Abstract
Purpose
Bone tunnel widening following anterior cruciate ligament reconstruction (ACLR) is well documented, although the aetiology and clinical significance of this phenomenon remain unclear. At mid-term follow-up, a greater prevalence of tunnel enlargement has been reported with the use of hamstring (HS) grafts. However, there are paucity of data on what happens in the longer term. The aim of this study was to assess the change in femoral and tibial tunnel dimensions 15 years after four-strand HS ACLR.
Methods
This is a retrospective review of 15 patients who underwent arthroscopic ACLR using HS autograft tendon and were followed up radiographically at 4 months, 2 years and 15 years. Suspensory fixation was used for both ends of the graft. The diameters of the bone tunnels on posteroanterior (PA) and lateral radiographs were measured using digital callipers. Repeated measures analysis of variance (ANOVA) was used to examine change in tunnel width over time.
Results
Radiographic tunnel width did not significantly change between 4 months and 2 years. However, a significant decrease in width was found for both the femoral and tibial tunnels between the 2- and 15-year follow-up (P < 0.01): the femoral tunnel decreased by 50% and 51% in the PA and lateral views, respectively; the tibial tunnel decreased by 77% and 91% in the PA and lateral views respectively. There was no significant correlation between femoral or tibial tunnel width and flexion and extension deficits or with side to side differences in anterior tibial laxity at 15 years.
Conclusions
This radiographic follow-up study of bone tunnel widening following HS ACLR with suspensory fixation demonstrated that tunnel width did not increase beyond 4 months and in fact had decreased significantly at long-term (15 years) follow-up. There was no correlation between tunnel width changes and clinical assessment of flexion and extension deficits or with side-to-side anterior knee laxity at 15-years.
Level of evidence
IV
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tibial and femoral bone tunnel widening following anterior cruciate ligament reconstruction (ACLR) is a well-known phenomenon and has been extensively documented [1, 3, 23, 25, 31]. Although the exact aetiology of tunnel widening remains unclear, it has been postulated to be the result of a combination of both biological and mechanical factors [33]. Resorbable implant degradation, synovial fluid propagation into the tunnels and inferior bone quality have all been suggested as potential biological factors [28]. In terms of mechanical factors, the type of graft fixation and graft motion within tunnels is thought to play an important role; both sagittal graft motion (‘windshield wiper effect’) and longitudinal graft motion (‘bungee cord effect’) have been reported to occur, especially with the use of suspensory fixation devices [10, 21]. The consequences of tunnel expansion are important to consider. An association has been found between tunnel enlargement and increased anterior laxity of the knee [29]. Also, in the setting of graft failure and revision ACLR, excessive tunnel widening may necessitate the use of a two-stage reconstructive approach; the initial procedure involving bone grafting of the tunnels followed by delayed reconstruction [18].
Previous research has shown greater tunnel enlargement with the use of hamstring grafts (HS) compared to bone-patellar tendon-bone grafts, particularly for the femoral bone tunnel [7, 11, 16, 32]. Tunnel widening appears to occur early and then stabilizes in the first postoperative year [6, 9, 23]. No long-term data are available. Anecdotally, there are instances of long-term follow up in which the tunnels appear to be much narrower than would have been drilled at surgery. The purpose of this study was, therefore, to examine radiographic changes in femoral and tibial tunnel enlargement 15 years after four-strand hamstring (HS) ACLR.
Materials and methods
This was a retrospective study of 15 patients (2 women, 13 men; mean age at surgery 26 ± 6 years) who underwent arthroscopic ACLR using HS autograft tendon between May 1996 and February 1998 as part of a previously reported randomised controlled trial [30]. To be included in the original trial, all participants had met the following inclusion criteria: primary unilateral ACLR, time interval between ACL injury and reconstruction more than 3 weeks and less than 12 months, no collateral ligament injury greater than grade 2 severity, no meniscal tear requiring repair, no chondral disruption greater than Noyes grade 2A. and no further surgery on the ipsilateral knee following the index ACLR surgery. The 15 patients in the current study were part of a group of 25 from the original trial who attended a 15-year follow-up. They were included in this study because they had available radiographs from each of the 4-months, 2 years and 15 years follow-up time points and had not sustained any further ACL injury (i.e. graft rupture) to the ipsilateral knee.
Surgical technique
All patients had ACLR using an arthroscopically-assisted technique performed by the same experienced knee surgeon. Gracilis and semitendinosus tendons were harvested through a small incision over the pes anserinus. A transtibial technique was used for femoral tunnel drilling, although the preferred femoral target point was identified and marked with a curette prior to tibial tunnel drilling. In current terminology, the position would be classified as high anteromedial in relation to the footprint. An oblique tibial tunnel starting at the anterior edge of the medial collateral ligament and ending in the centre of the ACL tibial footprint allowed for the desired starting point for the femoral tunnel to be reached. Femoral fixation was achieved by means of an EndoButton (Smith and Nephew Endoscopy, Mansfield, MA, USA) attached to the graft with a doubled 3-mm polyester tape. Thirty millimetres of graft was placed in the tunnel which was drilled to 37 mm and continued through the anterolateral cortex of the femur with a 4.5 mm drill. The distal ends of the HS grafts were fixed by means of an Acufex fixation post (Smith and Nephew Endoscopy) to which the two ends of a #5 Ethibond (Ethicon, Somerville, NJ, USA) whip-stitch in each tendon were tied. Graft constructs were statically pretensioned at 20 lb (89 N) for 5 min prior to insertion. All patients followed a standard accelerated rehabilitation protocol [27] which emphasized immediate restoration of full extension and quadriceps function and allowed full weight bearing as tolerated immediately post-operatively. Braces were not used.
Radiographic evaluation
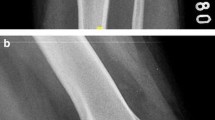
Patients were evaluated radiographically at 4 months, 2 years and 15 years post-operatively. A Rosenberg-type weight-bearing posteroanterior (PA) radiograph and a lateral radiograph with the knee in full extension were taken at each review (Siemens Fluorospot Compact, Germany). Tunnel widening was measured according to the method of L’Insalata et al. [16]. The measurements were made in both planes using digital Vernier callipers (Kincrome Australia Pty Ltd) and the inner aspect of the sclerotic bony margins of the tunnels. The widest segment of each tunnel was measured perpendicular to the long axis of the tunnel (Fig. 1). This was done independently by two observers both for the tibial and femoral measurements. All measurements were corrected for magnification—the diameter of the head of the fixation post-screw was measured to calculate the correction. Tunnel enlargement was expressed as a percentage of the diameter of the drill bit used at surgery.
Posteranterior (a) and lateral (b) knee radiographs 15 years after HS anterior cruciate ligament (ACL) reconstruction. The femoral and tibial tunnels are measured at the point of maximal tunnel width (full-line arrow). The diameter of the head of the fixation post-screw is measured (dotted-arrow) to allow correction for radiographic magnification
This study was approved by La Trobe University Human Ethics Committee—HEC application and approval number 11-083.
Statistical analysis
Statistical analysis was performed with SPSS Statistics software (Version 22 Armonk, NY: IBM Corp). Repeated measures analysis of variance (ANOVA) was used to examine change in tunnel width over time, with repeated contrasts used to examine differences between time points (4 months vs 2 years; 2 years vs 15 years). A p value of p < 0.05 was used to indicate statistical significance. Intra-class correlation coefficients were calculated to determine inter-observer reliability. Pearson correlation coefficients were calculated for femoral and tibial tunnel width changes in both planes tunnel with flexion and extension deficits and side to side differences in anterior tibial laxity at 15 years.
Results
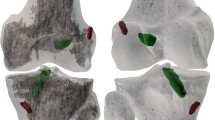
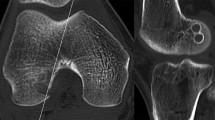
Well-defined sclerotic margins were always present for the tibial tunnel at each radiographic assessment. Two patients showed obliterated femoral tunnels, one from 4 months onwards and the other at 2 years follow-up. These patients were therefore not included in the repeated measures ANOVA model for the femoral tunnel.
For the femoral tunnel, there was a significant effect of time for both radiograph views (PA F(2.24) = 13.6, p < 0.001; Lateral F(2.24) = 9.8, p = 0.001). Post-hoc testing showed no difference in femoral tunnel width changes between the 4 month and 2 year assessments in either radiographic planes (PA, non-significant (n.s.); Lateral n.s.). However, a significant decrease in tunnel width was found between 2 and 15 years in both views (PA, p = 0.001; Lateral, p = 0.02; Table 1) (Fig. 2). Specifically, the femoral tunnel width decreased by 50% and 51% from 2 to 15 years in the PA and lateral views, respectively. The width of the femoral tunnel was found to be significantly larger compared to the drill bit used at the index surgery at 15 years (PA, p < 0.001; Lateral, p = 0.02).
For the tibial tunnel, there was also a significant effect of time for both radiograph views (PA F(2.28) = 13.1, p < 0.001; Lateral F(2.28) = 10.6, p < 0.001). Once again, post hoc testing showed no difference in tibial enlargement between the 4-month and 2-year assessments in either radiographic plane (PA, p = 0.3, Lateral, p = 0.5). However, a significant decrease in tunnel width was found between 2 and 15 years in both views (PA, p = 0.001; Lateral, p = 0.007; Table 1) (Fig. 2). Specifically, the tibial tunnel decreased by 77% and 91% in the PA and lateral views respectively. In contrast to the femoral tunnel, the width of the tibial tunnel width was not significantly different from the size of the drill bit used at the index procedure at 15 years (PA, n.s.; Lateral, n.s.)
Inter-observer reliability for the measurement of tunnel width was satisfactory. The average intra-class correlation coefficient was 0.9 (95% confidence interval 0.53–0.99).
There was no significant correlation between femoral or tibial tunnel width changes and flexion and extension deficits or with side-to-side differences in anterior tibial laxity at 15 years, with Pearson correlation coefficients ranging from 0 to 0.41.
Discussion
The main finding of this study is that following HS ACLR with suspensory fixation, tunnel widening did not occur beyond 4 months and in fact significantly decreased at 15-year follow-up. Tunnel widening was greater for the femoral tunnel than for the tibial tunnel. To the best of our knowledge, the present study is the first to describe the course of bone tunnel width changes for hamstring tendon grafts over such an extended period of time (15 years). In terms of objective clinical outcome, there was no significant correlation between femoral or tibial tunnel width and flexion and extension deficits and side to side differences in anterior tibial laxity at 15 years.
The current study is consistent with the finding of others that tunnel widening seems to occur early with stabilization in the first 1–2 years [4, 7, 11, 12, 22, 33]. Peyrache et al. reported that tunnel widening was evident at 3 months, but did not significantly change between 3 months and 2 years [22]. Clatworthy et al. also demonstrated bone tunnel widening up to 4 months, but no progression after 6 or 12 months [7]. Segawa et al. have suggested that an initial period of aggressive rehabilitation following surgery may increase the amount of graft tunnel motion before biological incorporation is complete, which may explain why tunnel widening ceases with time [26]. Jansson et al. have also reported that the presence of well-defined sclerotic margins on follow-up radiographs may indicate that the process of bone tunnel widening has ceased [14]. It is relevant to note that most studies examining tunnel widening with HS ACLR present only short- or medium-term results at a single time point. Dave et al. in a study of 54 patients using femoral suspensory fixation followed up at 5 years, reported more femoral than tibial tunnel widening [9]. The current study provides important long-term data and found that when compared to the size of the drill bit used at the index procedure, only the femoral tunnel was still significantly enlarged at 15 years postoperatively. It is therefore relevant to consider why the femoral tunnel widens more that the tibial tunnel.
Dave et al. suggested that the increased femoral tunnel widening may be linked to the orientation of the femoral tunnel which was drilled using a transtibial technique [9]. Femoral tunnels drilled using this technique are typically more vertical and longer than the tibial tunnel. Dave et al. therefore postulated that the graft in the femoral tunnel is subjected to more longitudinal motion compared to the shorter tibial tunnel which may explain some of the relative increase in tunnel widening. In the current study, all femoral tunnels were drilled using a transtibial technique and the results regarding the disproportionate enlargement of the femoral tunnel would concur with the aforementioned findings. It remains to be seen what impact the current trend of shorter femoral tunnels, drilled through an anteromedial portal, will have on long-term tunnel widening.
The impact of the method of tunnel fixation should also be considered as an important factor in tunnel widening over time. The current study used suspensory fixation on both the femoral (EndoButton) and tibial (fixation post) sides. EndoButton suspensory fixation has been shown to result in a relatively low stiffness graft construct, which has been associated with graft-tunnel motion and tunnel enlargement [5, 9, 21]. It is also relevant to point out that in the current study, the EndoButton was attached to the graft by means of a doubled 3-mm polyester tape. It has previously been demonstrated that there is less radiographic tunnel widening for both the femur and tibia when a continuous polyester loop EndoButton is used, attributed to a reduction in the bungee cord effect linked to viscoelasticity [17, 33]. Others have shown decreased femoral tunnel widening using fixation devices closer to the aperture of the tunnel, provided the interference screws used were not bioabsorbable [2, 10, 20, 24].
The choice of a fixation post for tibial fixation in the current study was due to the fact that interference screw usage for soft tissue grafts was not commonplace at the time of patient recruitment. However, in a study comparing suspensory (‘extra-cortical’) fixation with absorbable interference screw fixation, Buelow et al. demonstrated increased tunnel enlargement with interference screw fixation at 6 and 24 months [5]. This would suggest that biological factors possibly play a more important role than mechanical factors in tibial tunnel widening, especially when bioabsorbable interference screws are used. Interestingly, the use of tibial suspensory fixation has seen a resurgence in recent times with adjustable loop suspensory fixation and short graft configurations [8].
One of the limitations of this study is the small sample size. These patients were part of a previously reported randomized controlled trial [32], but not all of the patients had radiographs taken at all three time-points. However, as far as the authors are aware, this is the only study describing the course of bone tunnel enlargement over such an extended period (15 years) of time for HS ACL grafts, which have been associated with greater tunnel widening than other grafts. The 15-year clinical results of the larger study have previously been reported [32]. There has been no suggestion of any clinical effect of tunnel enlargement or implications for revision surgery. Based on current literature, tunnel widening does not appear to correlate with poor clinical outcome [9, 10, 15, 26]. The method of measuring tunnels in this study used radiographs alone. Although others have suggested using CT- or MRI-based measurements, Webster et al. reported that digital plain radiography is a satisfactory method for detecting bone tunnel enlargement following ACL reconstruction [13, 19, 30]. Because of this and the time and cost effectiveness, plain radiographs were taken at each follow-up.
Conclusion
This radiographic follow-up study of bone tunnel widening following HS ACLR with suspensory fixation demonstrated that tunnel width did not increase beyond 4 months and in fact reduced significantly at long-term (15 years) follow-up. In addition, there was no significant correlation between femoral or tibial tunnel width and flexion and extension deficits or with side to side differences in anterior tibial laxity at 15 years.
References
Asik M, Sen C, Tuncay I, Erdil M, Avci C, Taser OF (2007) The mid- to long-term results of the anterior cruciate ligament reconstruction with hamstring tendons using Transfix technique. Knee Surg Sports Traumatol Arthrosc 15:965–972
Baumfeld JA, Diduch DR, Rubino LJ, Hart JA, Miller MD, Barr MS, Hart JM (2008) Tunnel widening following anterior cruciate ligament reconstruction using hamstring autograft: a comparison between double cross-pin and suspensory graft fixation. Knee Surg Sports Traumatol Arthrosc 16:1108–1113
Buchner M, Schmeer T, Schmitt H (2007) Anterior cruciate ligament reconstruction with quadrupled semitendinosus tendon—minimum 6 year clinical and radiological follow-up. Knee 14:321–327
Buck DC, Simonian PT, Larson RV, Borrow J, Nathanson DA (2004) Timeline of tibial tunnel expansion after single-incision hamstring anterior cruciate ligament reconstruction. Arthroscopy 20:34–36
Buelow JU, Siebold R, Ellermann A (2002) A prospective evaluation of tunnel enlargement in anterior cruciate ligament reconstruction with hamstrings: extracortical versus anatomical fixation. Knee Surg Sports Traumatol Arthrosc 10:80–85
Chen CH, Chang CH, Su CI, Wang KC, Liu HT, Yu CM, Wong CB, Wang IC (2010) Arthroscopic single-bundle anterior cruciate ligament reconstruction with periosteum-enveloping hamstring tendon graft: clinical outcome at 2 to 7 years. Arthroscopy 26:907–917
Clatworthy MG, Annear P, Bulow JU, Bartlett RJ (1999) Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc 7:138–145
Colombet P, Saffarini M, Bouguennec N (2018) Clinical and functional outcomes of anterior cruciate ligament reconstruction at a minimum of 2 years using adjustable suspensory fixation in both the femur and tibia: a prospective study. Orthop J Sports Med 6:2325967118804128
Dave LY, Leong OK, Karim SA, Chong CH (2014) Tunnel enlargement 5 years after anterior cruciate ligament reconstruction: a radiographic and functional evaluation. Eur J Orthop Surg Traumatol 24:217–223
Fauno P, Kaalund S (2005) Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy 21:1337–1341
Feller JA, Webster KE (2003) A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 31:564–573
Fink C, Zapp M, Benedetto KP, Hackl W, Hoser C, Rieger M (2001) Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthroscopy 17:138–143
Ito MM, Tanaka S (2006) Evaluation of tibial bone-tunnel changes with X-ray and computed tomography after ACL reconstruction using a bone-patella tendon-bone autograft. Int Orthop 30:99–103
Jansson KA, Harilainen A, Sandelin J, Karjalainen PT, Aronen HJ, Tallroth K (1999) Bone tunnel enlargement after anterior cruciate ligament reconstruction with the hamstring autograft and endobutton fixation technique. A clinical, radiographic and magnetic resonance imaging study with 2 years follow-up. Knee Surg Sports Traumatol Arthrosc 7:290–295
Klein JP, Lintner DM, Downs D, Vavrenka K (2003) The incidence and significance of femoral tunnel widening after quadrupled hamstring anterior cruciate ligament reconstruction using femoral cross pin fixation. Arthroscopy 19:470–476
L’Insalata JC, Klatt B, Fu FH, Harner CD (1997) Tunnel expansion following anterior cruciate ligament reconstruction: a comparison of hamstring and patellar tendon autografts. Knee Surg Sports Traumatol Arthrosc 5:234–238
Lind M, Feller J, Webster KE (2009) Bone tunnel widening after anterior cruciate ligament reconstruction using EndoButton or EndoButton continuous loop. Arthroscopy 25:1275–1280
Maak TG, Voos JE, Wickiewicz TL, Warren RF (2010) Tunnel widening in revision anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 18:695–706
Marchant MH Jr, Willimon SC, Vinson E, Pietrobon R, Garrett WE, Higgins LD (2010) Comparison of plain radiography, computed tomography, and magnetic resonance imaging in the evaluation of bone tunnel widening after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18:1059–1064
Mermerkaya MU, Atay OA, Kaymaz B, Bekmez S, Karaaslan F, Doral MN (2015) Anterior cruciate ligament reconstruction using a hamstring graft: a retrospective comparison of tunnel widening upon use of two different femoral fixation methods. Knee Surg Sports Traumatol Arthrosc 23:2283–2291
Nebelung W, Becker R, Merkel M, Ropke M (1998) Bone tunnel enlargement after anterior cruciate ligament reconstruction with semitendinosus tendon using Endobutton fixation on the femoral side. Arthroscopy 14:810–815
Peyrache MD, Djian P, Christel P, Witvoet J (1996) Tibial tunnel enlargement after anterior cruciate ligament reconstruction by autogenous bone-patellar tendon-bone graft. Knee Surg Sports Traumatol Arthrosc 4:2–8
Plaweski S, Rossi J, Merloz P (2009) Anterior cruciate ligament reconstruction: assessment of the hamstring autograft femoral fixation using the EndoButton CL. Orthop Traumatol Surg Res 95:606–613
Sabat D, Kundu K, Arora S, Kumar V (2011) Tunnel widening after anterior cruciate ligament reconstruction: a prospective randomized computed tomography–based study comparing 2 different femoral fixation methods for hamstring graft. Arthroscopy 27:776–783
Sakai H, Yajima H, Hiraoka H, Fukuda A, Hayashi M, Tamai K, Saotome K (2004) The influence of tibial fixation on tunnel enlargement after hamstring tendon anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 12:364–370
Segawa H, Omori G, Tomita S, Koga Y (2001) Bone tunnel enlargement after anterior cruciate ligament reconstruction using hamstring tendons. Knee Surg Sports Traumatol Arthrosc 9:206–210
Shelbourne KD, Nitz P (1990) Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med 18:292–299
Silva A, Sampaio R, Pinto E (2010) Femoral tunnel enlargement after anatomic ACL reconstruction: a biological problem? Knee Surg Sports Traumatol Arthrosc 18:1189–1194
Webster KE, Chiu JJ, Feller JA (2005) Impact of measurement error in the analysis of bone tunnel enlargement after anterior cruciate ligament reconstruction. Am J Sports Med 33:1680–1687
Webster KE, Feller JA, Elliott J, Hutchison A, Payne R (2004) A comparison of bone tunnel measurements made using computed tomography and digital plain radiography after anterior cruciate ligament reconstruction. Arthroscopy 20:946–950
Webster KE, Feller JA, Hameister KA (2001) Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 9:86–91
Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK (2016) Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: a 15-year follow-up of a randomized controlled trial. Am J Sports Med 44:83–90
Wilson TC, Kantaras A, Atay A, Johnson DL (2004) Tunnel enlargement after anterior cruciate ligament surgery. Am J Sports Med 32:543–549
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No funding.
Ethical approval
Ethical approval was from La Trobe University Human Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Devitt, B.M., Maes, M., Feller, J.A. et al. No long-term tunnel enlargement following anterior cruciate ligament reconstruction using autograft hamstring tendon with dual suspensory fixation. Knee Surg Sports Traumatol Arthrosc 28, 2157–2162 (2020). https://doi.org/10.1007/s00167-019-05741-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05741-7