Abstract
Purpose
Long-term failure of total knee arthroplasty (TKA) is mostly due to loosening of the prosthesis. In this study, the short- and mid-term revision rates of cemented vs cementless TKAs were investigated. Comparable short- and mid-term survival rates of both fixation methods were expected.
Methods
Data on all cemented and cementless TKAs performed between 2007 and 2017 were retrieved from the Dutch Arthroplasty Register. The cumulative crude incidence of revision of cemented and cementless TKA was calculated. Death was considered a competing risk. Revision rates were compared using multivariable Cox proportional hazard regression analysis. The associations between fixation method and type of revision or reason for revision were tested using logistic regression analyses.
Results
In total, 190,651 (94.8%) cemented and 10,560 (5.3%) cementless TKAs were evaluated. Both groups had comparable case characteristics. Cemented TKAs were inserted more often in cases with previous knee surgery compared to cementless TKAs (32% vs 27%). The cumulative incidence of revision after 9 years was 5.5% (CI 5.3–5.6%) for cemented and 5.8% (CI 5.2–6.4%) for cementless TKAs (p = 0.2). Cementless TKAs were more often revised due to loosening of the tibial (27% vs 18%; p < 0.001) or the femoral component (7% vs 5%; p = 0.005) than cemented TKAs. Cemented TKAs were more often revised due to infection (17% vs 9%; p = 0.004) than cementless TKAs.
Conclusion
In conclusion, cemented and cementless TKAs have comparable short- and mid-term revision rates based on a nationwide register study.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is performed in large numbers in the Netherlands; over 24,000 TKAs are placed annually, with the large majority (95%) being cemented [9]. Cemented TKA has the advantage of immediate stability of the implant and less chance of periprosthetic fractures [13]. Cementless fixation has the disadvantage of an increased risk for early migration of the prosthesis, especially migration of the tibial component in patients with osteoarthritis [2, 12]. However, cementless fixation has multiple theoretical advantages over cemented fixation, such as lower risk of embolism, better bone stock, shorter operation time and absence of cement debris [11, 12]. Furthermore, Carlsson et al. stated that cementless implants seem to settle firmly over time, whereas the cemented implants might continuously migrate [2].
Although cementless TKA shows more early migration than cemented TKA, previous studies have shown that after short-term follow-up, no significant differences in revision rates were found between cemented and cementless TKA in the general population with primary TKA [3, 18]. Also, a recent meta-analysis showed that there are no differences in mid-term implant survivorship and clinical outcomes between cementless and cemented fixation in primary TKA [22]. Although these studies show that short- and mid-term survival rates of both fixation methods are comparable, none of these studies used national register data, which makes the results of these studies less reliable. Moreover, the survival of cementless and cemented TKA in specific patient groups and differences in reason of revisions between both fixation methods remain unknown.
The aim of this study is to determine the short- and mid-term revision rate of cemented TKA compared to cementless TKA based on data from the population-based Dutch Arthroplasty Register (LROI). In addition, this study aims to compare the number of revisions (stratified by osteoarthritis (OA) vs non-OA, age and ASA-score), type of revision and reasons for revision between cemented and cementless fixation. This will help surgeons to make a well-informed decision. The first hypothesis is that short- and mid-term survival rates of cementless TKA and cemented TKA are comparable, both in OA and non-OA patients. The second hypothesis is that the reasons for revision and the types of revision differ between cementless and cemented TKA, namely more revisions due to loosening of the tibial component and more partial revisions are expected in cementless TKA than in cemented TKA.
Materials and methods
The Dutch arthroplasty register
The Dutch Arthroplasty Register is a nationwide population-based register, initiated by the Dutch Orthopedic Association (NOV), which contains information on joint arthroplasties performed in the Netherlands since 2007. In 2013, the completeness of primary TKA registration was 96% [19], which improved to 99% in more recent years [9].
Data collection
Patient characteristics and surgical details of all cemented and cementless primary TKA procedures registered in the Dutch Arthroplasty Register and performed between 2007 and 2017 were included (n = 201,211). Hybrid prostheses (n = 10,986) were excluded, as in the Netherlands hybrid prostheses are frequently used in patients with different patient characteristics than cemented and cementless prostheses. The overall mean age was 68.5 years with a standard deviation of 9.4 years. Sixty-five percent of all cases was female. The overall mean body mass index (BMI) was 29.7 kg/m2 with a standard deviation of 5.1 kg/m2. The overall physical condition was scored using the ASA score (I–IV). The ASA score was in 67.2 percent ASA II, 17.9 percent ASA I and in 14.9 percent ASA III.
Primary TKA was defined as the first implantation of a total knee prosthesis to replace the original joint. Knee revision arthroplasty was defined as any change (insertion, replacement or removal) of one or more components of the primary prosthesis. Revision procedures were categorized into major revision (revision of at least the femoral or tibial component) and minor revision (patella and/or insert revision only) [15]. The category “any type of revision” was reserved for combinations of major revisions and/or minor revisions, unknown types of revision and addition of the patella component. Addition of the patella component was evaluated separately. The moment of death of the deceased patients was obtained from Vektis, a national insurance database which records the vital status of all Dutch citizens [20].
Statistical data analysis
All statistical analyses were performed using SPSS version 24.0 (IBM Corp, Armonk, NY, USA). p values below 0.05 were considered statistically significant. In case of multiple testing, a Bonferroni correction was applied to avoid type I errors.
Case characteristics were stratified for cemented and cementless TKA. Continuous variables with Gaussian distribution are presented as mean and standard deviation (SD), otherwise as median and interquartile range (IQR) or number and percentage.
Survival time was calculated as the time from primary TKA to first revision arthroplasty for any reason, to the death of the patient, or to the end of the study follow-up (January 1, 2018). For the short-term (i.e. 3 years) and mid-term analyses (i.e. 9 years), all-cause cumulative crude incidence of revision of cemented and cementless TKA was calculated, where death was considered to be a competing risk [8, 21]. The median follow-up was 3.9 years (IQR: 1.9–6.4 years).
Adjusted revision rates of cemented and cementless TKA were compared using multivariable Cox proportional hazard regression analysis. Revision rates were adjusted for the confounders age at surgery, gender, ASA score, previous surgery and diagnosis at primary TKA [OA vs non-OA (i.e. rheumatoid arthritis (RA), posttraumatic, osteonecrosis, inflammatory arthritis, tumour (primary) and tumour (metastasis)]. BMI, Charnley score and smoking status were excluded from analysis because they have only been registered since 2014. For all covariates added to the model, the proportional hazards assumption was inspected using log-minus-log curves.
Cases were stratified by diagnosis at primary TKA (OA vs non-OA) or age and ASA score to compare the numbers of revisions between patient groups. To test the association between the fixation method and the number of revisions stratified into major and minor revision in each group, logistic regression analyses were used.
The association between fixation method of TKA and type of revision was tested using logistic regression analyses. The association between fixation method and reasons for revision was also tested using logistic regression analyses and stratified into major and minor revisions. Each revision could have more than one selected reason.
Ethics, data sharing plan, funding and potential conflicts of interest
The data were registered confidentially with patient consent and in accordance with Dutch and EU data protection rules. Data were made accessible by application to the LROI. All available data were anonymous. This research received no specific grant from any funding agency. The authors have no conflicts of interest to declare.
Results
Case characteristics
A total of 201,211 TKAs were included, 94.8% of which (n = 190,651) were cemented and 5.2% (n = 10,560) were cementless. Cementless fixation was used in 64 of the 102 hospitals in the Netherlands registered in the Dutch Arthroplasty Register. Case characteristics and surgical details are presented in Table 1. BMI, Charnley score and smoking status were missing for 109,284 patients (54.3%). In the cemented group, the percentage of patients who had undergone previous knee surgery was higher than in the cementless group (30.8% vs 25.2%). In addition, the percentage of patients who received a patella component was higher in the cemented group than in the cementless group (22.1% vs 2.3%).
Revision rates
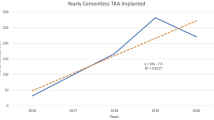
Figure 1 shows the cumulative incidence of revision in TKA stratified by fixation technique. The cumulative incidence of revision within 3 years was 3.4% (CI 3.3–3.5%) for the cemented group and 3.7% (CI 3.3–4.1%) for the cementless group. Within 9 years, 5.5% (CI 5.3–5.6%) of the cemented TKAs and 5.8% (CI 5.2–6.4%) of the cementless TKAs were revised. In the crude model as well as after adjustments, this difference was not statistically significant (Table 2).
In both the OA and the non-OA group, cases with a cementless primary TKA were more likely to undergo a major revision than cases with a cemented TKA [OR 1.4 (CI 1.2–1.6; p = 0.001) and OR 1.8 (CI 1.1–2.9; p = 0.015), respectively, Table 3]. Also, in the group of 60 to 69 years old with an ASA score of I or II, cases with a cementless TKA were more likely to undergo a major revision than cases with a cemented TKA [OR 1.3 (CI 1.1–1.6; p = 0.002); Table 4].
Revision characteristics
Nine years after surgery, 6903 (3.6%) of the cemented TKAs and 453 (4.3%) of the cementless TKAs were revised. More partial revisions (i.e. revision of at least the tibial or femoral component) were performed in cementless TKAs than in cemented TKAs [25.4% vs 14.9%; OR 2.1 (CI 1.7–2.5), p < 0.001]. More total revisions were performed in cementless TKAs than in cemented TKAs, namely 30.3% and 29.2%, respectively [OR 1.3 (CI 1.0–1.5), p = 0.01; Table 5].
The three most common reasons for a minor revision in cemented and cementless TKA were instability, infection and patellar pain. The numbers of revisions due to instability, infection or patellar pain did not differ significantly between cemented and cementless TKA after Bonferroni correction (p > 0.001). Minor revisions due to arthrofibrosis were significantly less common in cemented TKA than in cementless TKA (4.7% vs 14.2%, p < 0.001).
The three most common reasons for a major revision in cemented and cementless TKA were loosening of the tibial component, instability and malalignment. The numbers of revisions due to loosening of the tibial component, instability or malalignment did not differ significantly between cemented and cementless TKA after Bonferroni correction (p > 0.001). Major revisions due to infection were significantly more common in cemented TKA than in cementless TKA after applying a Bonferroni correction (18.2% vs 9.2%; p < 0.001; Table 6).
Discussion
The most important finding of this study was the comparable revision rates of cemented and cementless TKA after 9 years based on data from the population-based Dutch Arthroplasty Register. These results are comparable to the meta-analysis of Zhou et al. which showed no significant differences in implant survival and clinical efficacy between cemented and cementless fixation [22]. The results of the present study also confirm the results of Cherian et al. [3] who stated that short-term survival is comparable between cemented and cementless TKA. The results of the present study are also in accordance with the findings of Van der List et al. [17] who described a 5-, 10- and 15-year survival of cementless TKA of 97.7%, 95.4% and 93.0%, respectively. In contrast to previous studies, the present register study included more cases and the data were nearly complete, which makes the present study more accurate. However, long-term revision rates should still be evaluated.
Stratification by age and ASA score showed comparable revision numbers in cemented and cementless TKAs for each group. No significant difference in the number of revisions was found between the two types of fixation in older patients with a high ASA score and younger patients with a low ASA score. This suggests that there is no need to reserve the cementless TKA especially for younger and healthier patients. Kim et al. and Franceschetti et al. found no significant differences in terms of clinical, functional and radiological outcomes between cemented and cementless TKA in patients younger than 55 and 60 years, respectively [5, 7]. These studies showed good results of the young patients with cementless TKA, but did not compare young patients with old patients. The result of the present study might be explained by good ingrowth of the hydroxyapatite-coated implants in both elderly and young patients, as found by Dixon et al. [5]. Furthermore, our study showed that both in OA and in non-OA cases, major revisions were required more frequently in cementless TKA than in cemented TKA, which suggests that a cemented TKA could be better in both OA cases as well as in non-OA cases. This result might be due to the low number of cases with non-OA and the low number of revisions in both groups.
In both cemented and cementless TKA, the most frequent reason for revision is loosening of the tibial or femoral component. The results of the present study show that cementless TKAs were more often revised due to loosening of the tibial component or loosening of the femoral component than cemented TKAs. This finding may be explained by an RSA study with Interax TKAs by Pijls et al., which found a three-time higher revision rate due to aseptic loosening for uncoated uncemented tibial components than for cemented tibial components [12]. A recent radiostereometric analysis (RSA) study by Van Hamersveld et al. showed that the tibial component of a cementless total knee prosthesis coated with peri-apatite (PA) showed more overall migration than the tibial cemented component of a cemented total knee prosthesis [18]. However, post hoc analysis showed that this difference was caused by the migration of PA-coated components in the first 3 months. After these 3 months, a stable migration pattern was observed. Clinically, there was no significant difference in outcome between the groups after short-term follow-up [18]. Nakama et al. confirmed the outcome of Van Hamersveld et al. in a review, but even found that the risk of future aseptic loosening with cementless fixation was approximately half that of cemented fixation according to the arthroplasty instability classification [10]. Besides PA-coated or HA-coated cementless TKA, there are also newer designs of cementless TKA fixation, such as porous tantalum, which have better surface characteristics. Hu et al. [6] showed in their meta-analysis that the survival of cementless porous tantalum monoblock tibia component seems similar to the survival of the conventional cemented modular tibia component at 5-year follow-up. This could indicate that newer designs like cementless porous tantalum components have better surface characteristics than PA or HA components. Long-term survival of these prosthesis’ designs has not been described yet.
Besides the relevance of good implantation to prevent varus, valgus and stress shielding, another possible explanation for more revision due to loosening of the tibial component or the femoral component in cementless TKAs than cemented TKAs could be the stem design [2]. The shape of the stem needs to be different in cementless TKA than in cemented TKA. In addition, the length of the stem could be the problem. Scott et al. [14] showed that a longer stem could be used in cementless TKA with the advantages of resistance to shear reduced tibial lift-off and increased stability by reducing micro-motion. However, longer stems may have disadvantages, including stress shielding along the length of the stem, which is associated with an increase in bone loss, reduction in bone density and a theoretical risk of subsidence and loosening, periprosthetic fracture and end-of-stem pain. Furthermore, lengthening the stem of the primary cementless tibial plateau could make any revision more difficult. Lengthening, size, material and coating of the stem could be among the many factors that contribute to the migration of the prosthesis, besides the relevance of patient characteristics, such as thickness of the cortical bone and bone density.
The results of the present study showed a significantly higher number of revisions due to infection in cemented TKAs (27.8%) than in cementless TKAs (14.2%). This is in contrast to a previous study by Anis et al. [1] who analysed the 2-year overall infection rate in cemented and cementless TKAs and found no significant difference. Possible confounders of the results of the present study are not only operation time, hospital, experience of the surgeon, but also type of cement, cementation time and case characteristics. Furthermore, infections are only registered in the Dutch Arthroplasty Register if they lead to revision of one of the components. If cases undergo a debridement, antibiotics and implant retention (DAIR) procedure without revision of one of the components, the infection is not registered. Moreover, the definition of infection is arbitrary. Infections in this register-based study were not confirmed with microbiology results.
The increased infection rate in cemented TKAs found in this study may have been due to the chemical composition of the cement. Cordero et al. [4] already described in 1996 that PMMA cement usually appears to be the implant material most prone to causing infection, while titanium (Ti) and cobalt–chromium (CoCr) are the materials least likely to cause infection. Furthermore, Turhan [16] stated that the incidence of deep infections in cemented TKA was not reduced by the use of antibiotic-loaded bone cement. This suggests that it could be possible that bone ingrowth of porous cementless TKAs enables better access of the body’s inflammatory system than using a second matrix such as antibiotic-loaded bone cement. However, more studies should be performed to gain more insight into the underlying causes of infections in cemented and cementless TKAs.
The strength of this study is the large number of registry data used from the Dutch Arthroplasty Register with a completeness of nearly 100% [9, 21]. Because TKAs have a good survival and a relatively low revision rate, only large register studies can accurately evaluate the effect of fixation type on the revision rate. Furthermore, almost all revisions performed in the Netherlands are registered. This makes the results on revision characteristics reliable. Finally, cementless TKAs are performed in 64 out of 102 hospitals in the Netherlands, which ensures objective results reflecting the entire population.
Nevertheless, register data also have their drawbacks since data have not been collected prospectively and the number of variables that have been registered is limited. While the present register study provides possible explanations for the differences between cemented and cementless TKAs in terms of reason for revision and type of revision, these explanations will have to be verified by prospective cohort studies such as randomized controlled trials.
A limitation of this study is the exclusion of the possible confounders BMI, Charnley score and smoking in the analyses, as these data are unknown for more than half of the patients. Furthermore, no corrections were made for possible confounders such as operating surgeon, treatment hospital and other characteristics that could indicate the health care team’s experience in the chosen fixation method, as these data were not available. Also, no corrections were made for type of implant. However, the annual report of the LROI shows that the five most frequently registered knee prostheses were used in 86.8% of the primary TKAs. The annual report shows that the revision percentages of different types of prosthesis used in cemented primary TKAs do not differ [9]. Therefore, no large effect on the results was expected.
Conclusion
Based on population-based register data from the Netherlands, cemented and cementless TKAs showed comparable short-term and mid-term revision rates, which confirms that cemented and cementless fixation both are safe and effective fixation methods in TKA. Based on the findings in this study, there is no preferred fixation technique for OA and non-OA cases, elderly or cases with a high ASA score. As the long-term survival of TKAs is still unknown, the choice of fixation method remains dependent on the surgeon’s preference and experience.
References
Anis HK, Ramanathan D, Sodhi N, Klika AK, Piuzzi NS, Mont MA et al (2019) Postoperative infection in cementless and cemented total knee arthroplasty: a propensity score matched analysis. J Knee Surg. https://doi.org/10.1055/s-0039-1678678
Carlsson A, Bjorkman A, Besjakov J, Onsten I (2005) Cemented tibial component fixation performs better than cementless fixation: a randomized radiostereometric study comparing porous-coated, hydroxyapatite-coated and cemented tibial components over 5 years. Acta Orthop 76:362–369
Cherian JJ, Banerjee S, Kapadia BH, Jauregui JJ, Harwin SF, Mont MA (2014) Cementless total knee arthroplasty: a review. J Knee Surg 27:193–197
Cordero J, Munuera L, Folgueira MD (1996) The influence of the chemical composition and surface of the implant on infection. Injury 27(Suppl 3):SC34–37
Franceschetti E, Torre G, Palumbo A, Papalia R, Karlsson J, Ayeni OR et al (2017) No difference between cemented and cementless total knee arthroplasty in young patients: a review of the evidence. Knee Surg Sports Traumatol Arthrosc 25:1749–1756
Hu B, Chen Y, Zhu H, Wu H, Yan S (2017) Cementless porous tantalum monoblock tibia vs cemented modular tibia in primary total knee arthroplasty: a meta-analysis. J Arthroplasty 32:666–674
Kim YH, Park JW, Lim HM, Park ES (2014) Cementless and cemented total knee arthroplasty in patients younger than fifty five years. Which is better? Int Orthop 38:297–303
Lacny S, Wilson T, Clement F, Roberts DJ, Faris PD, Ghali WA et al (2015) Kaplan-Meier survival analysis overestimates the risk of revision arthroplasty: a meta-analysis. Clin Orthop Relat Res 473:3431–3442
LROI (2018) Online annual report. www.lroi-rapportage.nl/2018. Accessed 2 May 2019
Nakama GY, Peccin MS, Almeida GJ, Lira Neto Ode A, Queiroz AA, Navarro RD (2012) Cemented, cementless or hybrid fixation options in total knee arthroplasty for osteoarthritis and other non-traumatic diseases. Cochrane Database Syst Rev 10:CD006193
Newman JM, Sodhi N, Khlopas A, Sultan AA, Chughtai M, Abraham R et al (2018) Cementless total knee arthroplasty: a comprehensive review of the literature. Orthopedics 41:263–273
Pijls BG, Nieuwenhuijse MJ, Schoones JW, Middeldorp S, Valstar ER, Nelissen RG (2012) RSA prediction of high failure rate for the uncoated Interax TKA confirmed by meta-analysis. Acta Orthop 83:142–147
Prudhon JL, Verdier R (2017) Cemented or cementless total knee arthroplasty? Comparative results of 200 cases at a minimum follow-up of 11 years. SICOT J 3:70
Scott CE, Biant LC (2012) The role of the design of tibial components and stems in knee replacement. J Bone Joint Surg Br 94:1009–1015
Spekenbrink-Spooren A, Van Steenbergen LN, Denissen GAW, Swierstra BA, Poolman RW, Nelissen R (2018) Higher mid-term revision rates of posterior stabilized compared with cruciate retaining total knee arthroplasties: 133,841 cemented arthroplasties for osteoarthritis in the Netherlands in 2007–2016. Acta Orthop 89:640–645
Turhan S (2019) Does the use of antibiotic-loaded bone cement have an effect on deep infection in primary total knee arthroplasty practice? Surg Infect (Larchmt) 20:244–246
van der List JP, Sheng DL, Kleeblad LJ, Chawla H, Pearle AD (2017) Outcomes of cementless unicompartmental and total knee arthroplasty: a systematic review. Knee 24:497–507
van Hamersveld KT, Marang-van de Mheen PJ, Tsonaka R, Valstar ER, Toksvig-Larsen S (2017) Fixation and clinical outcome of uncemented peri-apatite-coated versus cemented total knee arthroplasty : five-year follow-up of a randomised controlled trial using radiostereometric analysis (RSA). Bone Joint J 99-B:1467–1476
van Steenbergen LN, Denissen GA, Spooren A, van Rooden SM, van Oosterhout FJ, Morrenhof JW et al (2015) More than 95% completeness of reported procedures in the population-based Dutch Arthroplasty Register. Acta Orthop 86:498–505
Vektis (2018) www.vektis.nl. Accessed 22 Mar 2018
Wongworawat MD, Dobbs MB, Gebhardt MC, Gioe TJ, Leopold SS, Manner PA et al (2015) Editorial: estimating survivorship in the face of competing risks. Clin Orthop Relat Res 473:1173–1176
Zhou K, Yu H, Li J, Wang H, Zhou Z, Pei F (2018) No difference in implant survivorship and clinical outcomes between full-cementless and full-cemented fixation in primary total knee arthroplasty: a systematic review and meta-analysis. Int J Surg 53:312–319
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to the manuscript. CQ, TD, HV and RD contributed to the design of the study. CQ, AS and LS collected the data. CQ, AS, LS and JP performed the data analysis and statistical analysis. CQ, SB, JP and RD interpreted and discussed the results. CQ, SB, TD, JP and HV drafted the manuscript. All authors critically revised the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No authors have conflicts of interest.
Ethical approval
Ethical approval has been evaluated by the LROI.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Quispel, C.R., Duivenvoorden, T., Beekhuizen, S.R. et al. Comparable mid-term revision rates of primary cemented and cementless total knee arthroplasties in 201,211 cases in the Dutch Arthroplasty Register (2007–2017). Knee Surg Sports Traumatol Arthrosc 29, 3400–3408 (2021). https://doi.org/10.1007/s00167-020-06183-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06183-2