Abstract
Purpose
This study aimed to evaluate the effects of scapular-focused treatment with (SFTF) and without (SFT) feedback on pain, function, and scapular kinematics in patients with Shoulder Impingement Syndrome (SIS).
Methods
Seventy-five males and females with SIS were randomly assigned into SFTF (n = 25), SFT (n = 25) and control (n = 25) groups. The primary outcome was pain, assessed by Visual Analog Scale (VAS). The secondary outcomes were function and scapular kinematics, assessed by DASH Questionnaire and a 3-D motion capture, respectively. All outcomes were measured at the baseline and after the 8-week interventions.
Results
A post hoc analysis performed to show significant differences between groups after the 8-week interventions. For pain, there were significant differences between SFTF vs. SFT (ES (95% CI) = − 0.3(− 0.4 to − 0.1); P = 0.04), SFTF vs. control (ES (95% CI) = 1.3(0.7–1.9); P = 0.01). For DASH, also, there were significant differences between SFTF vs. SFT (ES (95% CI) = 1.8(1.1–2.4); P = 0.03), SFTF vs. control (ES (95% CI) = 4.4(3.3–5.4); P = 0.01), and SFT vs. control (ES (95% CI) = 2.6(1.8–3.4); P = 0.01). For scapular internal rotation (the sagittal or scapular planes), scapular upward rotation, and the scapular tilt, however, there were no differences between SFTF vs. SFT.
Conclusion
Based on the study results, a rehabilitation program integrated with verbal feedbacks is effective to relieve pain, and improve function and scapular kinematics in patients with SIS. Adding feedback to an exercise therapy could clinically enhance outcomes in patients with SIS.
Level of evidence
Level II.
Trial registration
This study was prospectively registered at UMIN-CTR website, and the unique trail number is UMIN000036399.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shoulder impingement syndrome (SIS) is a common musculoskeletal disorder observed in both athletic and non-athletic population [11, 15, 16, 19]. In fact, SIS has been reportedly diagnosed to account for 44–65% of all shoulder complaints resulted in loss of function, and motor control deficits [30]. This syndrome has been described by a narrowing of the subacromial space that causes encroachment of the subacromial tissues, including the rotator cuff and the subacromial bursa [19]. It could be usually caused by repeated, tedious actions or movements with arm raised above the head in swimming, throwing, installing devices, playing golf, shoveling snow, etc. In elderly individuals, the pain-provoking factor is a contracture of the anterior shoulder complex structures caused by a rounded shoulder posture with protracted shoulders, and injury or degenerations in the joint area [12].
However, conflicting, altered scapular positioning and movement patterns may be critical risk factors for SIS [6, 16, 24]. In this regard, kinematic changes may occur in patients with shoulder impingement resulting in a further decrease in supraspinatus muscle activation [1, 10, 13, 25]. Excessive superior or anterior translation of the humeral head on the glenoid fossa, inadequate external rotations of the humerus, a decrease in normal scapular upward rotation, and posterior tipping on the thorax during shoulder elevation could cause shoulder impingement. Additionally, the hypothesized kinematic alterations in scapular motions have been linked to decrease in serratus anterior muscle activity, to increase in upper trapezius muscle activity, or to unbalanced forces between the upper and lower trapezius muscle [18].
Therefore, it seems that to treat SIS, the focus should be on stretching, strengthening, and neuromuscular control exercises for scapula muscles [7, 8]. It has been reported that a scapular-focused treatment (SFT) improves scapular upward rotation (as one of the main SIS incidence causes) [1] and movement patterns [16].
As monitoring scapular movements during exercise is impossible, shoulder exercises need feedbacks with verbal, visual, and kinesthetic stimuli to help the patients with shoulder pain to control abnormal movements, and maintain posture [28]. In this regard, Weon et al. [31] reported that real-time visual feedback using a video can provide an immediate and continuous feedback to correct scapular movements during independent shoulder flexion exercises, and this results in better activation of the upper trapezius and serratus anterior muscles in those patients with scapular winging.
No randomized controlled trial (RCT) has so far conducted to combine SFT and feedback (SFTF) to treat patients with SIS. Therefore, this study investigated the effects of an 8-week SFT with and without feedback on pain, function and scapular kinematics in participants with SIS. It was hypothesized that adding feedback to a shoulder exercise treatment in clinical setting may enhance the outcomes in participants with SIS.
Materials and methods
The study was performed in accordance with the ethical standards in the World Medical Association Declaration of Helsinki (2002). Ethical approval was obtained from the Ethical Committee of the Kharazmi University and Faculty of the Sport Sciences and the ethical standards in sport and exercise science research were respected (IRB ID number = Kharazmi.REC 20190601/34).
This RCT (UMIN000036399) with a 1:1 ratio allocation was conducted in and approved by the department of Sport Sciences. All the participants were fully informed about the nature of the study, and they signed an informed consent agreement. The examiners were blinded to group assignment.
Participants
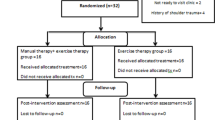
The participants were recruited by orthopedic physicians via flyers displayed at hospitals and the university in May and June 2019. Based on the criteria, 75 males and females were randomly assigned into the scapular-focused treatment (SFT) (n = 25), SFT with Feedback (SFTF) (n = 25), and control (n = 25) groups (Fig. 1). The group allocation was performed using a computer-generated, randomized list, created by a person not involved in recruiting procedure. After pre-intervention measurements, the first author opened the sealed envelopes and assigned the individuals into one of the groups. There was no significant difference between participants’ demographic data at baseline (Table 1). The sessions which the participants attended in each group are as follows: SFT group, 22 ± 1 sessions, SFTF group, 21 ± 1 sessions, and control group 22 ± 1 sessions. No adverse events were reported.
Inclusion and exclusion criteria
Participants with shoulder pains, lasted > 6 weeks, were included in the study. A consulting orthopedic surgeon diagnosed the participants with SIS if they exhibited at least two of the following items: painful arc during flexion or abduction; a positive Neer or Hawkins–Kennedy test; and painful resisted external rotation, abduction, or Jobe test [21, 29].
Participants were excluded if they had a history of surgery, fracture, or dislocation and traumatic onset of shoulder pains; existence of type 3 acromion; massive rotator cuff tear; a long head of bicep tendon tear; or degenerative joint disorder at the shoulder complex, any rheumatologic, systemic, or neurologic disorders; any neuro-musculoskeletal disorder (including cervical radiculopathy) [21, 23, 29], a body mass index > 30 kg/m2; being pregnant, and, receiving steroid injections and physical therapy during the previous 6 months preceding the study [21, 23, 29].
Procedures
The participants were assessed before (pre-intervention) and after the 8-week interventions (post-intervention). Pain, function and scapular kinematics were meatured as dependent variales. Only the involved side of each participant was assessed.
Primary outcome measure (pain)
Secondary outcomes (DASH, and 3D scapular kinematics)
Disability of the arm, shoulder, and hand (DASH) questionnaire was used to assess the upper limb functions. The DASH questionnaire has been identified and used as an upper extremity specific orthopedic outcome assessment tool [9, 20]. This version of the DASH questionnaire has been proved to be valid and highly reliable, with intra-observer and interobserver intraclass correlation coefficients (ICCs ˃ 0.90) [9, 20]. A recent study showed that a 10-point decrease on the DASH questionnaire can be considered a clinically important improvement [9].
Also, the scapular motion was recorded with nine infrared cameras (Vicons MX13, Oxford Metrics Ltd., Oxford, UK). Markers were fixed on the seventh cervical vertebra, eighth thoracic vertebra, on the humerus lateral and medial epicondyle, the angle of the acromion, the angle of the acromion jugular notch of the sternum, xiphoid process of the sternum, base of the scapular spine, inferior angle of the scapula, and midpoint between the most anterosuperior aspect of the acromioclavicular joint (Fig. 2). An experienced physiotherapist positioned the markers according to the recommendations of the international society of biomechanics (ISB) [32].
Reflective markers on the posterior of the scapula; a spinous process of the seventh cervical vertebra, b base of the scapular spine, c inferior angle of the scapula, d spinous process of the eighth thoracic vertebra, e midpoint between the most anterosuperior aspect of the acromioclavicular joint and the angle of the acromion, f the angle of the acromion, g on the humerus lateral and medial epicondyle
All data were collected at 200 Hz. Skin-based method, which inherently has some errors, was used to measure the kinematics [33].
The shoulder was guided to maintain in scapular plane at 90° of shoulder flexion, by two plastic guides while performing the tests. The test was performed in sequence of 0° maximum 120°–0° elevation every 2 s guided by a metronome (30 beats per min). Each subject performed five trials to familiarize with the test. Scapular positions at 90° and 120° of elevation were extracted during arm raising/lowering, the arc at which impingement might have occurred. Scapular angles were calculated based on the local coordinate system of the scapular relative to the local coordinate system of the thorax and protraction/retraction. The upward/downward rotation and anterior/posterior tilt were extracted using Euler sequencing [5]. These methods are aligned with the recommendations of ISB [4]. Scapular variable IR, PT MCD (1.8–1.6) and MCD value across arm angle, ranged from 2.9 to 7.7.
A difference of 4° or more in scapular kinematics was considered clinically relevant [11].
Kinematic data were analysed in sagittal and scapular planes during arm elevations. To ensure the test is performed correctly, the subject placed the arm on a flat surface while the thumb pointing to the ceiling. Three tests were performed, each in 3 s. Three complete cycles of movements were thereby completed. This procedure has been reported to be reliable in asymptomatic individuals and individuals with SIS [4, 27].
Scapular focused-exercise routine
The SFT protocol used in this research was based on previous studies. This protocol consisted of an 8-week SFT intervention (including isometric stretching, intrinsic and eccentric isotonic exercises). This training protocol includes a shoulder position training (in the first week), rotator cuff muscle strength (second, third, fifth, sixth and seventh weeks), and flexibility (fourth and eighth weeks) [7, 22]. The patients were instructed on how to perform the related exercises focusing on range of motion, strength, and function. At the week 8, they attended a one-on-one check review to ensure compliance with the exercise sheet.
Feedback intervention
The feedback intervention was conducted according to the previous studies [14, 31]. For a 15-min familiarization process, participants performed each exercise four times. During the towel Slide shoulder extension, maximum forward flexion, scapular movement in direction of the 9 o'clock, and the scapula retraction, focusing on the posterior scapula tilt was guided by the therapist using tactile and verbal feedbacks in the scapula and pre-scapular musculature. Each exercise was performed four times with a 1-min rest between each repetition while participants were looking at a monitor located 1 m away from them and at the height of 1 m from the ground. Modified Borg scale was used to assess subjective perception of the volunteer's exertion at the end of the test [3].
Statistical analysis
Statistical power calculations were conducted based on a type I error probability level of alpha = 0.05, type II error probability level of beta = 0.20, and an anticipated dropout rate of 20%, indicating 62 participants for the study [1, 14, 29].
Kolmogorov–Smirnov and Levene tests were used to assess the distribution and homogeneity of variance before performing analysis of covariance, respectively (ANCOVA).
Between-group comparisons were analyzed with a 3 × 2 analysis of variance test, including group interventions (SFT, SFTF, control) and time (baseline, or 8 wk). Furthermore, within-group comparisons were performed using 1-way analysis of variance, and Bonferroni correction was used to adjust the significance levels.
For DASH and VAS scores, intergroup comparisons were calculated using the nonparametric Kruskal–Wallis ANOVA test with multiple comparisons, and intragroup comparisons were calculated using the Friedman ANOVA test with multiple comparisons.
In addition, the effect size (Cohen´s d) was calculated to determine the difference magnitude between groups, and it was interpreted as small if d ≤ 0.5, moderate d = 0.5–0.8 and large d ˃ 0.8.
Results
The primary outcome
For pain, both the SFTF and SFT groups had significant within-group changes at 8 weeks. Also, there were significant differences between SFTF vs. SFT (mean difference = 1 ± 0.6; ES (95% CI) = − 0.3(− 0.4 to − 0.1); P = 0.04) SFTF vs. control (mean difference = − 4.5 ± 0.7; ES (95% CI) = 1.3(0.7–1.9); P = 0.01), and also SFT vs. control (mean difference = 3.5 ± 0.1; ES (95% CI) = 1.0(0.4–1.6); P = 0.01) (Table 2).
Secondary outcomes
The DASH scores significantly improved from pre- to post-intervention in both experimental groups at 8 weeks. Also, there were significant differences between SFTF vs SFT (mean difference = − 6.1 ± 0.7; ES (95% CI) = 1.8(1.1–2.4); P = 0.04), SFTF vs control (mean difference = 15.1 ± 0.9; ES (95% CI) = 4.4(3.3–5.4); P = 0.01), and also SFT vs control (mean difference = 9 ± 0.2; ES (95% CI) = 2.6(1.8–3.4); P = 0.01) (Table 3).
Table 4 shows the results of kinematics data. Comparisons between baseline and 8-week follow-up at scapular internal rotations indicated that there were no within-group differences at the sagittal and scapular plane in both experimental groups (Table 4).
Comparisons between baseline and 8-week follow-up at scapular upward rotation and tilt showed that the scapula was more upwardly rotated and posteriorly tilted in SFTF group, whereas there were no differences found in the SFT and control group. Also, there were significant differences between SFTF vs. SFT (sagittal plane, mean difference = 3.4 ± 2.6; ES (95% CI) = 1.0 (0.4–1.5); P = 0.03; or scapular plane, mean difference = 4 ± 0.5; ES (95% CI) = 1.1 (0.5–1.8); P = 0.01), SFTF vs control (sagittal plane, mean difference = 8.1 ± 3.5; ES (95% CI) = 2.3 (1.6–3.1); P = 0.01; scapular plane, mean difference = 7.5 ± 0.3; ES (95% CI) = 2.2 (1.4–2.9); P = 0.01) (Table 4).
Considering the scapular tilt, there was a significant difference between SFTF vs. control (sagittal plane, mean difference = 3.2 ± 0.5; ES (95% CI) = 0.92(0.3–1.5); P = 0.01) (Table 4).
Discussion
The most important findings of the study were the significant differences with a larger effect size between SFTF and SFT in pain, function and scapular upward rotation and tilt.
Consistent with the present research, studies reported adding visual feedback to the scapula-stabilization exercises could decrease pain and disability, and improve scapula range of motion, strength [17] and control of the movement [26] in patients with winging scapula.
It seems improving scapula kinematics (upward rotation and tilt) during SFTF (which emphasized on rotator cuff muscle strength and tight shoulder muscle flexibility) could decrease sub-acromion bursa inflammation and soft tissue impingement. Also, it is well supported that visual feedback could improve the eccentric contraction, control ability and electromyography (EMG) activity of the serratus anterior muscle [17, 31]. Although the present study did not evaluate EMG data, it may be inferred that improving kinematics (scapula upward rotation and tilt) after SFTF could result in improvement scapular muscle activities and reduce sub-acromion space.
Moreover, studies reported adding manual therapy [5] or scapular stabilization exercises [29] to a shoulder stretching and strengthening program could not enhance scapula kinematics in patients with shoulder pain. The ESs in kinematics outcomes of the present study were larger than two mentioned studies outcomes. This can be related to the SFT, emphasizing on isometric stretching, intrinsic and eccentric isotonic exercises, the kinds of the feedbacks and the time of the treatments. Finally, the research results indicated a large ESs in some kinematic outcomes (upward rotation and tilt), especially in the SFTF group. Especially, this difference between two studies in terms of clinical significance of the interventions might be associated with using feedback in this study. Using visual, patients have time to observe the exercises and movements they are performing. On the other hand, the auditory feedback provides patients with an opportunity to correct their movement by the feedback they received from an experienced supervisor.
The findings of this study indicate adding feedback to SFT protocol definitely provides more advantages to relieve pain and improve and shoulder kinematics in individuals with SIS. Adding feedbacks to SFT could clinically enhance the shoulder kinematics resulting in relieving pain and improvement in function.
Conclusion
The study confirms the effectiveness of exercise treatment to control pain and improve function in patients with SIS. Also, the results suggest a rehabilitation program integrated with feedback can be effective to reduce pain, and improve function and kinematic in patients with SIS.
Change history
27 June 2023
An Editorial Expression of Concern to this paper has been published: https://doi.org/10.1007/s00167-023-07474-0
References
Başkurt Z, Başkurt F, Gelecek N, Özkan MH (2011) The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J Back Musculoskelet Rehabil 24(3):173–179
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8(12):1153–1157
Burnetto A, Paulin E, Yamaguti W (2002) Comparação entre a escala de Borg modificada e a escala de Borg modificada análogo visual aplicadas em pacientes com dispnéia. Braz J Phys Ther 6(1):41–45
Camargo PR, Alburquerque-Sendín F, Avila MA, Haik MN, Vieira A, Salvini TF (2015) Effects of stretching and strengthening exercises, with and without manual therapy, on scapular kinematics, function, and pain in individuals with shoulder impingement: a randomized controlled trial. J Orthop Sports Phys Ther 45(12):984–997
Chu Y, Akins J, Lovalekar M, Tashman S, Lephart S, Sell T (2012) Validation of a video-based motion analysis technique in 3-D dynamic scapular kinematic measurements. J Biomech 45(14):2462–2466
Clarsen B, Bahr R, Andersson SH, Munk R, Myklebust G (2014) Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: a prospective cohort study. Br J Sports Med 48(17):1327–1333
Desjardins-Charbonneau A, Roy J-S, Dionne CE, Frémont P, MacDermid JC, Desmeules F (2015) The efficacy of manual therapy for rotator cuff tendinopathy: a systematic review and meta-analysis. J Orthop Sports Phys Ther 45(5):330–350
Diercks R, Bron C, Dorrestijn O, Meskers C, Naber R, de Ruiter T (2014) Guideline for diagnosis and treatment of subacromial pain syndrome: a multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop 85(3):314–322
Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G (2014) Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther 44(1):30–39
Fu FH, Harner CD, Klein AH (1991) Shoulder impingement syndrome. A critical review. Clin Orthop Relat Res 269:162–173
Haik MN, Alburquerque-Sendín F, Camargo PR (2014) Reliability and minimal detectable change of 3-dimensional scapular orientation in individuals with and without shoulder impingement. J Orthop Sports Phys Ther 44(5):341–349
Hawkins R, Kennedy J (1980) Impingement syndrome in athletes. Am J Sports Med 8(3):151–158
Jobe F, Bradley J (1989) The diagnosis and nonoperative treatment of shoulder injuries in athletes. Clin Sports Med 8(3):419–438
Junghyun Kim DS, Song C (2017) Visual feedback to improve the effects of scapular stabilization exercises on pain intensity, range of motion, strength, and disability in patients with shoulder impingement syndrom. Med Sci Tech 58:42–48
Kessel L, Watson M (1977) The painful arc syndrome. Clinical classification as a guide to management. J Bone Joint Surg 59(2):166–172
Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD (2013) Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘Scapular Summit’. Br J Sports Med 47(14):877–885
Kim B, Gong W, Lee S (2010) The effect of push-up plus exercise with visual biofeedback on the activity of shoulder stabilizer muscles for winged scapula. J Phys Ther Sci 22:355–358
Kraus SL (1988) TMJ disorders: management of the craniomandibular complex: Churchill Livingstone. New York, Churchill Livingstone 18:32–50
Lewis JS, Green A, Wright C (2005) Subacromial impingement syndrome: the role of posture and muscle imbalance. J Shoulder Elbow Surg 14(4):385–392
MacDermid JC, Solomon P, Prkachin K (2006) The shoulder pain and disability index demonstrates factor, construct and longitudinal validity. BMC Musculoskelet Disord 7(1):12. https://doi.org/10.1186/1471-2474-7-12
Marques AP (2014) Manual de goniometria: Editora Manole. 35. ISBN-10: 8520438970, ISBN-13: 978-8520438978
McCormack HM, David JdL, Sheather S (1988) Clinical applications of visual analogue scales: a critical review. Psychol Med 18(4):1007–1019
Michener LA, Walsworth MK, Doukas WC, Murphy KP (2009) Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil 90(11):1898–1903
Myers JB, Oyama S, Hibberd EE (2013) Scapular dysfunction in high school baseball players sustaining throwing-related upper extremity injury: a prospective study. J Shoulder Elbow Surg 22(9):1154–1159
Paine RM, Voight M (1993) The role of the scapula. J Orthop Sports Phys Ther 18(1):386–391
Roy JS, Moffet H, Hebert LJ, Lirette R (2009) Effect of motor control and strengthening exercises on shoulder function in persons with impingement syndrome: a single-subject study design. Man Ther 14:180–188
Struyf F, Nijs J, Mollekens S, Jeurissen I, Truijen S, Mottram S (2013) Scapular-focused treatment in patients with shoulder impingement syndrome: a randomized clinical trial. Clin Rheumatol 32(3):417
Sturmberg C, Marquez J, Heneghan N, Snodgrass S, van Vliet P (2013) Attentional focus of feedback and instructions in the treatment of musculoskeletal dysfunction: a systematic review. Man Ther 18(6):458–467
Turgut E, Duzgun I, Baltaci G (2017) Effects of scapular stabilization exercise training on scapular kinematics, disability, and pain in subacromial impingement: a randomized controlled trial. Arch Phys Med Rehabil 98(10):1915–1923
Van der Windt D, Koes BW, Boeke A, Devillé W, De Jong BA, Bouter LM (1996) Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract 46(410):519–523
Weon JH, Kwon OY, Cynn HS, Lee WH, Kim TH, Yi CH (2011) Real-time visual feedback can be used to activate scapular upward rotators in people with scapular winging: an experimental study. J Physiother 57(2):101–107
Wu G, Van der Helm FC, Veeger HD, Makhsous M, Van Roy P, Anglin C (2005) ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion-Part II: shoulder, elbow, wrist and hand. J Biomech 38(5):981–992
Ludewig MP, Cook MT (2000) Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther 80(3):276–291
Acknowledgments
We would like to express our deepest appreciation for valuable assistance and contribution of all the participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We confirm that there are no known conflicts of interest associated with this publication and there has been no financial support for this work that could have influenced its outcome. The researchers independently collected, analyzed, and interpreted the results and have no financial interests in the results of this study. Furthermore, dissemination of the results of this study does not constitute endorsement by the researchers or their institutional affiliations.
Ethical approval
The protocol was approved by the local ethics committee, in the Kharazmi University, Tehran, Iran.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moslehi, M., Letafatkar, A. & Miri, H. Feedback improves the scapular-focused treatment effects in patients with shoulder impingement syndrome. Knee Surg Sports Traumatol Arthrosc 29, 2281–2288 (2021). https://doi.org/10.1007/s00167-020-06178-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06178-z