Abstract
Purpose
To compare tunnel widening and clinical outcome after anterior cruciate ligament reconstruction (ACLR) with interference screw fixation and all-inside reconstruction using button fixation.
Methods
Tunnel widening was assessed using tunnel volume and diameter measurements on computed tomography (CT) scans after surgery and 6 months and 2 years later, and compared between the two groups. The clinical outcome was assessed after 2 years with instrumented tibial anteroposterior translation measurements, hop testing and International Knee Documentation Committee (IKDC), Lysholm and Tegner activity scores.
Results
The study population at the final follow-up was 14 patients with screw fixation and 16 patients with button fixation. Tibial tunnels with screw fixation showed significantly larger increase in tunnel volume over time (P = 0.021) and larger tunnel diameters after 2 years in comparison with button fixation (P < 0.001). There were no significant differences in femoral tunnel volume changes over time or in tunnel diameters after 2 years. No significant differences were found in the clinical outcome scores.
Conclusions
All-inside ACLR using button fixation was associated with less tibial tunnel widening and smaller tunnels after 2 years in comparison with ACLR using screw fixation. The need for staged revision ACLRs may be greater with interference screws in comparison with button fixation at the tibial tunnel. The clinical outcomes in the two groups were comparable.
Level of evidence
II.
RCT: Consort NCT01755819.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postoperative tunnel widening is a phenomenon that has been widely reported with the use of soft-tissue grafts for anterior cruciate ligament (ACL) reconstruction [9, 12, 15, 18, 40]. Mechanical and biological factors have been postulated as causes of tunnel widening, but the phenomenon may be multifactorial. Micromovements at the tendon–bone interface have been shown to cause tunnel widening in experimental animal studies [36, 39]. Mechanical factors reported to affect tunnel widening include aggressive rehabilitation and increased graft forces due to improper graft placement [15, 42]. Biological factors include the surface area for tendon–bone healing, influx of synovial fluid into the tunnel, nonspecific inflammatory responses, cell necrosis in the graft during remodelling, immune response to allografts, toxic effects of ethylene oxide gas, cell necrosis due to drilling and foreign-body reactions [15, 17, 19, 34, 35]. Although most studies have not reported any negative associations between tunnel widening and the clinical outcome [12, 18, 40, 43], large tunnels may compromise graft fixation during revision surgery or may require two-stage surgery.
With interference screw fixation, the graft is compressed against the tunnel wall, allowing for fixation close to the joint. This may reduce graft–tunnel movement and reduce the influx of synovial fluid into the tunnel. Concerns that have been raised in relation to interference screw fixation include graft and tunnel damage during screw insertion, foreign-body reactions and poor integration of the screw [33]. Biodegradable interference screws composed of biphasic calcium phosphate and poly(l-lactide-co-d,l-lactide) PLDLA are designed to allow osseous integration and reduce postoperative tunnel widening.
With all-inside ACL reconstruction techniques, graft fixation can be achieved using adjustable-length loop cortical button devices on the femoral and tibial sides. The graft is prepared in a tendon loop with securing sutures [23]. The graft has full contact within the bone socket without any foreign material, which may allow early graft integration [37]. Concerns regarding the all-inside graft preparation and fixation technique were raised in laboratory studies that showed high graft and button loop elongation, potentially resulting in graft micromotion at the bone–tendon interface [2, 13, 27, 28, 36, 38]. Graft elongation is associated with increased knee laxity and poorer subjective knee function [7, 20]. Clinical studies reported good functional outcomes and less pain on the tibial side in comparison with conventional full tibial tunnel drilling [3, 24, 25, 32].
To date, there have been no prospective randomized trials reporting on clinical outcomes and tunnel volume changes after the all-inside ACL reconstruction technique using two adjustable-length loop cortical buttons in comparison with ACL reconstruction with interference screw fixation. The aim of the present study was therefore to compare postoperative tunnel widening and clinical outcomes after ACL reconstruction with interference screw fixation or all-inside ACL reconstruction using button fixation. The first hypothesis was that ACL reconstruction with interference screw fixation results in less postoperative tunnel widening in comparison with all-inside reconstruction using extracortical button fixation. The second hypothesis was that the two techniques would result in comparable clinical outcomes.
Materials and methods
Forty-seven patients were enrolled from 2013 to 2016 in a prospective randomized study. The patients were randomly assigned either to the ACL reconstruction technique using interference screw fixation on the femoral and tibial graft or to all-inside ACL reconstruction using adjustable-length loop cortical button fixation. Block randomization was used to assign eligible patients to the treatment arms. Patients aged 18–45 years were included if they met the following inclusion criteria: (1) unilateral ACL rupture diagnosed clinically and on magnetic resonance imaging (MRI); (2) a time interval between ACL injury and reconstruction of 1 year; (3) Tegner activity score ≥ 5; (4) a normal contralateral knee. Major exclusion criteria were total collateral ligament rupture, a full-thickness cartilage lesion and an unstable longitudinal meniscus tear (requiring meniscus refixation and changes in the postoperative rehabilitation protocol) visualized on MRI or arthroscopically (Appendix, Table 1).
Twenty-three patients were allocated to the group with screw fixation and 24 patients to the all-inside reconstruction group with button fixation. The flow diagram for the patients is shown in Fig. 1. Intraoperatively, patients were excluded because of unstable meniscus tears in four patients with screw fixation and in one patient with button fixation. Complications during surgery related to the fixation technique included one femoral screw breakage, one button mislocation in the femoral tunnel and one loop rupture of the femoral button. Three patients with button fixation sustained early repeat rupture within 6 months (one soccer, two low-energy knee distortions). One patient with button fixation presented with septic arthritis 2 weeks after surgery and was treated with two irrigations and graft retention. This patient showed ACL insufficiency at the follow-up examination after 1 year and was excluded from the final analysis. One patient with screw fixation underwent a partial medial meniscus resection 12 months after ACL reconstruction and medial meniscal repair. One patient in the button group underwent repeat surgery 18 months after ACL reconstruction for a cyclops lesion and tibial button removal.
Knee CT scans were performed within 3 days after surgery and after 6 months and 2 years postoperatively.
Surgical technique
Screw fixation
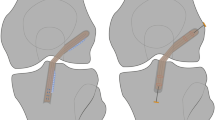
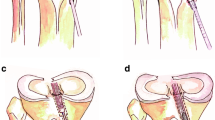
The semitendinosus and gracilis tendon were harvested. The tendon ends were whipstitched using a non-resorbable suture (FiberWire #2; Arthrex Inc., Naples, Florida, USA). A four-stranded tendon graft and graft strands were prepared. The mean graft size was 7.3 ± 0.5 mm on the femoral side and 7.9 ± 0.8 mm on the tibial side. The femoral tunnel was drilled through the anteromedial portal at the centre of the femoral ACL insertion site and the graft was fixed using a 23-mm long bioabsorbable interference screw (BioComposite; Arthrex Inc.) with a diameter 1 mm less than the tunnel diameter. A full tibial tunnel was created in the tibial ACL stump using a drill guide. The tibial ACL stump was preserved. The knee was cycled approximately 10 times for graft preconditioning. The graft was fixed at 30° of flexion by inserting the bioabsorbable interference screw (BioComposite; Arthrex Inc.) into the tibial tunnel aperture using the length scale on the screwdriver. The screw diameter selected was 1 mm larger than the tunnel diameter and the screw length was 28 mm (Fig. 2a).
Button
The semitendinosus tendon was harvested. The tendon was folded over the loop of an adjustable-length loop cortical button (TightRope RT; Arthrex Inc.) and the two tendon ends were whipstitched together using a non-resorbable suture (FiberWire #2; Arthrex Inc.). The two tendon ends were passed through another cortical button loop in order to obtain a four-stranded graft. The two graft ends were secured with two sutures (FiberWire #2; Arthrex Inc.) in a buried-knot technique as described by Lubowitz [23]. The mean length of the tendon graft was 67.2 ± 3.6 mm. The mean graft size was 7.7 ± 0.8 mm on the femoral side and 8.0 ± 0.5 mm on the tibial side. The femoral tunnel was drilled at the centre of the femoral ACL insertion area. Femoral tunnel drilling was performed using the anteromedial (AM) portal reaming technique in five patients, and with an outside-in technique using a retrograde drilling guide pin in 11 patients (FlipCutter; Arthrex Inc.). The tibial socket was created at the tibial ACL stump using a retrograde drilling guide pin (FlipCutter; Arthrex Inc.), preserving the tibial ACL stump as much as possible. A minimum of 7 mm cortical bone bridge was left. After graft insertion, the knee was cycled approximately 10 times for graft preconditioning. The graft was finally tensioned by shortening the loop of the adjustable-length loop cortical buttons on the femoral and tibial sides at 30° of flexion (Fig. 2b).
Rehabilitation
Active quadriceps exercise and passive knee motion were performed starting from the first day. Full weight-bearing was immediately allowed. A knee brace was worn for 2 weeks postoperatively. From weeks 4 to 12, cycling, muscle training and swimming were permitted. Running was allowed after 12 weeks. Full exercise activity was allowed after 6–9 months.
Clinical outcome
The clinical outcome was assessed at the 2-year follow-up appointment, with assessment of the IKDC, Lysholm and Tegner activity scores, hop testing and KT-1000 measurement. Anteroposterior knee stability after 2 years, assessed using the KT-1000 knee instrumented laxity measuring device (MEDmetric, San Diego, California, USA), was defined as the primary clinical outcome parameter.
Radiological measurements
Multidetector CT scanning (GE Discovery CT 750 HD; GE Healthcare, Chicago, Illinois, USA) was performed on the operated knee. The slice thickness was 0.625 mm (512 × 512 voxels). Images were acquired at 100 kV and 120–400 mAs, with a noise index of 25.
The bone tunnel volume was measured on the axial slices. In the group with interference screw fixation, the screw volume was included in the measurement. The cross-sectional area of the bone tunnel was added up and multiplied to calculate the total volume on every third slice (AW Server 2.0; GE Healthcare). The interrater intraclass correlation coefficient (ICC) with this measurement technique has been reported to be between 0.606 and 0.922 [30].
CT images were used for tunnel diameter measurements. The images were orientated along the longitudinal axis of the femoral and tibial tunnel. The maximum diameter of the tunnel was measured. ACL tunnel placement was measured on the sagittal slices of the postoperative CT scan. The femoral tunnel location was evaluated using the quadrant method on the lateral femoral condyle, as described by Bernard et al. [4]. The centre of the femoral tunnel was measured in the proximal–distal direction, normalized to the Blumensaat line and the dorsal–anterior location was measured as the distance from the most posterior contour of the lateral femoral condyle. The interrater ICC has been reported to be between 0.729 and 0.895 [31]. The location of the tibial tunnel was evaluated along the Amis and Jakob line (the distance from the anterior margin on the tibia to the centre of the tibial tunnel, expressed as a percentage of the anteroposterior tibial length) [1]. An ICC of 0.934 has been reported for this measurement method [16].
The study protocol was approved by the ethics committee at the Medical University of Innsbruck (ID: UN4820 316/4.22). The study was planned and conducted in accordance with the Consolidated Standards on Reporting Trials (CONSORT) guidelines (NCT01755819). All of the patients provided written informed consent prior to surgery.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corporation, Armonk, New York, USA). Parametric data are presented as mean with standard deviation (SD). The Kolmogorov–Smirnov test was used to check whether the data were normally distributed. Groups were compared using Student’s t test for normally distributed data and the Mann–Whitney U test for non-normally distributed data. Categorical data were analysed using Fisher’s exact test and expressed as absolute numbers and percentage distributions.
Changes in the absolute tunnel volume over time were compared between the two study groups using two-way analysis of variance (ANOVA) with repeated measurements. To account for possible sphericity violation among states, the P values were corrected in accordance with the Greenhouse–Geisser method [14].
Reported P values are two-sided, with significance set at < 0.05.
An effect size of 1.0 units was deemed relevant when comparing changes in tunnel widening (difference in means: 10%, SD 10%), KT-1000 (2 mm, SD 2 mm) and Lysholm score (2 points, SD 2) between the two groups. To achieve this with a power of 80% using a two-group t test with a two-sided significance level of P < 0.05, a sample size of 17 in each treatment group is required. Data for the final follow-up were available for 14 patients with screw fixation and 16 patients with button fixation, and a power of 80% was therefore not reached.
Results
There were no significant differences in the patients’ demographic characteristics in relation to age, sex, body mass index (BMI), or preinjury Tegner score. The mean operating time was significantly longer in the button group (Table 1). Early repeat rupture within 6 months was observed in three patients with button fixation.
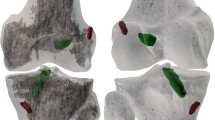
Tunnel widening
The tibial tunnel volume with button fixation was significantly smaller at all three measurement time points (P < 0.001) (Table 2). The increase in the tibial tunnel volume over time was significantly larger in the group with screw fixation (Fig. 3a) (P = 0.021).
The femoral tunnel volume with button fixation was significantly smaller at baseline in comparison with screw fixation (P = 0.025). After 6 months and 2 years, the differences between the groups were not significant (Table 2). The change in femoral tunnel volume over time did not differ significantly between the two groups (Fig. 3b).
The maximum tibial tunnel diameter was significantly larger with screw fixation at all three time points (P < 0.001). The femoral tunnel was larger with screw fixation at time point zero, but was comparable between the two groups after 6 months and 2 years (not significant) (Table 3).
In the group with button fixation, no significant differences in the femoral tunnel volume change over time were observed between the anteromedial and outside-in femoral tunnel drilling techniques (Appendix, Table 2).
Tunnel location
The tunnel location was comparable between the two groups on the tibial side (not significant). The centre of the femoral tunnel was located significantly more posteriorly with screw fixation in comparison with button fixation (P = 0.004) (Table 2). The femoral tunnel location was comparable between the anteromedial and outside-in femoral tunnel drilling techniques (not significant) (Appendix, Table 2).
Clinical outcome
At the final follow-up, 1 of 14 patients (7.1%) with screw fixation was graded C in the IKDC objective score, in comparison with 5 of 16 patients (31.3%) with button fixation (not significant). Two of 14 patients (14.3%) with screw fixation had KT laxity of more than 3 mm, in comparison with 7 of 16 patients (43.8%) with button fixation (not significant). No significant differences were found in the IKDC subjective score, Tegner activity score, or Lysholm score at the final follow-up (Table 4).
Discussion
The most important finding of this study is that all-inside ACL reconstruction using button fixation is associated with less postoperative tibial tunnel widening in comparison with interference screw fixation. The first hypothesis was rejected, as the group with button fixation showed less tunnel widening on the tibial side. The second hypothesis was partly accepted, as screw fixation showed a trend toward less knee laxity in comparison with button fixation.
The aetiology of postoperative tunnel widening is still not fully understood, but biomechanical and biological issues have been postulated. With button fixation, graft micromovements at the bone–tendon interface (bungee, windshield wiper effects) or synovial fluid migration into the tunnel might cause tunnel widening. Initial bone tunnel enlargement, bone and graft damage during insertion, allergic reactions and biological or immune responses to the foreign material are concerns with the use of biodegradable screws [9, 11, 21, 44]. In the present study, all-inside ACL reconstruction with button fixation was association with less change in the tibial tunnel volume over 2 years in comparison with screw fixation. The change in the femoral tunnel volume was comparable between the two study groups. These results are consistent with the findings of a recent study by Monaco et al. [32] that reported more tibial tunnel widening with ACL reconstruction using a tibial biodegradable interference screw and femoral cortical button fixation in comparison with all-inside ACL reconstruction with button fixation. CT measurements were performed 1 year after surgery. The authors reported a mean tibial diameter increase of 0.81 ± 0.41 mm in the middle tunnel portion and 0.79 ± 0.78 mm in the articular portion after all-inside ACL reconstruction. For tibial screw fixation, a mean tibial diameter increase of 2.42 ± 1.51 mm in the middle tunnel portion and 1.51 ± 0.81 mm in the articular portion was reported. The tunnel diameter is an important factor when one is considering single-stage or two-stage revision ACL surgery. With tunnel enlargement more than 10 mm in diameter, staged revision surgery must be considered and may be indicated at more than 12 mm [29, 41]. In the present study, significantly more patients with screw fixation had tibial tunnel diameters larger than 10 or 12 mm in comparison with button fixation. In revision surgery, larger tibial tunnels must be expected with the use of tibial interference screw fixation, and a larger proportion of patients may require bone tunnel filling. A comparable tunnel situation in terms of tunnel diameter can be expected on the femoral side after screw or button fixation. The centre of the femoral tunnel was located significantly more posteriorly with screw fixation in comparison with button fixation for both the outside-in and medial portal drilling techniques. Our explanation for this is that the femoral screw was inserted through the medial portal anteriorly to the graft. This might lead to an initial tunnel expansion at the location of least resistance in the posterior tunnel wall.
There are concerns regarding a higher graft failure rate with all-inside ACL reconstruction using adjustable-length loop cortical buttons in comparison with conventional ACL reconstruction techniques [10]. Biomechanical analyses have shown large graft elongation for all-inside ACL grafts with adjustable-length loop cortical button devices. Mayr et al. [27] used porcine tibiae and bovine extensor tendons to compare the all-inside graft preparation technique with button fixation in comparison with conventional graft preparation with a femoral button and tibial interference screw fixation. The authors reported greater graft elongation during cyclic loading with all-inside graft preparation with button fixation in comparison with the graft with tibial interference screw fixation (6.0 ± 0.6 mm vs 3.3 ± 0.8 mm). Other studies have reported overall graft elongation during cyclic loading of 5.98–6.1 mm for the all-inside graft with two adjustable-length loop cortical buttons [28, 38]. Graft elongation may result from slippage of the tendon strands at the securing sutures and from an increased distance of the fixation points when extracortical button fixation is used. Knee laxity with a side-to-side difference of more than 3 mm is a commonly used criterion for quantifying failure of ACL reconstruction [5, 41]. In the present study, knee laxity with a more than 3 mm side-to-side difference was observed in more patients with button fixation in comparison with screw fixation (2 of 14 versus 7 of 16). Despite patient randomization, the group with button fixation had higher knee laxity values preoperatively—a risk factor that has been reported for postoperative laxity of more than 3 mm [6]. Bressy et al. [8] reported a similarly high rate of residual side-to-side differences of more than 3 mm in 16 of 35 patients (46%) after all-inside ACL reconstruction using adjustable-length loop cortical button fixation on the femoral and tibial sides. In a prospective randomized study, Lubowitz et al. [24] compared all-inside ACL reconstruction with button fixation and ACL reconstruction with aperture interference screw fixation using a tibial screw placed in retrograde fashion [24]. They reported comparable scores for knee stability and clinical outcome after 2 years. In the retrospective study by Monaco et al. [32], comparable outcome and knee laxity values between ACL reconstruction using interference screw fixation or adjustable-length loop button for tibial graft fixation were reported after 2 years (KT 1000 1.7 ± 1.2 mm vs. 2.1 ± 1.2 mm).
The present study has certain limitations. The calculated sample size of 17 patients per group to achieve a power of 80% was not reached. The high rate of intraoperative drop-outs was not expected and the study must be regarded as underpowered. In addition, the study was started only shortly after the introduction of the all-inside ACL reconstruction technique in our department. Possible later improvements in the technical performance of a new technique over time (the learning curve) must therefore be regarded as a limitation of the study. The femoral tunnel reaming technique was not unique in the group with all-inside button fixation. Angulation of the femoral tunnel has been reported to affect femoral tunnel widening. Transtibial tunnel drilling has been reported to show more femoral tunnel widening in comparison with the medial portal or outside-in drilling techniques [22, 43]. However, the initial increase in femoral tunnel widening after 6 months cannot be explained by the outside-in femoral tunnel drilling, as the latter was associated with less femoral tunnel widening in this group. The tunnel location did not differ between medial portal and outside-in drilling.
Strengths of the present study include its prospective randomized trial design, with longitudinal tunnel widening volume assessment on CT scans. CT is the most accurate image modality for assessing tunnel widening after ACL reconstruction [26, 30]. The clinical relevance of this study is that ACL reconstruction with tibial button fixation results in smaller tunnels in comparison with screw fixation; this may be advantageous if revision ACL reconstruction is required.
Conclusions
All-inside ACL reconstruction using button fixation was associated with less tibial tunnel widening and smaller tunnels after 2 years in comparison with ACL reconstruction using screw fixation. There were no significant differences in the clinical outcome between the two groups.
References
Amis AA, Jakob RP (1998) Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg Sports Traumatol Arthrosc 6(Suppl 1):S2–12
Barrow AE, Pilia M, Guda T, Kadrmas WR, Burns TC (2014) Femoral suspension devices for anterior cruciate ligament reconstruction: do adjustable loops lengthen? Am J Sports Med 42:343–349
Benea H, d'Astorg H, Klouche S, Bauer T, Tomoaia G, Hardy P (2014) Pain evaluation after all-inside anterior cruciate ligament reconstruction and short term functional results of a prospective randomized study. Knee 21:102–106
Bernard M, Hertel P, Hornung H, Cierpinski T (1997) Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg 10:14–21 (discussion 21–12)
Beynnon BD, Johnson RJ, Fleming BC, Kannus P, Kaplan M, Samani J, et al. (2002) Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts. A prospective, randomized study. J Bone Joint Surg Am 84-A:1503–1513
Boutsiadis A, Panisset JC, Devitt BM, Mauris F, Barthelemy R, Barth J (2018) Anterior laxity at 2 years after anterior cruciate ligament reconstruction is comparable when using adjustable-loop suspensory fixation and interference screw fixation. Am J Sports Med 46:2366–2375
Branch TP, Stinton SK, Hutton WC, Neyret P (2017) The combination of tibial anterior translation and axial rotation into a single biomechanical factor improves the prediction of patient satisfaction over each factor alone in patients with ACL reconstructed knees. Knee Surg Sports Traumatol Arthrosc 25:1038–1047
Bressy G, Brun V, Ferrier A, Dujardin D, Oubaya N, Morel N et al (2016) Lack of stability at more than 12 months of follow-up after anterior cruciate ligament reconstruction using all-inside quadruple-stranded semitendinosus graft with adjustable cortical button fixation in both femoral and tibial sides. Orthop Traumatol Surg Res 102:867–872
Buelow JU, Siebold R, Ellermann A (2002) A prospective evaluation of tunnel enlargement in anterior cruciate ligament reconstruction with hamstrings: extracortical versus anatomical fixation. Knee Surg Sports Traumatol Arthrosc 10:80–85
Connaughton AJ, Geeslin AG, Uggen CW (2017) All-inside ACL reconstruction: how does it compare to standard ACL reconstruction techniques? J Orthop 14:241–246
Emond CE, Woelber EB, Kurd SK, Ciccotti MG, Cohen SB (2011) A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: a meta-analysis. J Bone Joint Surg Am 93:572–580
Fink C, Zapp M, Benedetto KP, Hackl W, Hoser C, Rieger M (2001) Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthroscopy 17:138–143
Glasbrenner J, Domnick C, Raschke MJ, Willinghofer T, Kittl C, Michel P, et al. (2018) Adjustable buttons for ACL graft cortical fixation partially fail with cyclic loading and unloading. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5262-2
Greenhouse SW, Geisser S (1959) On methods in the analysis of profile data. Psychometrika 24:95–112
Hoher J, Moller HD, Fu FH (1998) Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction? Knee Surg Sports Traumatol Arthrosc 6:231–240
Inderhaug E, Strand T, Fischer-Bredenbeck C, Solheim E (2014) Effect of a too posterior placement of the tibial tunnel on the outcome 10–12 years after anterior cruciate ligament reconstruction using the 70-degree tibial guide. Knee Surg Sports Traumatol Arthrosc 22:1182–1189
Jackson DW, Windler GE, Simon TM (1990) Intraarticular reaction associated with the use of freeze-dried, ethylene oxide-sterilized bone-patella tendon-bone allografts in the reconstruction of the anterior cruciate ligament. Am J Sports Med 18:1–10 (discussion 10–11)
Kawaguchi Y, Kondo E, Kitamura N, Kai S, Inoue M, Yasuda K (2011) Comparisons of femoral tunnel enlargement in 169 patients between single-bundle and anatomic double-bundle anterior cruciate ligament reconstructions with hamstring tendon grafts. Knee Surg Sports Traumatol Arthrosc 19:1249–1257
Kobayashi M, Nakagawa Y, Suzuki T, Okudaira S, Nakamura T (2006) A retrospective review of bone tunnel enlargement after anterior cruciate ligament reconstruction with hamstring tendons fixed with a metal round cannulated interference screw in the femur. Arthroscopy 22:1093–1099
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32:629–634
Konan S, Haddad FS (2009) A clinical review of bioabsorbable interference screws and their adverse effects in anterior cruciate ligament reconstruction surgery. Knee 16:6–13
Lanzetti RM, Lupariello D, De Carli A, Monaco E, Guzzini M, Fabbri M et al (2017) Can the outside-in half-tunnel technique reduce femoral tunnel widening in anterior cruciate ligament reconstruction? a CT study. Eur J Orthop Surg Traumatol 27:659–664
Lubowitz JH (2012) All-inside anterior cruciate ligament graft link: graft preparation technique. Arthrosc Tech 1:e165–168
Lubowitz JH, Schwartzberg R, Smith P (2015) Cortical suspensory button versus aperture interference screw fixation for knee anterior cruciate ligament soft-tissue allograft: a prospective, randomized controlled trial. Arthroscopy 31:1733–1739
Lubowitz JH, Schwartzberg R, Smith P (2013) Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy 29:1195–1200
Marchant MH Jr, Willimon SC, Vinson E, Pietrobon R, Garrett WE, Higgins LD (2010) Comparison of plain radiography, computed tomography, and magnetic resonance imaging in the evaluation of bone tunnel widening after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18:1059–1064
Mayr R, Heinrichs CH, Eichinger M, Coppola C, Schmoelz W, Attal R (2015) Biomechanical comparison of 2 anterior cruciate ligament graft preparation techniques for tibial fixation: adjustable-length loop cortical button or interference screw. Am J Sports Med 43:1380–1385
Mayr R, Heinrichs CH, Eichinger M, Smekal V, Schmoelz W, Attal R (2016) Preparation techniques for all-inside ACL cortical button grafts: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 24:2983–2989
Mayr R, Rosenberger R, Agraharam D, Smekal V, El Attal R (2012) Revision anterior cruciate ligament reconstruction: an update. Arch Orthop Trauma Surg 132:1299–1313
Mayr R, Smekal V, Koidl C, Coppola C, Fritz J, Rudisch A et al (2017) Tunnel widening after ACL reconstruction with aperture screw fixation or all-inside reconstruction with suspensory cortical button fixation: volumetric measurements on CT and MRI scans. Knee 24:1047–1054
Mochizuki Y, Kaneko T, Kawahara K, Toyoda S, Kono N, Hada M et al (2018) The quadrant method measuring four points is as a reliable and accurate as the quadrant method in the evaluation after anatomical double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 26:2389–2394
Monaco E, Fabbri M, Redler A, Gaj E, De Carli A, Argento G, et al. (2018) Anterior cruciate ligament reconstruction is associated with greater tibial tunnel widening when using a bioabsorbable screw compared to an all-inside technique with suspensory fixation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5275-x
Pereira H, Correlo VM, Silva-Correia J, Oliveira JM, Reis RL, Espregueira-Mendes J (2013) Migration of "bioabsorbable" screws in ACL repair. How much do we know? a systematic review. Knee Surg Sports Traumatol Arthrosc 21:986–994
Roberts TS, Drez D Jr, McCarthy W, Paine R (1991) Anterior cruciate ligament reconstruction using freeze-dried, ethylene oxide-sterilized, bone-patellar tendon-bone allografts. Two year results in thirty-six patients. Am J Sports Med 19:35–41
Rodeo SA (2018) Editorial commentary: the quest to prevent knee anterior cruciate ligament bone tunnel widening continues. Arthroscopy 34:2228–2229
Rodeo SA, Kawamura S, Kim HJ, Dynybil C, Ying L (2006) Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? Am J Sports Med 34:1790–1800
Smith PA, Stannard JP, Pfeiffer FM, Kuroki K, Bozynski CC, Cook JL (2016) Suspensory versus interference screw fixation for arthroscopic anterior cruciate ligament reconstruction in a translational large-animal model. Arthroscopy 32:1086–1097
Tiefenboeck TM, Hirtler L, Winnisch M, Joestl J, Koch T, Komjati M et al (2018) A bigger suture diameter for anterior cruciate ligament all-inside graft link preparation leads to better graft stability: An anatomical specimen study. Knee 25:427–433
Tsuda E, Fukuda Y, Loh JC, Debski RE, Fu FH, Woo SL (2002) The effect of soft-tissue graft fixation in anterior cruciate ligament reconstruction on graft-tunnel motion under anterior tibial loading. Arthroscopy 18:960–967
Webster KE, Feller JA, Hameister KA (2001) Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 9:86–91
Weiler A, Schmeling A, Stohr I, Kaab MJ, Wagner M (2007) Primary versus single-stage revision anterior cruciate ligament reconstruction using autologous hamstring tendon grafts: a prospective matched-group analysis. Am J Sports Med 35:1643–1652
Wilson TC, Kantaras A, Atay A, Johnson DL (2004) Tunnel enlargement after anterior cruciate ligament surgery. Am J Sports Med 32:543–549
Xu Y, Ao Y, Wang J, Yu J, Cui G (2011) Relation of tunnel enlargement and tunnel placement after single-bundle anterior cruciate ligament reconstruction. Arthroscopy 27:923–932
Zantop T, Weimann A, Schmidtko R, Herbort M, Raschke MJ, Petersen W (2006) Graft laceration and pullout strength of soft-tissue anterior cruciate ligament reconstruction: in vitro study comparing titanium, poly-d, l-lactide, and poly-d, l-lactide-tricalcium phosphate screws. Arthroscopy 22:1204–1210
Acknowledgements
The authors are grateful to Clemens Unterwurzacher for the illustrations.
Funding
Funding for the study was received from Arthrex Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of ineterst
The corresponding author declares that all authors listed have no conflict of interest.
Ethical approval
IRB: Ethics committee Medical University Innsbruck
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Investigation performed at the Department of Trauma Surgery, Medical University Innsbruck, Austria.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mayr, R., Smekal, V., Koidl, C. et al. ACL reconstruction with adjustable-length loop cortical button fixation results in less tibial tunnel widening compared with interference screw fixation. Knee Surg Sports Traumatol Arthrosc 28, 1036–1044 (2020). https://doi.org/10.1007/s00167-019-05642-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05642-9