Abstract
Purpose
Free quadriceps tendon autograft (QTA) has gained popularity for both primary and revision ACL reconstruction. The aim of this study is to measure the dimensions of quadriceps tendon and determine its correlation with patient’s height, weight and BMI. This is to provide a guide for patients and surgeons in predicting the suitability of QTA for ACL reconstructions.
Methods
A cross-sectional study in which the length and thickness of the quadriceps tendon was measured in 51 Caucasian patients who underwent primary total knee arthroplasty. Exclusion criteria include non-Caucasians and previous tendon pathology. Patients were selected from routine elective total knee arthroplasty list. Tendon length is taken from musculotendinous junction to its insertion. Thickness was measured at midpoint and at distal insertion. Patients’ height, weight and BMI were recorded. The correlation between patient physical parameters and tendon dimensions were determined.
Results
Subjects’ median age was 65 years (range 44–87), with 34 females and 17 males. Median length of the tendon was 9 mm (range 70–110), and median insertional thickness was 9 mm (7–10 mm). Median thickness at midpoint was 7 mm (range 4–10 mm). There was moderately positive correlation between subjects’ height and tendon length (correlation coefficient 0.50), and also between weight and tendon length (correlation coefficient 0.47). There was no significant correlation between subjects’ BMI and the tendon length. There was also no significant correlation between tendon thickness and subject’s physical parameters.
Conclusion
This study has shown that most patients could provide adequate QTA for ACL reconstruction. It also points to the fact that no investigation is required to predict the adequacy of QTA. Though further studies with larger sample size are required to confirm this, clinician can rely on analysing patients’ physical parameter in predicting the adequacy of QTA for ACL reconstruction.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autograft choice for anterior cruciate ligament (ACL) reconstruction has remained controversial with wide variations in practices worldwide [10, 30]. Proponents of different grafts put forwards different reasons for their choice with donor site morbidity, graft availability, ease of harvest, graft incorporation, size and ultimate strength, featuring on the list [11].
Bone–patellar tendon–bone (BPTB) was once considered the ‘gold standard’ due to some of its properties and level of patient satisfaction on long-term follow-up [25]. It has been credited with high ultimate load to failure strength, good size consistency, ease of harvest, with good bone to bone healing within the tibial and femoral tunnels [29]. It has a few downsides, however, with patella tendon rupture, weakness in quadriceps strength and loss of full knee extension, anterior knee pain and difficulty with kneeling reported [32, 34].
Hamstring tendon autograft (HTA) is a commonly used graft choice for ACL reconstruction [13]. It has the advantage that the complications associated with BPTB harvest can be obviated. It is also noted that a quadrupled strand of HTA has an average load to failure strength higher than that of BPTB graft (2422 N vs 1785 N) [12]. However, this is not considered clinically significant as both are stronger than native ACL which is 1730 N. The downside of HTA includes reduced strength of knee flexion, risk of injury to the sciatic or saphenous nerve with harvest, and inferior fixation strength [18, 26, 31]. It also has a relatively poorer long-term result and higher re-rupture rate compared to BPTB graft [40].
Donor site complications led to the search and use of allografts, which in turn presented their own problems of disease transmission, immunogenic reactions, slower incorporation, and higher graft failure rates [20]. Their use is, therefore, not popular. Then, synthetic grafts were considered, but these also presented barrage of problems with subsequent decline in their use [28].
The use of quadriceps tendon autograft (QTA) with or without bone plug has seen a surge in popularity in recent years, undoubtedly in effort to avoid complications and problems associated with other grafts choices above [5, 41, 42, 44, 50]. Blauth [6] introduced use of quadriceps tendon with bone plug [6], and Stäubli (1992) popularised this in 1992 [22]. Fulkerson et al. used it as a free graft in 1995 [16]. Studies show less anterior knee pain and morbidity, and comparable outcomes using free quadriceps tendon [16, 29, 46]. The role of QTA has also been highlighted in revision ACL reconstruction, paediatric population [4], and in anatomic single- or double-bundle ACL reconstruction [8].
It would be useful for surgeons and patients to know the probability of a suitable QTA harvest in a particular patient. This can be done through investigations that may or may not be invasive. This study attempts to provide this information through the analysis of simple physical patient parameters such as height, weight, BMI and sex, without relying on imaging or any invasive procedure.
Materials and methods
As this research had no bearing on the outcome or procedures being carried out, it was deemed by the Research Committee that ethical approval was not required. Further details of this consideration can be obtained from Head of Research Governance of South Warwickshire NHS Foundation Trust, United Kingdom.
This is a cross-sectional study in which the length and thickness of the quadriceps tendon was measured in 51 Caucasian patients who underwent total knee arthroplasty (TKA). Patients who met the inclusion criteria were selected from cohort of patients scheduled to have primary TKA. Inclusion criteria are follows:
-
1.
No reported or obvious previous patella or quadriceps tendon pathology. These were determined following history and examination. Patients who have had previous surgery (excluding arthroscopy for other conditions other than ligament reconstruction), or trauma that necessitated knee surgery were excluded. As such, patients with previous bone and ligament surgery around the knee were not included.
-
2.
Patients of Caucasian ethnicity. It was envisaged that over the study period, comparable number of patients of ethnicity other than Caucasians, is unlikely to be encountered, to allow reasonable generalisation to be made. In addition, more than 95% of patients that undergo ACL reconstruction in this institution are of Caucasian ethnicity.
The rational for the inclusion criteria is to eliminate possible variation in tendon parameters that may be due to ethnicity or previous tendon pathologies. This study ran over a period of 6 months. Out of the 82 patients included in the routine operating list from which patients were selected, 51 met the criteria. Eleven were excluded due to ethnicity and 20 due to previous tendon pathology or knee surgery.
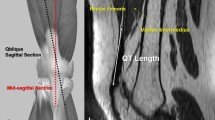
Measurements were taken intraoperatively following full exposure of the knee but before retraction and bone cuts were made. This was to avoid any effect these might have on the tendon thickness and/or length. The incision used for all TKA in the study was straight midline skin incision with medial para-patella exposure. With the knee in 45°–90° of flexion, the superior pole of the patella was identified and was located with the aid of a needle inserted in the midpoint of the tendon in the longitudinal axis. The musculotendinous junction was determined at the centre of the tendon as it begins to fade into muscle tissue. This was then marked with a sterile marker pen and the distance between the mark and needle measured with a sterile ruler. The accuracy of this measurement was to the nearest millimetre. The midpoint between the marker and needle were determined and the thickness of the tendon measured with a calliper at this point. Here, the accuracy was again to the nearest millimetre.
Patients’ height, BMI, and weight were recorded from the measurement taken during the pre-op assessment. This assessment is usually done 2–4 weeks prior to the patients’ booked operation.
The correlation between tendon parameters (length, midpoint thickness, and thickness at insertion) and these patients’ physical attributes were analysed.
Statistical analysis
Pearson’s product moment correlation coefficient was used to check the correlation between various parameters. A value between + 0.4 and + 0.6 was inferred as fair to moderately positive correlation [3]. The sample size determination has been based on previous studies [48, 51] which studied the correlation between autograft sizes and patients anthropometric parameters, with sample size of 61 and 62, respectively. It was, therefore, inferred that taking measurement across 51 patients selected from sample size of 82 patients will provide a reliable representation of the population studied.
Results
This study had 34 females and 17 males in the sample, with median age of 65 years (range 44–87). Median length of the quadriceps tendon and thickness at insertion point were both 9 mm (range 70–110, and 7–10 mm, respectively). Median thickness at midpoint was 7 mm (range 4–10 mm).
There was a moderately positive correlation between the subjects’ height and tendon length (correlation coefficient 0.50), and also between weight and tendon length (correlation coefficient 0.47). There were no significant correlations between subjects’ BMI and the tendon length, and between tendon thickness and subject’s height, weight or age.
Forty-eight out of 51 subjects had a minimum tendon length of 80 mm. Three subjects had a tendon length of 70 mm, 70 mm and 75 mm, respectively. Of note is that all three were females with height less than 160 cm. However, the number is not large enough to infer a correlation between sex and tendon length. Though, there’s a possibility that females of this height or less are more likely to have shorter tendon length.
Discussion
The most important finding of the present study is that using patient’s physical parameters alone, the probability of harvesting adequate QTA for ACL reconstruction in a patient can be predicted.
This study found that all 51 (100%) subjects had a minimum tendon length of 70 mm, and 49 out of 51 (96%) had minimum midpoint thickness of 5 mm. This shows that with the standard practice of harvesting 10 mm width of the quadriceps tendon, a graft with cross-sectional area of 10 mm × 5 mm could be harvested from 96% of the subject in this study. This will provide adequate length and thickness of graft for carrying out ACL reconstruction using standard technique [17]. Two of the subjects had midpoint thickness of 4 mm and this could not be correlated with patient’s sex, height or weight. However, given that up to 20 mm of quadriceps tendon width could be harvested with no untoward effect [14] harvesting up to 15 mm width of tendon will mean that all the subjects could provide adequate quadriceps tendon graft for ACL reconstruction. In addition, measurements in the present study were taken from the centre of the tendon, but harvesting from the lateral side of the tendon could give a longer tendon length [8].
Preoperative predication of autograft parameters is helpful for both patients and surgeons [35]. Janssen et al. correlated the length and thickness of hamstring tendon autograft (HTA) harvested during ACL reconstruction with patient height and gender and found that height was a good predictor of graft length, while male gender was associated with thicker graft [23]. Zakko et al. applied preoperative MRI to measure the sizes of frequently used grafts [51]. For the quadriceps tendon, they measured the thickness at 10, 20, and 30 mm from the insertion. They observed that there is a significant correlation between patients’ anthropometric data and the thickness of the quadriceps and patella tendons, and advised preoperative MRI measurement to obtain this information. This study points to the fact that preoperative MRI is not required once patients’ physical parameters are known.
Though it is acknowledged that the patients’ group in this study and the group of patients that usually require ACL reconstruction are different, older patients are more likely to have less bulk of tendon [21, 36]. It could, therefore, be expected that if patients within the age group of patients in this study had adequate tendon size for ACL reconstruction, younger patients will most likely have adequate size of tendon for ACL graft.
Stergios et al. also evaluated the anthropometric parameters of hamstrings with regards to their adequacy for ACL reconstruction and found that semitendinosus of adequate length was harvested in 79% of the cases [48]. Similar to findings in this study, they found moderate correlation of patient’s height and weight with the hamstring tendon length. Additionally, the mean length and thickness of the tendon in this study was similar to that reported by Schulz et al. [39]. They used bone plug free quadriceps graft for ACL reconstruction and noted that the shortest length of quadriceps tendon graft was 75 mm, whereas in this study, there were two subjects with length of 70 mm.
No correlation between tendon length and age was found in this study. However, when the correlations with subject’s height was looked at, those with tendon length 75 mm or less were shorter than 160 cm in height and were all females. In these subjects, there will be 1 in 6 probability of harvesting a free soft tissue graft of less than 80 mm. Cavaignac et al. [9] noted that harvesting from the lateral side would be preferable if greater length is desired. However, as the minimum length of tendon graft for standard technique fixation is 70 mm [16], this may not pose any additional problem particularly in primary ACL reconstructions. In addition, all the patients in this study cohort had arthritis. This is noted to be associated with shorter or contracted quadriceps tendon [20, 35], and this means that there is a good chance of harvesting graft of greater length and thickness in patients of same sex, height and weight but younger and with no arthritis or similar pathology.
It has been reported that the use of hamstring tendon autograft (HTA) and bone–patellar tendon–bone (BPTB) autograft produce equivalent clinical results [33, 37]. However, donor site morbidity has received considerable attention over the years [24, 43]. A study comparing the pain levels in immediate postoperative period between quadriceps tendon autograft (QTA) without bone block and HTA, found that use of QTA lead to less postoperative pain and less analgesic consumption [7]. Till date, there are three studies that directly compared QTA with HTA [9, 27, 45]. Cavaignac et al. [8] found that the QTA did better on the Lysholm and KOOS symptoms scores, and the negative Lachman component was higher in the QTA than in the HTA group, while there was a trend for the negative pivot shift component to be higher in the QTA group than in the HTA group. They concluded that the use of QTA graft in ACL reconstruction leads to equal or better functional outcomes than does the use of HTA, without affecting morbidity. Lee et al. [26] compared bone quadriceps tendon autograft (BQTA) with double bundle hamstring tendon graft (DBHTA) and found similar knee stability and functional outcome scores between the two. Additionally, they found that the quadriceps group had better flexor muscle strength recovery, indicating a potential advantage of BQTA in ACL reconstruction. In the above two comparative studies, similar technique of fixation was used for the two groups. Sofu et al. [44] however, found increased laxity with BQTA, but it is to be noted that they utilised two different fixation techniques for BQTA and HTA, which may have contributed to this difference.
It is known that there is regrowth of the hamstring tendon within 1 year of the primary harvest [24]; re-harvesting this with adequate graft length and strength for revision ACL reconstruction has not been reported. Re-harvesting the central patella tendon cannot be recommended due to significant clinical, radiographic and histological abnormalities 2 years after harvesting its central third [24]. In addition, revision procedures frequently require thicker graft with equivalent or greater ultimate load to failure. QTA meets these criteria [41], and has, until recently been used mainly for revision surgery [14]. In cases of revision ACL or multi-ligamentous reconstructions, the surgeon is also limited by the available autologous graft options. There is, therefore, a case to consider use of QTA as graft of choice for revision or primary ACL reconstruction where HTA or BPTB has previously been used or in limited supply. This present study, therefore, provides a guide, as well as reassurance, that if up to 20 mm width of the quadriceps tendon is taken, there is high degree of certainty that an adequate graft size will be obtained for primary and revision ACL reconstruction.
Akhtar et al. found that 58% of revision ACL reconstructions were done with BPTB and 54% with HTA usually from the opposite limb [2]. Frank et al. also concluded that given the similar outcomes and failure rates for most patients undergoing ACL revision with BPTB autograft and HTA, determining the most appropriate graft for a given patient undergoing ACL revision should be based on both patient and surgeon preferences [15]. To avoid the potential complications associated with BPTB graft while at the same time obtain a graft of similar size and strength, one could consider the QTA if patients’ physical parameter of height, weight and BMI are reassuring. In favour of QTA is also the desire to avoid double limb draping, contralateral limb pain and risks associated with HTA harvest. The finding by Häner et al. showing similar outcome using ipsilateral QTA as compared to using HTA from contralateral limb for ACL revision [19], supports this view. Once again, when patients’ parameters are reassuring, this study will guide the surgeon in choosing QTA as the graft of choice.
Some authors have claimed advantage of bone to bone integration when using BPTB autograft for ACL revision. However, a randomised control trial comparing the long-term outcomes after HTA versus BPTB autograft for revision ACL reconstruction found no significant difference in the rate of graft rupture or contralateral ACL injury in the final follow-up [49]. In addition, Runer et al. found no significant difference between patients reported outcome (PRO) 2 years after using either the QTA or HTA [38]. They, therefore, concluded that both QTA and HTA show acceptable and comparable PRO scores making the QTA a reliable graft alternative to HTA for primary/revision ACL reconstruction. There appears, therefore, no advantage of using BPTB over QTA on the ground of bone to bone fixation. But for surgeons who believe bone to bone fixation to be significantly superior, harvesting the QTA using a technique described by Kim et al. providing bone plug at each end of the QTA will meet this requirement [25].
Fulkerson and Langeland reported that the quadriceps tendon can be an effective graft sources with or without patella bone block [16]. This is particularly suitable as an alternative for primary procedures. Stäubli et al. showed that the QTA has up to 1.36 times the ultimate tensile failure load as compared to BPTB graft [47]. Though the donor site morbidity following QTA has not been extensively reported, it was observed that patients report considerable pain during the first 2 weeks, and pain during flexion for the first 4–6 weeks. In the long term, there were no local sequelae [5]. It has also been shown that harvest of a central quadriceps free tendon graft leaves a stronger extensor mechanism than harvest of a patella tendon graft [1].
This study has shown that most patients could provide adequate QTA for ACL reconstruction. It also points to the fact that no investigation is required to predict the adequacy of QTA. Though further studies with larger sample size are required to confirm this, clinician can rely on analysing patients’ physical parameter in predicting the adequacy of QTA for ACL reconstruction.
Strengths of this observational study lie in its ability to guide the surgeons in predicting the suitability of graft for ACL reconstruction without involving radiological or invasive investigational procedure.
Limitations of this study include small sample size. In addition, most patients in our cohort coming for TKA will have significant arthritis of the knee joint which may affect the quadriceps tendon properties. The patient age range in this study is different from patient age range that usually requires ACL reconstruction. However, the effects of these are likely to be positive with respect to the tendon size and suitability for ACL reconstruction in younger age group.
This study has provided a useful insight, both for patients and surgeons, on the possibility of harvesting adequate free quadriceps tendon autograft from most patients requiring ACL reconstruction—both primary and revision. Going forward, in day to day practice, surgeons and patients, who want to benefit from the advantages of free QTA for ACL reconstruction, can be reassured that with no invasive investigations, the possibility of obtaining an adequate QTA can be determined.
Conclusions
This study has provided a guide to the probability of harvesting adequate size quadriceps tendon autograft for primary and revision ACL reconstruction. In up to 96% of subjects, quadriceps tendon offered a graft of adequate length to carry out ACL reconstruction using standard technique. If intraoperative measurement of tendon thickness is taken and found to be less than 5 mm, up to 20 mm width of tendon could be harvested to give the desired size of graft for most patients. Similarly, if the length of the free graft is less than 75 mm the senior author (SEK) would recommend including patella bone plug harvest to ensure adequate fixation within the tunnels.
References
Adams DJ, Mazzocca AD, Fulkerson JP (2006) Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Arthroscopy 22:76–79
Akhtar MA, Bhattacharya R, Ohly N, Keating JF (2011) Revision ACL reconstruction—causes of failure and graft choices. Br J Sports Med 45:A15–A16
Akoglu H (2018) User’s guide to correlation coefficients. Turk J Emerg Med 18:91–93
Albright J, Lepon AK, Mayer S (2016) Anterior cruciate ligament reconstruction in pediatric and adolescent patients using quadriceps tendon autograft. Sports Med Arthrosc Rev 24:159–169
Antonogiannakis E, Yiannakopoulos CK, Hiotis I, Karabalis C, Babalis G (2005) Arthroscopic anterior cruciate ligament reconstruction using quadriceps tendon autograft and bioabsorbable cross-pin fixation. Arthroscopy 21:894
Blauth W (1984) 2-strip substitution-plasty of the anterior cruciate ligament with the quadriceps tendon. Unfallheilkunde 87:45–51
Buescu CT, Onutu AH, Lucaciu DO, Todor A (2017) Pain level after ACL reconstruction: a comparative study between free quadriceps tendon and hamstring tendons autografts. Acta Orthop Traumatol Turc 51:100–103
Caterev S, Nistor DV, Todor A (2016) Anatomic double-bundle anterior cruciate ligament reconstruction with a free quadriceps tendon autograft. Arthrosc Tech 5:e1063–e1067
Cavaignac E, Coulin B, Tscholl P, Nik Mohd Fatmy N, Duthon V, Menetrey J (2017) Is quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Am J Sports Med 45:1326–1332
Chechik O, Amar E, Khashan M, Lador R, Eyal G, Gold A (2013) An international survey on anterior cruciate ligament reconstruction practices. Int Orthop 37:201–206
Dhammi IK, Rehan-Ul-Haq KS (2015) Graft choices for anterior cruciate ligament reconstruction. Indian J Orthop 49:127–128
Dheerendra SK, Khan WS, Singhal R, Shivarathre DG, Pydisetty R, Johnstone D (2012) Anterior cruciate ligament graft choices: a review of current concepts. Open Orthop J 6:281–286
Feller JA, Webster KE (2003) A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 31:564–573
Fink C, Herbort M, Abermann E, Hoser C (2014) Minimally invasive harvest of a quadriceps tendon graft with or without a bone block. Arthrosc Tech 3:e509–e513
Frank RM, Higgins J, Bernardoni E, Cvetanovich G, Bush-Joseph CA, Verma NN, Bach BR (2017) Anterior cruciate ligament reconstruction basics: bone–patellar tendon–bone autograft harvest. Arthrosc Tech 6:e1189–e1194
Fulkerson JP, Langeland R (1995) An alternative cruciate reconstruction graft: the central quadriceps tendon. Arthrosc J Arthrosc Relat Surg 11:252–254
Gobbi A, Domzalski M, Pascual J, Zanazzo M (2005) Hamstring anterior cruciate ligament reconstruction: is it necessary to sacrifice the gracilis? Arthroscopy 21:275–280
Gobbi A, Francisco R (2005) Quadruple semitendinosus tendon for anterior cruciate ligament reconstruction. Tech Orthop 20:203–206
Häner M, Bierke S, Petersen W (2016) Anterior cruciate ligament revision surgery: ipsilateral quadriceps versus contralateral semitendinosus-gracilis autografts. Arthroscopy 32:2308–2317
Hu J, Qu J, Xu D, Zhou J, Lu H (2013) Allograft versus autograft for anterior cruciate ligament reconstruction: an up-to-date meta-analysis of prospective studies. Int Orthop 37:311–320
Ikeda S, Tsumura H, Torisu T (2005) Age-related quadriceps-dominant muscle atrophy and incident radiographic knee osteoarthritis. J Orthop Sci 10:121–126
Jakob RP, Stäubli H-U (1992) The knee and the cruciate ligaments. Springer, Berlin, pp 123–133
Janssen RPA, van der Velden MJF, van den Besselaar M, Reijman M (2017) Prediction of length and diameter of hamstring tendon autografts for knee ligament surgery in Caucasians. Knee Surg Sports Traumatol Arthrosc 25:1199–1204
Kartus J, Movin T, Karlsson J (2001) Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 17:971–980
Kim DW, Kim JO, You JD, Kim SJ, Kim HK (2001) Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon composite autograft. Arthroscopy 17:546–550
Koh HS, In Y, Kong C-G, Won H-Y, Kim K-H, Lee J-H (2010) Factors affecting patients’ graft choice in anterior cruciate ligament reconstruction. Clin Orthop Surg 2:69–75
Lee JK, Lee S, Lee MC (2016) Outcomes of anatomic anterior cruciate ligament reconstruction: bone-quadriceps tendon graft versus double-bundle hamstring tendon graft. Am J Sports Med 44:2323–2329
Legnani C, Ventura A, Terzaghi C, Borgo E, Albisetti W (2010) Anterior cruciate ligament reconstruction with synthetic grafts A review of literature. Int Orthop 34:465–471
Lund B, Nielsen T, Faunø P, Christiansen SE, Lind M (2014) Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy 30:593–598
Macaulay AA, Perfetti DC, Levine WN (2012) Anterior cruciate ligament graft choices. Sports Health 4:63–68
Makihara Y, Nishino A, Fukubayashi T, Kanamori A (2006) Decrease of knee flexion torque in patients with ACL reconstruction: combined analysis of the architecture and function of the knee flexor muscles. Knee Surg Sports Traumatol Arthrosc 14:310–317
Mickelsen PL, Morgan SJ, Johnson WA, Ferrari JD (2001) Patellar tendon rupture 3 years after anterior cruciate ligament reconstruction with a central one-third bone–patellar tendon–bone graft. Arthroscopy 17:648–652
Mohtadi NG, Chan DS, Dainty KN, Whelan DB (2011) Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 2011(9):CD005960. https://doi.org/10.1002/14651858.CD005960.pub2
Oliveira JP, Fonseca F, Noronha JC (2013) Anterior knee pain and sensitivity after anterior cruciate ligament: its impact on sports. OA Orthop 1(2):13
O’Neill DB (2004) Revision arthroscopically assisted anterior cruciate ligament reconstruction with previously unharvested ipsilateral autografts. Am J Sports Med 32:1833–1841
Petterson SC, Barrance P, Buchanan T, Binder-Macleod S, Snyder-Mackler L (2008) Mechanisms underlying quadriceps weakness in knee osteoarthritis. Med Sci Sports Exerc 40:422–427
Pinczewski LA, Deehan DJ, Salmon LJ, Russell VJ, Clingeleffer A (2002) A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 30:523–536
Runer A, Wierer G, Herbst E, Hepperger C, Herbort M, Gföller P, Hoser C, Fink C (2018) There is no difference between quadriceps- and hamstring tendon autografts in primary anterior cruciate ligament reconstruction: a 2-year patient-reported outcome study. Knee Surg Sports Traumatol Arthrosc 26:605–614
Schulz AP, Lange V, Gille J, Voigt C, Fröhlich S, Stuhr M, Jürgens C (2013) Anterior cruciate ligament reconstruction using bone plug-free quadriceps tendon autograft: intermediate-term clinical outcome after 24–36 months. Open Access J Sports Med 4:243–249
Shaerf DA, Pastides PS, Sarraf KM, Willis-Owen CA (2014) Anterior cruciate ligament reconstruction best practice: a review of graft choice. World J Orthop 5:23–29
Shani RH, Umpierez E, Nasert M, Hiza EA, Xerogeanes J (2016) Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthroscopy 32:71–75
Sheean AJ, Musahl V, Slone HS, Xerogeanes JW, Milinkovic D, Fink C, Hoser C, International Quadriceps Tendon Interest Group (2018) Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: use it now, use it often. Br J Sports Med 52:698–701
Shelton WR, Fagan BC (2011) Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 19:259–264
Slone HS, Romine SE, Premkumar A, Xerogeanes JW (2015) Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy 31:541–554
Sofu H, Sahin V, Gürsu S, Yıldırım T, Issın A, Ordueri M (2013) Use of quadriceps tendon versus hamstring tendon autograft for arthroscopic anterior cruciate ligament reconstruction: a comparative analysis of clinical results. Eklem Hastalik Cerrahisi 24:139–143
Stäubli HU, Schatzmann L, Brunner P, Rincón L, Nolte LP (1996) Quadriceps tendon and patellar ligament: cryosectional anatomy and structural properties in young adults. Knee Surg Sports Traumatol Arthrosc 4:100–110
Stäubli HU, Schatzmann L, Brunner P, Rincón L, Nolte LP (1999) Mechanical tensile properties of the quadriceps tendon and patellar ligament in young adults. Am J Sports Med 27:27–34
Stergios PG, Georgios KA, Konstantinos N, Efthymia P, Nikolaos K, Alexandros PG (2012) Adequacy of semitendinosus tendon alone for anterior cruciate ligament reconstruction graft and prediction of hamstring graft size by evaluating simple anthropometric parameters. Anat Res Int 2012:424158. https://doi.org/10.1155/2012/424158
Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK (2016) Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: a 15-year follow-up of a randomized controlled trial. Am J Sports Med 44:83–90
Xerogeanes JW, Mitchell PM, Karasev PA, Kolesov IA, Romine SE (2013) Anatomic and morphological evaluation of the quadriceps tendon using 3-dimensional magnetic resonance imaging reconstruction: applications for anterior cruciate ligament autograft choice and procurement. Am J Sports Med 41:2392–2399
Zakko P, van Eck CF, Guenther D, Irrgang JJ, Fu FH (2017) Can we predict the size of frequently used autografts in ACL reconstruction? Knee Surg Sports Traumatol Arthrosc 25:3704–3710
Funding
No external funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Ethical approval
As this research had no bearing on the outcome or procedures being carried out, it was deemed by the Research Committee that ethical approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ugwuoke, A., Syed, F. & El-Kawy, S. Predicting adequacy of free quadriceps tendon autograft, for primary and revision ACL reconstruction, from patients’ physical parameters. Knee Surg Sports Traumatol Arthrosc 28, 448–453 (2020). https://doi.org/10.1007/s00167-019-05640-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05640-x