strenuous functional activities, when compared to the contralateral non-operated knees. This suggests that the contemporary CR TKA design is not fully able to replicate healthy knee contact kinematics during strenuous functional daily activities. This information is useful for peri-operative counselling of patients undergoing total knee arthroplasty with this contemporary CR TKA design.
Data availablity
Data are available upon request. Only standard software was used for analysis.
References
Arauz P, Klemt C, Limmahakhun S, An S, Kwon Y-M (2018) Stair climbing and high knee flexion activities in bi-cruciate retaining total knee arthroplasty. In vivo kinematics and articular contact analysis. J Arthroplasty 34:570–576
Arauz P, Peng Y, An S, Kwon Y-M (2018) In-vivo analysis of sliding distance and cross-shear in Bi-cruciate retaining total knee arthroplasty. J Biomech 77:8–15
Bingham J, Li G (2006) An optimized image matching method for determining in-vivo TKA kinematics with a dual-orthogonal fluoroscopic imaging system. J Biomech Eng 128:588–595
Bonner BE, Castillo TN, Fitz DW, Zhao JZ, Klemt C, Kwon Y-M (2019) Preoperative opioid use negatively affects patient-reported outcomes after primary total hip arthroplasty. J Am Acad Orthop Surg 27:1016–1020
Cates HE, Komistek RD, Mahfouz MR, Schmidt MA, Anderle M (2008) In vivo comparison of knee kinematics for subjects having either a posterior stabilized or cruciate retaining high-flexion total knee arthroplasty. J Arthroplasty 23:1057–1067
DeFrate LE, Gill TJ, Li G (2004) In vivo function of the posterior cruciate ligament during weightbearing knee flexion. Am J Sports Med 32:1923–1928
Defrate LE, Papannagari R, Gill TJ, Moses JM, Pathare NP, Li G (2006) The 6 degrees of freedom kinematics of the knee after anterior cruciate ligament deficiency: an in vivo imaging analysis. Am J Sports Med 34:1240–1246
Dimitriou D, Tsai T-Y, Park KK, Hosseini A, Kwon Y-M, Rubash HE, Li G (2016) Weight-bearing condyle motion of the knee before and after cruciate-retaining TKA: in-vivo surgical transepicondylar axis and geometric center axis analyses. J Biomech 49:1891–1898
Grieco TF, Sharma A, Dessinger GM, Cates HE, Komistek RD (2018) In vivo kinematic comparison of a bicruciate stabilized total knee arthroplasty and the normal knee using fluoroscopy. J Arthroplasty 33:565–571
Grieco TF, Sharma A, Komistek RD, Cates HE (2016) Single versus multiple-radii cruciate-retaining total knee arthroplasty: an in vivo mobile fluoroscopy study. J Arthroplasty 31:694–701
Horiuchi H, Akizuki S, Tomita T, Sugamoto K, Yamazaki T, Shimizu N (2012) In vivo kinematic analysis of cruciate-retaining total knee arthroplasty during weight-bearing and non-weight-bearing deep knee bending. J Arthroplasty 27:1196–1202
Klemt C, Tirumala V, Oganesyan R, Xiong L, den van Kieboom J, Kwon Y-M (2020) Single-stage revision of the infected total knee arthroplasty is associated with improved functional outcomes: a Propensity Score Matched Cohort Study. J Arthroplasty 20:883–5403
Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, Li G (2009) Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech 42:1877–1884
Li G, Van de Velde SK, Bingham JT (2008) Validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion. J Biomech 41:1616–1622
Li G, Wuerz TH, DeFrate LE (2004) Feasibility of using orthogonal fluoroscopic images to measure in vivo joint kinematics. J Biomech Eng 126:314–318
Lin H, Wang S, Tsai T-Y, Li G, Kwon Y-M (2013) In-vitro validation of a non-invasive dual fluoroscopic imaging technique for measurement of the hip kinematics. Med Eng Phys 35:411–416
Mendez JH, Mehrani A, Randolph P, Stagg S (2019) Throughput and resolution with a next-generation direct electron detector. IUCrJ 6:1007–1013
Mikashima Y, Tomatsu T, Horikoshi M, Nakatani T, Saito S, Momohara S, Banks SA (2010) In vivo deep-flexion kinematics in patients with posterior-cruciate retaining and anterior-cruciate substituting total knee arthroplasty. Clin Biomech 25:83–87
Most E, Li G, Sultan PG, Park SE, Rubash HE (2005) Kinematic analysis of conventional and high-flexion cruciate-retaining total knee arthroplasties: an in vitro investigation. J Arthroplasty 20:529–535
Nabeyama R, Matsuda S, Miura H, Kawano T, Nagamine R, Mawatari T, Tanaka K, Iwamoto Y (2003) Changes in anteroposterior stability following total knee arthroplasty. J Orthop Sci 8:526–531
Nosrati M, Dey D, Mehrani A, Strassler SE, Zelinskaya N, Hoffer ED, Stagg SM, Dunham CM, Conn GL (2019) Functionally critical residues in the aminoglycoside resistance-associated methyltransferase RmtC play distinct roles in 30S substrate recognition. J Biol Chem 294:17642–17653
Nozaki H, Banks SA, Suguro T, Hodge WA (2002) Observations of femoral rollback in cruciate-retaining knee arthroplasty. Clin Orthop Relat Res 404:308–314
Peng Y, Arauz P, An S, Limmahakhun S, Klemt C, Kwon Y-M (2019) Does component alignment affect patient reported outcomes following bicruciate retaining total knee arthroplasty? An in vivo three-dimensional analysis. J Knee Surg 33:798–803
Peng Y, Arauz P, Desai P, Byers A, Klemt C, Kwon Y-M (2019) In vivo kinematic analysis of patients with robotic-assisted total hip arthroplasty during gait at 1-year follow-up. Int J Med Robot 15:2021–2027
Qi W, Hosseini A, Tsai T-Y, Li J-S, Rubash HE, Li G (2013) In vivo kinematics of the knee during weight bearing high flexion. J Biomech 46:1576–1582
Simmons S, Lephart S, Rubash H, Pifer GW, Barrack R (1996) Proprioception after unicondylar knee arthroplasty versus total knee arthroplasty. Clin Orthop Relat Res 331:179–184
Tsai T-Y, Li J-S, Wang S, Lin H, Malchau H, Li G, Rubash H, Kwon Y-M (2013) A novel dual fluoroscopic imaging method for determination of THA kinematics: in-vitro and in-vivo study. J Biomech 46:1300–1304
Victor J, Banks S, Bellemans J (2005) Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br 87:646–655
Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty 20:777–783
Zambianchi F, Fiacchi F, Lombari V, Venturelli L, Marcovigi A, Giorgini A, Catani F (2018) Changes in total knee arthroplasty design affect in-vivo kinematics in a redesigned total knee system: a fluoroscopy study. Clin Biomech 54:92–102
Funding
The study did not receive any funding.
Author information
Authors and Affiliations
Contributions
CK: data collection, analysis, write-up; JD: data collection, analysis, write-up; VT: data collection, analysis; Y-MK: analysis, write-up.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflict of interest or financial disclosures.
Ethical approval
This study was approved by the internal Institutional Review Board at Massachusetts General Hospital/Harvard Medical School (ID: 2013P000821).
Informed consent
All patients provided written consent prior to enrolment into the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Klemt, C., Drago, J., Tirumala, V. et al. Asymmetrical tibial polyethylene geometry-cruciate retaining total knee arthroplasty does not fully restore in-vivo articular contact kinematics during strenuous activities. Knee Surg Sports Traumatol Arthrosc 30, 652–660 (2022). https://doi.org/10.1007/s00167-020-06384-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06384-9