Abstract
Purpose
To determine and compare the incidence of post-operative septic arthritis following revision anterior cruciate ligament reconstruction (R-ACLR) with autologous quadriceps tendon (with patellar bone block) compared to autologous hamstring tendons (semitendinosus and gracilis).
Methods
A total of 1638 isolated R-ACLR with either autologous hamstring tendons (n = 1004, 61.3%) or quadriceps tendon (n = 634; 38.7%) were performed between 2004 and 2017 and were retrospectively analysed with regard to the occurrence of post-operative septic arthritis. The technique of R-ACLR did not significantly change during the years of the study. All patients received pre-op i.v.antibiotics, but no presoaking of the grafts in vancomycin was performed in the years of the study. The individual decision of graft choice was based on graft availability, tunnel position and the presence of tunnel widening. Generally, hamstring tendons were preferred. There were no clinically relevant differences between the groups regarding gender or age. Routine follow-up examination was performed 6 weeks after the index operation (follow-up rate 96.5%), and patients unsuspicious for septic arthritis at that time were classified as non-infected.
Results
Fourteen patients with septic arthritis were identified, resulting in an overall incidence of 0.85%. There was one patient with septic arthritis in the quadriceps tendon group (incidence: 0.16%) and 13 patients in the hamstring tendons group (incidence: 1.29%), respectively. The difference was significant (p = 0.013).
Conclusion
In this series, the incidence of post-operative septic arthritis after R-ACLR was lower when quadriceps tendon graft was used compared to hamstring tendon grafts.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Septic arthritis following anterior cruciate ligament reconstruction (ACLR) is generally rare, but dramatic cases and generally inferior results with regard to functional and clinical outcome have been reported [13, 27, 33, 40]. The risk is generally higher in more complex procedures; particularly for revision ACLR (R-ACLR) an odds ratio of around 2.5 compared to primary reconstructions has been reported [23, 37]. Beside individual parameters (e.g. comorbidities, diabetes or tobacco use), it has been shown that there are differences depending on the graft used for ACLR [5, 6, 9, 11, 15, 19, 23, 24, 34, 35].
The quadriceps tendon as an alternative graft for ACLR has come into focus in recent years [8, 26, 38]. At the authors’ sports orthopaedics centre, hamstring tendons were the preferred graft for primary reconstructions. In R-ACLR either hamstrings (semitendinosus and gracilis) or quadriceps tendons (with patellar bone block) were used. Although some case series of ACLR or R-ACLR using quadriceps tendons occasionally present data on individual cases of septic arthritis, no study has exclusively focused on this issue or has compared the incidence to other graft types [7, 20, 26, 38].
Therefore, the purpose of this study was to determine and compare the incidence rate of septic arthritis following R-ACLR with either quadriceps tendon or hamstring tendons. The hypothesis was that graft choice does not make a difference in the incidence rate of this complication.
Materials and methods
The study protocol was approved by the competent research ethics board (Landesärztekammer Baden-Württemberg, Germany, F-2014-039).
Between January 2004 and January 2017, a total of 1638 R-ACLR were performed, with multi-ligament reconstructions and allografts excluded. In 634 patients (38.7%) quadriceps tendons were used, and in 1004 patients (61.3%) hamstring tendons were used, respectively. Table 1 displays demographic parameters of the two groups. From February 2017 on all grafts were soaked in vancomycin solution and were consequently not included in the study.
Medical charts of all included patients were retrospectively reviewed with focus on the occurrence of septic arthritis. At the authors’ institution, all patients undergoing R-ACLR are scheduled for follow-up examination at 6 weeks, 6 months and 12 months from the index surgery. As it is extremely unlikely that septic arthritis occurs later than 6 weeks to the index procedure, patients with unsuspicious follow-up examinations at 6 weeks or beyond were classified as non-infected [27, 43].
In patients with septic arthritis, medical records were further examined in terms of microbiological results, whether eradication was achieved, how many arthroscopic reoperations were necessary therefore and whether the graft could be retained.
Technique of R-ACLR
The technique of revision ACLR was standardized and did not significantly change over the years of the study. Surgery was performed with single-dose antibiotics 30–60 min before surgery (cephalosporins group I or II or clindamycin in cases of allergy or intolerance) in both groups. A tourniquet was used (250 mmHg). All reconstructions were performed arthroscopically with independent femoral tunnel placement.
The individual decision of graft choice was depending on graft availability, tunnel position, the presence of tunnel widening and further individual parameters. In patients with no clear advantages for a certain graft, hamstring tendons were preferred (4-stranded or 6-stranded, semitendinosus and gracilis tendon, either ipsi- or contralateral). Throughout the years of the study, these two graft types were used in comparable numbers, and therefore comparison of these subgroups of R-ACLR is possible. For instance, usually ipsilateral hamstrings were used in previous reconstruction with bone-patellar-tendon-bone (BTB) graft, contralateral in patients with previous hamstrings reconstructions. The quadriceps tendon was used in patients with no hamstrings available (e.g. after bilateral ACLR) or in patients with marginal tunnel malpositioning or tunnel widening (ipsilateral, if not available contralateral).The bone block provides a better option of slightly correcting the former malpositioning of a tunnel in terms of an offset placement within the previous tunnel, and the problem of slight tunnel widening might be overcome by bone packing. Hamstring tendons were harvested over a 2 cm oblique incision over the pes anserinus, or along previous incisions. Quadriceps tendon was harvested over a 3–4 cm incision slightly proximal to the patella and with an attached patellar bone block of approx. 20 mm in length. In patients with no autologous hamstring or quadriceps tendons available, allografts were used, but these patients were excluded from this study. No BTB grafts were used at the institution of the authors with regard to reported higher morbidity [10, 39]. If tunnel positioning or widening did not allow single-stage revision, debridement of the tunnels and filling with autograft bone from the iliac crest (until 2012) or allograft bone (from 2012) was performed. R-ACLR was then performed after 3–6 months.
Aperture fixation with interference screws was performed on the femoral side (usually biodegradable or PEEK for hamstrings, titanium for bone block fixation of the quadriceps tendon). On the tibial side, a hybrid fixation with interference screw and non-absorbable sutures fixed to a cortical button or screw was used. Preparation of the tendons was done on a graft preparation table.
Post-operative rehabilitation protocol consisted of full range of motion with a brace without limitation and partial weight bearing (10–20 kg) for 10–14 days. In patients with concomitant meniscus repair or cartilage procedures rehabilitation protocol was adapted.
Management of septic arthritis
In patients with septic arthritis arthroscopic reoperation was urgently performed. Arthroscopic irrigation and debridement (I&D) were performed with at least 10 L [37, 43]. The approach was focused on graft retention. Antibiotic therapy was started after I&D and was re-evaluated and changed if necessary depending on microbiological findings. Clinical evaluation was performed every day, and inflammatory laboratory parameters (c-reactive-protein, CRP) were obtained every other day. Another or sequential arthroscopic I&D procedures were performed if clinical or laboratory parameter deteriorated. Graft removal was only considered in graft insufficiency or loosened fixation. Patients were discharged with oral antibiotics.
Statistical analysis
Data were analysed retrospectively. Statistical analysis was performed using IBM SPSS Statistics for Windows (version 24, IBM Corp., Armonk, NY). For statistical evaluation of categorial variables, Fisher’s exact test was used. For analysis of parametric data, a two-sample student’s t test was used. All reported P values are two-tailed, with an alpha level < 0.05 considered as significant. A post hoc power calculation was performed. With an alpha of 0.05, the calculated post hoc power of this study was 71%.
Results
From the included 1638 patients, a total of 1581 attended at least one follow-up examination at 6 weeks or beyond, resulting in a follow-up rate of 96.5%. The follow-up rate did not significantly differ between the groups (n.s.).
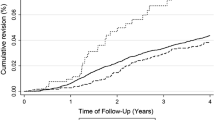
The overall incidence of septic arthritis following R-ACLR was 0.85%. There was one patient with post-operative septic arthritis in the quadriceps tendon group (incidence rate 0.16%) and 13 patients in the hamstring tendons group (incidence rate 1.29%). The difference was significant (p = 0.013).
Microbiological analyses were positive 11 of 14 patients. Coagulase-negative staphylococci (63.6%) and Staphylococcus aureus (27.3%) were most commonly detected.
Eradication could be achieved in all patients. A mean of 2.4 ± 1.4 (1–6) arthroscopic reoperations with irrigation and debridement were performed, and graft retention was possible in 13 of 14 patients (92.9%).
Discussion
The major finding of this study is that the incidence of post-operative septic arthritis in this series of R-ACLR was lower when quadriceps tendon was used compared to hamstring tendons. Therefore, the hypothesis of this study was rejected.
Septic arthritis following ACLR is generally rare, but devastating cases and generally inferior results have been reported [13, 22, 25, 33, 40]. It is generally accepted that longer operation time and more complex procedures enhance the risk of septic arthritis, particularly in ACLR compared to R-ACLR [4, 11, 15, 23]. Schuster et al. found an odds ratio of 2.5 for post-operative septic arthritis comparing revision to primary reconstructions [37]. Maletis et al. reported on very similar findings in an analysis of a large institutional ACLR registry [23]: They found deep surgical site infections in 0.3% of primary and 0.8% of revision ACLR, respectively. Arianjam et al. reported on an incidence rate of 0.6% after R-ACLR based on data of a community registry [3]. This is in line with the findings of this study, which is the largest single-centre series exclusively including R-ACLR. As it could be expected, Leroux et al. reported that the risk of infection following R-ACLR is further increased if the surgeon has a low annual volume of these procedures [21].
There are a number of studies that investigated in the incidence rate of septic arthritis depending on graft choice, but comparison is usually limited to BTB, hamstring tendon autograft and allografts (or other grafts grouped): Brophy et al. found an odds ratio of 4.6 comparing hamstring autografts to BTB autografts [9]. Maletis et al. even found an odds ratio of 8.2 for the same comparison in a registry-based study of over 10,000 primary ACLRs [24]. Judd et al. reviewed 1615 ACLR performed at their institution and identified eleven patients with infection [17]: Although half of their reconstructions were performed with BTB, all infections occurred in the hamstrings group. The present study revealed a difference between quadriceps and hamstring tendons in terms of septic complications comparable to the previously reported difference between BTB and hamstring tendons. Therefore, it might be assumed that the incidence of septice arthritis for quadriceps tendons is in the range of those for BTB, and hamstring tendons have a generally higher incidence for this complication. Even though some studies report inferior clinical results after R-ACLR with allografts, the reported incidence of septic arthritis appears comparable to BTB autografts [6, 9, 12, 24, 29].
In recent years, the quadriceps tendon has gained increasing attention for primary and particularly for revision ACLR, and reported outcomes appear comparable to the common used graft types of hamstrings, BTB and allografts [8, 16, 26]. However, so far, no studies are available presenting systematic analyses of the incidence of septic complications after ACLR with quadriceps tendon. In particular, no studies are available comparing quadriceps tendons to the aforementioned grafts in terms of the occurrence of septic complications. In clinical follow-up studies, occasionally individual cases of septic arthritis following ACLR with quadriceps tendon grafts have been reported: Akoto et al. performed a retrospective matched-pair analysis of quadriceps tendon grafts compared to hamstrings [1]. They had three patients with post-operative septic arthritis: one in the quadriceps tendon group and two in the hamstring tendons group (with 41 patients in each group). However, no conclusions can be drawn because of the overall low number of patients with infection. Slone et al. performed a review on clinical results of ACLR with quadriceps tendon [38]. Although 14 studies and more than 1100 patients were included, only one patient with a superficial infection was reported. These findings are in line with the data of the present study, with generally very low incidence of septic complications in the quadriceps group and a considerable incidence in the hamstrings group.
The reason for the differences in the incidence of septic depending on graft choice is unclear. Bacterial contamination and an environment that allows bacterial growth are necessary to cause an infection. Therefore, one reason might be the extent of graft contamination, which is likely to occur either during harvesting or preparation. No data are available for contamination of quadriceps tendons, but some studies reported graft contamination rates of BTB and hamstrings: Hantes et al. reported on graft contamination rates of 13% and 10% for BTB and hamstrings, respectively, with no difference between the groups. None of the 60 included patients in that study developed septic arthritis. Alomar et al. reported a higher rate of 22% for contamination of hamstring grafts before implantation [2]. Further, allografts have occasionally been reported to have an even lower incidence compared to autografts, which might be because of shorter surgical time and less graft manipulation [6, 18]. However, the reasons for possible differences remain still unclear. Generally, not only the graft and its susceptibility might be decisive, but also the technique of graft harvesting might substantially influence contamination rate and consequently the occurrence of septic arthritis. Although quadriceps and hamstring tendons are both harvested through small incisions trying to avoid skin contact, hamstring tendons are more likely to get into contact with the patient’s skin, especially when both semitendinosus and gracilis are harvested (as in the presented study). There might be differences in skin flora above and below knee level, which also might contribute to different graft contamination rates. However, the typical incision for BTB harvest is close to the incision for hamstring tendon harvest, and yet substantial differences in infection rates between these two graft types have been reported. Being long and thin, and being folded to a 4- or 6-stranded graft, the surface area of a hamstring tendon graft is surely higher than a BTB or quadriceps tendon graft, even if the final dimensions (length, diameter) of the grafts are similar. This might allow a higher inoculation dose resulting from skin contact or manipulation in a hamstring tendon graft. Finally, generally more manipulation is necessary in the more complex preparation of a hamstring graft (removal of muscle tissue, folding) compared to quad or BTB.
In the presented series, the incidence of septic arthritis among quadriceps tendon R-ACLR was only 0.16%. Although these were exclusively revision reconstructions with an inherent higher risk, this is even lower than it has been reported for primary ACLR with hamstring tendons, where incidence rates between 0.5 and 1.0% have been reported in large series [37, 42, 43]. It appears that quadriceps tendon has generally a lower risk for post-operative septic arthritis.
With regard to serious complications, prevention is of utmost importance. In 2012, Vertullo et al described a simple technique of soaking hamstring tendons for ACLR in vancomycin solution [41]. Using this technique, the incidence of post-operative septic arthritis was reduced to 0.0% in their series. These findings have been confirmed in several other studies [28, 31, 32]. Perez-Pietro et al. showed that the abovementioned graft contamination could be eradicated with this treatment, which might be one reason for its effectiveness [30]. Recently it has been reported that this technique is also highly effective in R-ACLR with a reduction in the incidence of septic arthritis to 0.0% regardless of the used tendon (quadriceps or hamstrings) in a series of 517 R-ACLR with vancomycin treatment compared to more than 1600 without [36]. The soaking of tendons in vancomycin solution appears safe in terms of allergies or adverse reaction; however, only limited follow-up data are available at that time [28, 41]. Generally, procedures with a high number of patients needed to be treated should be very carefully observed if its benefit outweighs potential adverse effects. For topical vancomycin treatment, this might not be fully understood to date. Clear data of incidence rates of septic arthritis in primary ACLR with quadriceps tendon are also necessary to justify the indication of vancomycin treatment. For instance, in spine surgery, similar procedures in which vancomycin powder was used topically have been reported to successfully decrease the incidence of surgical site infections, but it has been reported that the incidence of gram-negative infections increased because of selection pressure effects [14]. Therefore, further research is necessary to clearly define the significance of this procedure.
In clinical practice, the findings of this study might contribute to the individual decision of graft choice in R-ACLR. However, with regard to the generally low incidence of this complication and the promising effect of local vancomycin treatment, other factors seem more decisive in choosing the right graft for the right patient.
There are several limitations to this study that have to be considered: First, it is a comparative retrospective investigation and not a randomized controlled trial. Further, the number of affected patients is low, in particular because of the overall low incidence rate of this complication. Although the number of included patients is rather high for a single-centre series, the topic simply restricts high numbers. No more patients could have been included because from February 2017 on all cruciate ligament reconstructions were performed with soaking of the grafts in vancomycin solution. It is not possible to overcome this bias. Since the overwhelming majority of primary ACLR (> 98%) at the institution of the authors is performed with autologous hamstring tendons, comparisons of different grafts in primary reconstruction are not reasonably possible. Therefore, this analysis is limited to R-ACLR, where comparable numbers of the subgroups of different grafts are available. Further, although no clinically relevant differences are present between the two groups in terms of age or sex, it cannot be completely excluded that there are differences in terms of comorbidities, number of preceding procedures, number of preceding ACLRs or concomitant procedures. These data could not be completely obtained retrospectively. Last, it cannot be completely excluded that patients with septic arthritis were treated elsewhere. However, it would be extremely unusual that a patient is treated with this rare condition at another institution and with the presented extremely high follow-up rate this bias is minimized.
Conclusion
In this series, the incidence of post-operative septic arthritis after R-ACLR was lower when quadriceps tendon graft was used compared to hamstring tendon grafts.
References
Akoto R, Albers M, Balke M, Bouillon B, Hoher J (2019) ACL reconstruction with quadriceps tendon graft and press-fit fixation versus quadruple hamstring graft and interference screw fixation—a matched pair analysis after one year follow up. BMC Musculoskelet Disord 20:109
Alomar AZ, Alfayez SM, Somily AM (2018) Hamstring autografts are associated with a high rate of contamination in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 26:1357–1361
Arianjam A, Inacio MCS, Funahashi TT, Maletis GB (2017) Analysis of 2019 patients undergoing revision anterior cruciate ligament reconstruction from a community-based registry. Am J Sports Med 45:1574–1580
Armstrong RW, Bolding F, Joseph R (1992) Septic arthritis following arthroscopy: clinical syndromes and analysis of risk factors. Arthroscopy 8:213–223
Balato G, Di Donato SL, Ascione T, D’Addona A, Smeraglia F, Di Vico G et al (2017) Knee septic arthritis after arthroscopy: incidence, risk factors, functional outcome, and infection eradication rate. Joints 5:107–113
Bansal A, Lamplot JD, VandenBerg J, Brophy RH (2018) Meta-analysis of the risk of infections after anterior cruciate ligament reconstruction by graft type. Am J Sports Med 46:1500–1508
Barie A, Ehmann Y, Jaber A, Huber J, Streich NA (2019) Revision ACL reconstruction using quadriceps or hamstring autografts leads to similar results after 4 years: good objective stability but low rate of return to pre-injury sport level. Knee Surg Sports Traumatol Arthrosc 27:3527–3535
Belk JW, Kraeutler MJ, Marshall HA, Goodrich JA, McCarty EC (2018) Quadriceps tendon autograft for primary anterior cruciate ligament reconstruction: a systematic review of comparative studies with minimum 2-year follow-up. Arthroscopy 34:1699–1707
Brophy RH, Wright RW, Huston LJ, Nwosu SK, Spindler KP (2015) Factors associated with infection following anterior cruciate ligament reconstruction. J Bone Joint Surg Am 97:450–454
Chee MY, Chen Y, Pearce CJ, Murphy DP, Krishna L, Hui JH et al (2017) Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy 33:450–463
Clement RC, Haddix KP, Creighton RA, Spang JT, Tennant JN, Kamath GV (2016) Risk factors for infection after knee arthroscopy: analysis of 595,083 cases from 3 United States databases. Arthroscopy 32:2556–2561
Condello V, Zdanowicz U, Di Matteo B, Spalding T, Gelber PE, Adravanti P et al (2019) Allograft tendons are a safe and effective option for revision ACL reconstruction: a clinical review. Knee Surg Sports Traumatol Arthrosc 27:1771–1781
Frank M, Schmucker U, David S, Matthes G, Ekkernkamp A, Seifert J (2008) Devastating femoral osteomyelitis after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 16:71–74
Gande A, Rosinski A, Cunningham T, Bhatia N, Lee YP (2019) Selection pressures of vancomycin powder use in spine surgery: a meta-analysis. Spine J 19:1076–1084
Gowd AK, Liu JN, Bohl DD, Agarwalla A, Cabarcas BC, Manderle BJ et al (2019) Operative time as an independent and modifiable risk factor for short-term complications after knee arthroscopy. Arthroscopy 35:2089–2098
Horvath A, Senorski EH, Westin O, Karlsson J, Samuelsson K, Svantesson E (2019) Outcome after anterior cruciate ligament revision. Curr Rev Musculoskelet Med 12:397–405
Judd D, Bottoni C, Kim D, Burke M, Hooker S (2006) Infections following arthroscopic anterior cruciate ligament reconstruction. Arthroscopy 22:375–384
Katz LM, Battaglia TC, Patino P, Reichmann W, Hunter DJ, Richmond JC (2008) A retrospective comparison of the incidence of bacterial infection following anterior cruciate ligament reconstruction with autograft versus allograft. Arthroscopy 24:1330–1335
Kraeutler MJ, Bravman JT, McCarty EC (2013) Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med 41:2439–2448
Lee JK, Lee S, Lee MC (2016) Outcomes of anatomic anterior cruciate ligament reconstruction: bone-quadriceps tendon graft versus double-bundle hamstring tendon graft. Am J Sports Med 44:2323–2329
Leroux T, Wasserstein D, Dwyer T, Ogilvie-Harris DJ, Marks PH, Bach BR Jr et al (2014) The epidemiology of revision anterior cruciate ligament reconstruction in Ontario, Canada. Am J Sports Med 42:2666–2672
Makhni EC, Steinhaus ME, Mehran N, Schulz BS, Ahmad CS (2015) Functional outcome and graft retention in patients with septic arthritis after anterior cruciate ligament reconstruction: a systematic review. Arthroscopy 31:1392–1401
Maletis GB, Inacio MC, Funahashi TT (2013) Analysis of 16,192 anterior cruciate ligament reconstructions from a community-based registry. Am J Sports Med 41:2090–2098
Maletis GB, Inacio MC, Reynolds S, Desmond JL, Maletis MM, Funahashi TT (2013) Incidence of postoperative anterior cruciate ligament reconstruction infections: graft choice makes a difference. Am J Sports Med 41:1780–1785
Mester B, Ullerich F, Ohmann T, Glombitza M, Schoepp C (2017) Ankylosis of the knee after septic arthritis following anterior cruciate ligament reconstruction in a 13-year-old male. Orthop Traumatol Surg Res 103:619–622
Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E (2019) Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am J Sports Med 47:3531–3540
Mouzopoulos G, Fotopoulos VC, Tzurbakis M (2009) Septic knee arthritis following ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 17:1033–1042
Offerhaus C, Balke M, Hente J, Gehling M, Blendl S, Hoher J (2019) Vancomycin pre-soaking of the graft reduces postoperative infection rate without increasing risk of graft failure and arthrofibrosis in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27:3014–3021
Ouillette R, Edmonds E, Chambers H, Bastrom T, Pennock A (2019) Outcomes of revision anterior cruciate ligament surgery in adolescents. Am J Sports Med 47:1346–1352
Perez-Prieto D, Portillo ME, Torres-Claramunt R, Pelfort X, Hinarejos P, Monllau JC (2018) Contamination occurs during ACL graft harvesting and manipulation, but it can be easily eradicated. Knee Surg Sports Traumatol Arthrosc 26:558–562
Perez-Prieto D, Torres-Claramunt R, Gelber PE, Shehata TMA, Pelfort X, Monllau JC (2016) Autograft soaking in vancomycin reduces the risk of infection after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 24:2724–2728
Phegan M, Grayson JE, Vertullo CJ (2016) No infections in 1300 anterior cruciate ligament reconstructions with vancomycin pre-soaking of hamstring grafts. Knee Surg Sports Traumatol Arthrosc 24:2729–2735
Pogorzelski J, Themessl A, Achtnich A, Fritz EM, Wortler K, Imhoff AB et al (2018) Septic arthritis after anterior cruciate ligament reconstruction: how important is graft salvage? Am J Sports Med 46:2376–2383
Salzler MJ, Lin A, Miller CD, Herold S, Irrgang JJ, Harner CD (2014) Complications after arthroscopic knee surgery. Am J Sports Med 42:292–296
Saper M, Stephenson K, Heisey M (2014) Arthroscopic irrigation and debridement in the treatment of septic arthritis after anterior cruciate ligament reconstruction. Arthroscopy 30:747–754
Schuster P, Schlumberger M, Mayer P, Eichinger M, Geßlein M, Richter J (2019) Soaking of autografts in vancomycin is highly effective in preventing postoperative septic arthritis after revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05820-9
Schuster P, Schulz M, Immendoerfer M, Mayer P, Schlumberger M, Richter J (2015) Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: evaluation of an arthroscopic graft-retaining treatment protocol. Am J Sports Med 43:3005–3012
Slone HS, Romine SE, Premkumar A, Xerogeanes JW (2015) Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy 31:541–554
Thompson SM, Salmon LJ, Waller A, Linklater J, Roe JP, Pinczewski LA (2016) Twenty-year outcome of a longitudinal prospective evaluation of isolated endoscopic anterior cruciate ligament reconstruction with patellar tendon or hamstring autograft. Am J Sports Med 44:3083–3094
Torres-Claramunt R, Pelfort X, Erquicia J, Gil-Gonzalez S, Gelber PE, Puig L et al (2013) Knee joint infection after ACL reconstruction: prevalence, management and functional outcomes. Knee Surg Sports Traumatol Arthrosc 21:2844–2849
Vertullo CJ, Quick M, Jones A, Grayson JE (2012) A surgical technique using presoaked vancomycin hamstring grafts to decrease the risk of infection after anterior cruciate ligament reconstruction. Arthroscopy 28:337–342
Wang C, Ao Y, Wang J, Hu Y, Cui G, Yu J (2009) Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, presentation, treatment, and cause. Arthroscopy 25:243–249
Wang C, Lee YH, Siebold R (2014) Recommendations for the management of septic arthritis after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 22:2136–2144
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the competent Ethical committee.
Informed consent
No patients were contacted for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Investigation performed at the Centre for Sports Orthopedics and Special Joint Surgery, Orthopedic Hospital Markgroeningen, Germany.
Rights and permissions
About this article
Cite this article
Schuster, P., Schlumberger, M., Mayer, P. et al. Lower incidence of post-operative septic arthritis following revision anterior cruciate ligament reconstruction with quadriceps tendon compared to hamstring tendons. Knee Surg Sports Traumatol Arthrosc 28, 2572–2577 (2020). https://doi.org/10.1007/s00167-020-05878-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05878-w