Abstract
Purpose
Stiffness is a common problem following total knee arthroplasty (TKA). Mal-rotated components have been claimed to be the major cause of pain and limited motion after TKA. The present study investigates whether intra-operative intentional malrotation of the tibial component would change in vivo kinematics. The hypothesis is excessive internal rotation of the tibial component would result in postoperative extension deficit.
Methods
Thirty-one patients were enrolled in this study. After completing bony cuts and proper soft tissue balancing, the femoral and tibial trials were impacted and fixed using small pins. Lateral radiographs were used to measure and compare intraoperative full knee extension during normal and after intentional internal rotation of the tibial component. The extension deficit angles were also compared between the posterior stabilised (PS) and cruciate retaining (CR) implants.
Results
For normal tibial component rotation, the median (interquartile range) extension deficit was 0° (4). The mean tibial trial intentional internal rotation was 21.2° (± 4.5). The median (interquartile range) extension deficit significantly increased to 6° (4) after tibial component internal rotation (p = 0.001). The use of PS spacers resulted in a significantly greater extension deficit after intentional internal rotation 9° (5) compared to that of the CR implant 1° (4) (p = 0.001).
Conclusion
Internal rotation of the tibial component in total knee arthroplasty can lead to postoperative extension deficit. This could be attributed to interference with “screw home” mechanism that requires full external rotation of the tibia on the femur. Consequently, this deficit may cause pain and knee stiffness following TKA.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stiffness is a common problem with a prevalence of 1.3–13.2% in patients after total knee arthroplasty (TKA) [10, 28]. Many preoperative, intraoperative, and postoperative factors contribute to the development of stiffness after TKA [25, 26]. Mal-rotated components are reportedly the major cause of pain and limited motion after TKA because of patellar maltracking, extension flexion gap mismatch, and altered tibiofemoral kinematics [1, 8, 15].
Previous reports showed that internal malrotation of the tibial component was observed in more than 20% of conventional TKAs [20, 23]. Panni et al. in a recent systematic review showed evidence that excessive internal rotation (>10°) of the tibial component is a major cause of pain and lower functional outcome (WOMAC scores) after TKA [24]. Further, anterior knee pain following TKA has been attributed to excessive tibial internal rotation due to increased contact stress [21] and retropatellar peak pressure [27]. Moreover, a few studies linked post-TKA stiffness to excessive internal malrotation of the tibial component [2, 3, 17]. For example, excessive internal rotation of the tibial component of 13.7° was noted in 33 out of 34 patients who developed knee stiffness following TKA [3]. However, the exact cause of stiffness is still unclear, with alteration of knee kinematics being proposed.
The “Screw-home” movement is a kinematic phenomenon that normally occurs during the last 20° of knee extension. This kinematic locking mechanism occurs when the knee joint is slightly hyperextended and is stabilised with the taut collateral and cruciate ligaments. Considering the longer length of medial femoral condyle compared to that of the lateral condyle, the tibia rotates externally about 15°, thus, achieving full knee extension [9, 16]. Consequently, any limitation of tibial external rotation on the femur could hamper knee extension, resulting in extension deficit.
The aim of this in vivo study was to investigate whether induced internal rotation of the tibial component intra-operatively would change in vivo knee kinematics. It was hypothesised that excessive internal rotation of the tibial component would result in a knee extension deficit.
The primary outcome for this study was to determine the angle of extension deficit during normal and internal malrotation of the tibial component. The secondary outcome measure was the difference in extension deficit between posterior stabilising (PS) and cruciate retaining (CR) spacers.
Materials and methods
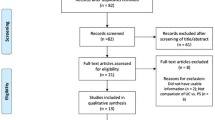
Patients scheduled for primary TKA were asked to volunteer in this study. If they agreed, the purpose and procedures of the study were fully explained, specifically the in vivo testing procedure that was expected to prolong surgery duration for 15 min. Then, informed consent was signed. The use of intraoperative imaging required additional consent. Patients with morbid obesity (BMI > 35), severe osteoporosis, and preoperative flexion contracture (> 30°) were excluded. Thirty-one patients were enrolled in this study. Table 1 demonstrates the basic characteristics of the studied sample.
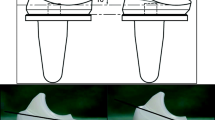
All the enrolled patients underwent TKA via the Persona Knee system (Zimmer, Inc, Warsaw, IN, USA). All surgeries were performed by the senior orthopaedic surgeons in our hospital using the measured resection technique. Initially, the femur cut was made, as recommended by the manufacturer, and the inter-epicondylar line was used to define the rotation of the femoral component. The tibial cut was made using the external guide with a 3° slope for the PS knee and 7° for the CR implant. After completing all bony cuts, the femoral trial component was impacted and fixed using small pins. The tibial component was then rotated to the proper rotation depending on the tibial landmark, which is medial third of the tibial tubercle and curvature of the tibial component itself. The tibial component in this system is asymmetrical, allowing surgeons to properly place the rotation using the curve on curve technique. The proper rotational axis of the tibial component was drawn using a marker pen. The trial component was then pinned in, and the soft tissues were balanced to ensure equal flexion and extension gap. Residual flexion deformity was corrected by removal of any posterior osteophyte and by a gradual release of the posterior capsule using a sharp curved osteotome. Patellar tracking was then tested by gradually flexing the knee and any maltracking was recorded. After all proper soft tissue alignment and balancing, lateral radiographs were taken intraoperatively to confirm full extension of the knee. Whilst imaging, the patient was positioned with the knee hanging freely and the ankle planted on a stand, without exerting any pressure on the knee, allowing only gravitational forces to determine the tension in soft tissues. The extension deficit angle was measured using the angle between two lines drawn down the mid-shafts of the femur and tibia. This method was proved to be reliable for measurement of knee joint flexion angle [14] (Fig. 1a, b).
Before cementing the implant, the provisional femur implant was kept in situ and the tibial component was intentionally malrotated. The intended new rotational axis of the tibial component was drawn using the marker pen, and the angle between the normal and malrotation axes was then measured intraoperatively. The tibial component was then fixed in the new position with pins and the same trial spacer was placed in and the knee stability and patellar tracking were re-assessed. Full extension was assessed again using proper lateral radiographs (Fig. 1b).
This present study obtained approval from the Local Institutional Ethical Committee of Burjeel Hospital for Advanced Surgery (IRB no. E10022).
Statistical analysis
Descriptive statistics: Means, standard deviation, medians, interquartile range (IQR) and percentages were calculated. Initially, data were tested for normality using the Shapiro–Wilk test. As data were not normally distributed, non-parametric Wilcoxon Signed-Rank test was used to compare the extension deficit angle within the same group. To compare the angle between PS and CR spacers, Mann–Whitney U tests were used. p value was set ≤ 0.05 throughout to declare significance. Data were analysed using SPSS version 21 (IBM Incorporation, IL, USA).
Sample size was calculated using G*Power 3 software. With a power of 80% and type I error of 5%, a minimum of 30 patients were required (α = 0.05 and β = 80%) to detect an effect size of 0.5 in the repeated measure of the median extension deficit parameters.
Results
For normal tibial component rotation, the median (IQR) extension deficit was 0° (4), whereas the median (IQR) deficit with intentional internal malrotation was 6° (4). There was a significant increase in extension deficit between the two tested positions (p = 0.001). The average amount of intentional internal malrotation of the tibial trial was 21.2° ± 4.5 (Mean ± SD).
For the PS spacers, the median (IQR) extension deficit after internal rotation was 9° (5), whereas that of the CR spacer was 1° (4). This denoted a significantly greater deficit with PS implants (p = 0.001), as shown in Table 2.
In all our patients, the patellar tracking was not affected, except for one case of valgus deformity (3.22%), where patellar lift-off was noted with internal rotation of the tibial component.
Discussion
The most significant finding of the present study was that excessive internal rotation of the tibial component results in extension deficit after TKA. Excessive internal rotation may interfere with the naturally occurring screw-home mechanism. This could be attributed to limitation of tibial external rotation, which is a prerequisite for full knee extension [9, 16]. Additionally, because of the ‘dishing’ (concave surface) of the tibial insert, excessive internal rotation of the tibial component causes the femoral component to override at the edge of the polyethylene which is normally elevated. The manufacturer’s design tolerance for rotation of the tibial component is 10° in the Persona system, i.e. any excessive rotation more than that will force the femoral component to override at the edge. Moreover, this override will cause tension in the collateral ligament and result in pain and flexion deformity.
The PS spacers were associated with a greater extension deficit than the CR spacer. This could be attributed to the flat surface geometry of the CR spacer, which may better accommodate minor rotational malalignment. Similarly, mobile bearing inserts are supposed to have a greater rotation range and, consequently, less extension deficit. On the other hand, more conforming insert designs are, therefore, expected to have a greater extension deficit with excess internal rotation of the tibial component.
Although accurate rotation of the tibial component is essential for TKA outcome, internal malrotation of the tibial component has been reported in about 20% of patients who underwent conventional primary TKA [3, 7, 18, 20, 23]. Barrack et al. [2], in a CT analysis study, reported an average 6.2° of internal rotation of the tibial component in patients with anterior knee pain following TKA, whereas pain-free patients had an average of 0.4° external rotation.
The optimal target for rotation of the tibial component is still debatable [24]. There remains a lack of consensus with regard to the best anatomical landmark to use as a reference for rotation measurement. There are many commonly used landmarks such as the medial third of the tibial tuberosity [12], the “Akagi” line [1], Cobb ‘s line [11], and “self-range-of-motion” technique [4]. The tibial tubercle is the most reproducible clinical landmark in terms of tibial tray rotation [12]. However, obtaining maximum tibial coverage may hinder proper rotation, especially when using symmetric (non- anatomic) tibial designs [19]. This challenge can be overcome using asymmetric (anatomical) tibial designs [13, 19, 22].
Extension deficit may cause pain and limited knee motion, predisposing to joint stiffness following TKA. Excessive internal rotation of the tibial component also limits knee flexion and causes its posterolateral corner to be in a more anterior position. As the posterior migration of the femoral condyle on the tibia with flexion occurs maximally in the lateral compartment, the internally rotated tibial component, especially of a conforming design, will limit flexion and rollback [3]. Kuryma et al. [17] proposed a different potential mechanism to explain postoperative stiffness based on computer simulation. In this model, excessive internal rotation of the tibial component, especially in a high-constrained geometry, increased the medial collateral ligament tension, and tibiofemoral and patellofemoral contact stresses, resulting in increased pain and stiffness.
A few studies have also reported the negative impact of internal malrotation of the tibial component on patellofemoral tracking [5]. For example, Berger and Rubash [6] reported patellar subluxation when the tibial component was internally rotated from 3° to 8°. Moreover, patellar dislocation or prosthetic failure occurred with 7° to 17° internal rotation.
The present study has a few limitations. Firstly, this study investigated the effects of internal rotation of the tibial component on limiting knee extension by hindering the ‘Screw-home’ mechanism. However, the proposed explanation does not necessarily rationalise the occurrence of extension deficit with intentional rotation of the tibial component. The significant difference between the two types of spacers (PS and CR) can partly add to our assumption. CR spacers are known to have a greater range of rotation than PS spacers in which the cam prevents this freedom. The limitation of external rotation of the tibia caused by intentional malrotation of the tibial component is less in CR spacers than in PS spacers. Hence, there is less extension deficit. A dynamic MRI study or 3D computer simulation could support this argument. Future prospective studies are, therefore, needed to fully study the kinematic effects of excessive internal rotation of the tibial component. Secondly, although the sample size was calculated and fulfilled, yet the data were not normally distributed. Re-calculation of sample size based on the reported findings is recommended to identify the optimum patient number in any future study. Third, other confounding variables that can contribute to the development of extension deficit or postoperative stiffness were not accounted for. Since different mechanisms are described for pathological effects of internal rotation of the tibial component, there is no single mechanism that is alone effective. Rather, mechanisms interact synergistically and contribute to the development of a stiff knee.
Excessive internal rotation of the tibial component has many adverse effects. It should be suspected in any case with persistent pain or stiffness after TKA.
Conclusion
Internal rotation of the tibial component during TKA can lead to postoperative knee extension deficit and, subsequently, pain and limited motion. This could be attributed to limitation of tibial component external rotation, which might hinder the ‘Screw-home’ mechanism required for full knee extension. Along with other mechanisms mentioned before, this can lead to stiffness after TKA.
References
Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C (2005) Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 436:172–176
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Bedard M, Vince KG, Redfern J, Collen SR (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469:2346–2355
Benjamin J (2006) Component alignment in total knee arthroplasty. Instr Course Lect 55:405–412
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Berger RA, Rubash HE (2001) Rotational instability and malrotation after total knee arthroplasty. Orthop Clin N Am 32(639–647):ix
Berhouet J, Beaufils P, Boisrenoult P, Frasca D, Pujol N (2011) Rotational positioning of the tibial tray in total knee arthroplasty: a CT evaluation. Orthop Traumatol Surg Res 97:699–704
Bonnin MP, Saffarini M, Mercier PE, Laurent JR, Carrillon Y (2011) Is the anterior tibial tuberosity a reliable rotational landmark for the tibial component in total knee arthroplasty? J Arthroplasty 26(260–267):e261–262
Bytyqi D, Shabani B, Lustig S, Cheze L, Karahoda Gjurgjeala N, Neyret P (2014) Gait knee kinematic alterations in medial osteoarthritis: three dimensional assessment. Int Orthop 38:1191–1198
Clement ND, Bardgett M, Weir D, Holland J, Deehan DJ (2018) Increased symptoms of stiffness 1 year after total knee arthroplasty are associated with a worse functional outcome and lower rate of patient satisfaction. Knee Surg Sports Traumatol Arthrosc 4:1196–1203
Cobb JP, Dixon H, Dandachli W, Iranpour F (2008) The anatomical tibial axis: reliable rotational orientation in knee replacement. J Bone Jt Surg Br 90:1032–1038
Coughlin KM, Incavo SJ, Churchill DL, Beynnon BD (2003) Tibial axis and patellar position relative to the femoral epicondylar axis during squatting. J Arthroplasty 18:1048–1055
Dai Y, Scuderi GR, Bischoff JE, Bertin K, Tarabichi S, Rajgopal A (2014) Anatomic tibial component design can increase tibial coverage and rotational alignment accuracy: a comparison of six contemporary designs. Knee Surg Sports Traumatol Arthrosc 22:2911–2923
Edwards JZ, Greene KA, Davis RS, Kovacik MW, Noe DA, Askew MJ (2004) Measuring flexion in knee arthroplasty patients. J Arthroplasty 19:369–372
Heyse TJ, El-Zayat BF, De Corte R, Chevalier Y, Fuchs-Winkelmann S, Labey L (2018) Internal femoral component malrotation in TKA significantly alters tibiofemoral kinematics. Knee Surg Sports Traumatol Arthrosc 26:1767–1775
Kim HY, Kim KJ, Yang DS, Jeung SW, Choi HG, Choy WS (2015) Screw-home movement of the tibiofemoral joint during normal gait: three-dimensional analysis. Clin Orthop Surg 7:303–309
Kuriyama S, Ishikawa M, Furu M, Ito H, Matsuda S (2014) Malrotated tibial component increases medial collateral ligament tension in total knee arthroplasty. J Orthop Res 32:1658–1666
Lutzner J, Krummenauer F, Gunther KP, Kirschner S (2010) Rotational alignment of the tibial component in total knee arthroplasty is better at the medial third of tibial tuberosity than at the medial border. BMC Musculoskelet Disord 11:57
Martin S, Saurez A, Ismaily S, Ashfaq K, Noble P, Incavo SJ (2014) Maximizing tibial coverage is detrimental to proper rotational alignment. Clin Orthop Relat Res 472:121–125
Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y (2001) Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg 14:152–156
Matsuda S, White SE, Williams VG 2nd, McCarthy DS, Whiteside LA (1998) Contact stress analysis in meniscal bearing total knee arthroplasty. J Arthroplasty 13:699–706
Minoda Y, Ikebuchi M, Mizokawa S, Ohta Y, Nakamura H (2018) Asymmetric tibial component improved the coverage and rotation of the tibial component in a medial pivot total knee prosthesis. J Knee Surg 31:416–421
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Jt Surg Br 92:1238–1244
Panni AS, Ascione F, Rossini M, Braile A, Corona K, Vasso M et al (2018) Tibial internal rotation negatively affects clinical outcomes in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:1636–1644
Parvizi J, Tarity TD, Steinbeck MJ, Politi RG, Joshi A, Purtill JJ et al (2006) Management of stiffness following total knee arthroplasty. J Bone Jt Surg Am 88(Suppl 4):175–181
Scuderi GR (2005) The stiff total knee arthroplasty: causality and solution. J Arthroplasty 20:23–26
Steinbruck A, Schroder C, Woiczinski M, Muller T, Muller PE, Jansson V et al (2016) Influence of tibial rotation in total knee arthroplasty on knee kinematics and retropatellar pressure: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24:2395–2401
Yercan HS, Sugun TS, Bussiere C, Ait Si Selmi T, Davies A, Neyret P (2006) Stiffness after total knee arthroplasty: prevalence, management and outcomes. Knee 13:111–117
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This present study obtained approval from the Local Institutional Ethical Committee of Burjeel Hospital for Advanced Surgery (IRB no. E10022).
Informed consent
Informed consent was obtained from patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdelnasser, M.K., Adi, M.M., Elnaggar, A.A. et al. Internal rotation of the tibial component in total knee arthroplasty can lead to extension deficit. Knee Surg Sports Traumatol Arthrosc 28, 2948–2952 (2020). https://doi.org/10.1007/s00167-019-05695-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05695-w