Abstract
Purpose
The purpose was to calculate the incidence of osteoarthritis in individuals following Anterior Cruciate Ligament Reconstruction (ACLR) in a large, national database and to examine the risk factors associated with OA development.
Methods
A commercially available insurance database was queried to identify new diagnoses of knee OA in patients with ACLR. The cumulative incidence of knee OA diagnoses in patients after ACLR was calculated and stratified by time from reconstruction. Odds ratios were calculated using logistic regression to describe factors associated with a new OA diagnosis including age, sex, BMI, meniscus involvement, osteochondral graft use, and tobacco use.
Results
A total of 10,565 patients with ACLR were identified that did not have an existing diagnosis of OA, 517 of which had a documented new diagnosis of knee OA 5 years after ACL reconstruction. When stratified by follow-up time points, the incidence of a new OA diagnosis within 6 months was 2.3%; within a 1-year follow-up was 4.1%; within 2 years, follow-up was 6.2%, within 3 years, follow-up was 8.4%; within 4 years, follow-up was 10.4%; and within 5 years, follow-up was 12.3%. Risk factors for new OA diagnoses were age (OR 2.44, P < 0.001), sex (OR 1.2, P = 0.002), obesity (OR 1.4, P < 0.001), tobacco use (OR = 1.3, P = 0.001), and meniscal involvement (OR 1.2, P = 0.005).
Conclusion
Approximately 12% of patients presenting within 5 years following ACLR are diagnosed with OA. Demographic factors associated with an increased risk of a diagnosis of PTOA within 5 years after ACLR are age, sex, BMI, tobacco use, and concomitant meniscal surgery. Clinicians should be cognizant of these risk factors to develop risk profiles in patients with the common goal to achieve optimal long-term outcomes after ACLR.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) injuries are common, especially in young athletes with rates ranging from 6 to 32 injuries per 100,000 athlete exposures [23, 31]. Over 130,000 patients in the US annually elect to have anterior cruciate ligament reconstruction (ACLR) to address knee laxity with the goal of expedient return to pre-injury level of activity [10, 29]. Short-term outcomes after ACLR are oftentimes positive with reports of over 66% of patients returning to pre-injury sports within 2 years of surgery [2, 14]. In the mid-to-long term, there is compelling evidence that patients with ACLR are at increased risk for the development of post-traumatic osteoarthritis (PTOA) [25].
PTOA accounts for approximately 10% of diagnosed knee osteoarthritis (OA) leading to a U.S. economic burden of over $11 billion annually in healthcare costs [7]. Signs of joint degeneration precede patient-reported symptoms; therefore, recognition of subtle early signs of OA has been the focus of recent research. Descriptive reports of the prevalence of early onset PTOA through study visits use imaging and other evaluation modalities in patients who are not currently seeking medical care. For example, patients who are between 2 and 5 years after primary ACLR exhibit nearly a 10% joint space narrowing on weight bearing radiographs compared to healthy matched controls [40]. In addition, patients as early as 29 weeks after ACL injury show signs of cartilage breakdown prior to radiographic evidence of degenerative joint disease [8].
Prior studies and epidemiological reviews [39] have reported the incidence of diagnosed OA and PTOA in population-based studies, finding up to 40% of individuals which are diagnosed with PTOA following ACLR [32, 41]. Prior reports do not include diagnosis from symptomatic patients seeking medical care; rather patients are diagnosed through research scheduled visits. To obtain diagnostic data for the general population, large samples of healthcare data should be analyzed. Therefore, the purpose of this study was twofold: to examine a national database to calculate the incidence of osteoarthritis in individuals following ACLR and to examine the risk factors associated with OA development using a large healthcare database. Greater incidence of PTOA was hypothesized to be present the further out from ACLR and risk factors for OA diagnosis would be obesity, concomitant meniscal injuries, and cartilage restoration at the time of ACLR.
Materials and methods
Database
An insurance-based, for-fee database of patient records was utilized for the present study (PearlDiver Patient Records Database, http://www.pearldiverinc.com, Fort Wayne, IN). The PearlDiver database contains data from both Medicare and private insurers including United Healthcare (UHC) and Humana. The patients for the present study were taken from the Humana data set as it covers a younger population that would sustain ACL injuries.
The Humana data set contains procedural volumes, basic patient demographics, and laboratory data for patients with International Classification of Diseases, 9th Revision (ICD-9) diagnoses and procedures or Current Procedural Terminology (CPT) codes. The database includes patients insured from the years 2007–2015. These patients can be tracked across all locations (inpatient, outpatient, etc.) of patient care throughout the years covered by the database. In total, the database contains approximately 20 million unique patients with orthopedic diagnoses. All data from PearlDiver are de-identified and anonymous and were, thus, deemed exempt by the university’s Institutional Review Board.
Study cohort
The database was queried for patients who underwent arthroscopic ACLR (CPT 29888) between 2007 and 2015, excluding patients with a prior diagnosis of ACLR and history of any previous knee surgeries. New diagnoses of OA (ICD-9 s 715.16, 715.26, 715.36, and 715.96) were identified by excluding patients with prior OA diagnoses. Up to 7 years of longitudinal data were available through the database. The CPT and ICD-9 codes are listed in Table 1.
Incidence of post-operative OA
The outcome of interest was a new diagnosis of knee OA after ACLR. To account for patients who may be transient in the database, separate cohorts of patients were defined with certain minimums of database activity: minimum of 6 months of post-operative database activity, 1 year, 2 years, 3 years, 4 years, and 5 years. Incidences of post-operative knee OA were calculated within each group.
Risk factors
The secondary outcome was to identify patient-related and surgical risk factors for new diagnoses of knee OA after ACLR. This was accomplished by evaluating the ACL group as a whole, excluding those with prior knee OA diagnoses. The specific risk factors evaluated included: concomitant meniscectomy at time of ACLR, concomitant meniscus repair at the time of ACLR, a cartilage restoration procedure at the time of ACLR, age, sex, obesity (BMI 30–40 kg/m2), morbid obesity (BMI > 40 kg/m2), and tobacco use. CPT codes for cartilage restoration procedures can be found in Table 1.
Multiple medical co-morbidities were controlled for, including alcohol use, inflammatory arthritis, depression, hypercoagulable disorders, hyperlipidemia, hypertension, peripheral vascular disease, congestive heart failure, coronary artery disease, chronic kidney disease, chronic lung disease, chronic liver disease, hemodialysis use, and thyroid disorders.
Statistical analyses
The cumulative incidence of diagnoses of knee OA in patients after ACLR was calculated stratified by time from reconstruction. Incidence was expressed for 6 months and annually up to 5-year post-ACLR by the following equation: \({\text{OA}}\;{\text{proportion}}=~\frac{{\# \;{\text{of}}\;{\text{patients}}\;{\text{diagnosed}}\;{\text{with}}\;{\text{knee}}\;{\text{OA}}}}{{\# \;{\text{of}}\;{\text{available}}\;{\text{patients}}\;{\text{in}}\;{\text{the}}\;{\text{database}}}}\).
Odds ratios were calculated through logistic regression to describe the relative risk of OA diagnosis based on age, sex, BMI, meniscus involvement, osteochondral graft use, and tobacco use. The odds ratio is a measure of association between an exposure variable and an outcome (diagnosis of OA). An odds ratio over 1.0 indicates a greater risk of OA diagnosis when that exposure variable is present. The higher the odds ratio, the greater effect the variable has on the diagnosis of OA. An odds ratio under 1.0 represents a lower risk of OA diagnosis when exposure variable is present. Odds ratios were considered statistically significant if the associated P value was < 0.05. The p value represents the probability of the result occurring by chance.
Results
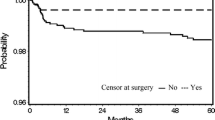
10,565 patients with ACLR without an existing diagnosis of OA were identified, 517 of which had a documented new diagnosis of knee OA after ACLR. Frequencies of sex and age for the study cohort can be found in Table 2. When stratified by follow-up time points, the incidence of a new OA diagnosis within 6 months was 2.3%; within a 1 year, follow-up was 4.1%; within 2 years, follow-up was 6.2%, within 3 years, follow-up was 8.4%; within 4 years, follow-up was 10.4%; and within 5 years, follow-up was 12.3% (Fig. 1).
Proportions of patients presenting in the healthcare system following ACLR and subsequently diagnosed with knee OA. The left axis corresponds with the bar graph indicating the number of new OA diagnoses following ACLR. The right axis corresponds with the line graph indicating the proportion of patients diagnosed with OA from the total number of patients represented in the database at that follow-up time point
Risk factors for new OA diagnoses were: age > 35 years (OR 2.44, P < 0.0001), female sex (OR 1.2, P = 0.002), obesity (OR 1.4, P = 0.0004), morbid obesity (OR 1.5, p = 0.006), tobacco use (OR 1.3, P = 0.001), partial meniscectomy (OR 1.2, P = 0.005), and meniscus repair (OR 1.3, P = 0.0004) (Table 1). History of an osteochondral graft was not significant (n.s.).
Discussion
The most important finding of the present study was that over 12% of individuals with primary ACLR are diagnosed with PTOA within 5 years of surgery, and over 2% are diagnosed with PTOA as early as 6 months. Risk factors for new diagnoses of OA were age, obesity, sex, concomitant meniscal injury, and tobacco use. In the US population, knee OA is most commonly reported in individuals between ages of 55–64 and estimated to be diagnosed in over 13% of the general population [27]. PTOA, accounting for approximately 5.6 million cases per year, is categorized as OA onset due to a precipitating incident, such as ACL injury [7]. In comparison to the previous studies that use research follow-up visits to calculate incidence of OA diagnoses, this study utilized a commercially available healthcare database to calculate the incidence of PTOA following ACLR in the general population.
ACL injuries and reconstructions are most common in young active individuals [35]; however, the findings from the current study indicate that patients with ACLR who are over 35 years of age are at highest risk for new OA diagnoses. OA diagnoses are more common later in life with highest prevalence of new OA diagnoses in the 7th decade of life [42]. Due to this study, only following patients for up to 7-year post-index surgery, it is concerning that ACLR is accelerating the process leading to a diagnosis of OA [15]. Though patients over the age of 40 have demonstrated improved outcomes, suggesting the beneficial effects of reconstruction of an injured ACL in these patients [15], degenerative articular cartilage changes from the time of ACLR has been found to be related with low overall subjective function [6]. The result of age being a risk factor for OA demonstrated in this study may suggest that surgeons consider age at time of surgery when guiding post-operative rehabilitation. Five-year incidence rates from this study support findings from a recent meta-analysis, finding 11.3% of individuals which are diagnosed with PTOA within 5-year post-ACLR [9]; however this is the first study to our knowledge to document incidence rates of OA earlier than this time point.
OA is the 11th leading cause of disability worldwide and a primary reason for reduced physical activity [13]. The risk factors for new OA diagnoses after ACLR identified in this study may or may not be modifiable. Non-modifiable risk factors for OA diagnosis were patient age and sex. Numerous studies support this finding of older patients being at greater risk for PTOA [9, 19, 34]. This study included the dichotomous variable of being younger or older than 35 years of age. Individuals over 30 years of age are likely to be diagnosed with OA within 5 years of a traumatic event to the knee, which is considerably less compared to individuals younger than 30, who are not diagnosed with OA until around 15-year post-traumatic injury [34]. PTOA presents morphologically as local cartilage damage through chondrocyte death and matrix distribution [1]. With aging, natural changes observed in a non-injured knee include structural change of type II collagen and a decreased capacity of chondrocytes to repair the damaged extracellular matrix [16]. An older individual may present with a different healing profile leading to increased rates of OA diagnoses following ACLR. Clinical findings from this study may support the biologic hypotheses that chondrocytes in an aging cartilage may be less effective in repairing articular surface damage.
Females have been reported to have a greater risk of incident OA [5]. Though the biological effect of sex on cartilage degeneration is unclear, medical providers should be aware that ACLR does not appear to modify the previously reported risk for PTOA in females. Biologic or physiologic explanations for sex-based risk for PTOA are an area for future hypothesis-based research.
Modifiable risk factors for diagnosis of OA following ACLR included BMI and smoking. BMI has been reported to be the highest predictor of OA in many populations [42], with a 35% increased risk for knee OA with a 5-point increase in BMI [22]. In the current study, obese and morbidly obese BMIs were independent risk factors for PTOA diagnoses agreeing with prior studies [18, 37]. reporting that a high body mass may increase both knee joint loading mediated by knee alignment and inflammatory responses [4] hastening the process of cartilage degeneration. Patients with ACLR should monitor BMI early after reconstruction, especially since BMI was found to be a risk factor for OA within 5 years. Research findings about the impact of tobacco use on degenerative joint disease is conflicting [5, 11]. Smoking has been reported to result in lower subjective outcomes in individuals following ACLR and in patients with knee OA [12]. Though previous studies have found smoking to decrease patient-reported outcomes and activity levels following ACLR [12, 38], the findings of the current study are the first to our knowledge to propose that tobacco use may increase the risk for PTOA following ACLR.
Surgical factors that significantly increased the risk of PTOA following ACLR were concomitant meniscal repair or meniscectomy. A meniscectomy at the time point of ACLR has been found to worsen knee symptoms [38] decrease muscle strength [36], and lead to greater risk of OA [3, 28]. In comparison, meniscal repairs at the time point of ACLR have been found to result in better subjective outcomes [30] and lower likelihood of OA development [3]. Current best practice includes repairing meniscal tears to preserve normal tibiofemoral biomechanics and loading patterns to optimize patient outcomes. The association between partial or total meniscectomy and knee OA has been well documented [17, 24]. The findings from the current study suggest that any meniscus treatment (repair or meniscectomy) is a risk factor for PTOA after ACLR.
The present study did not find any significant risk factors for cartilage restoration procedures and PTOA diagnosis. Chondral defects, such as osteochondritis dissecans and chondral lesions, have been shown to be highly predictive of OA development [21]. The non-significant finding in this study may highlight the success of osteochondral repairs accompanying ACLR; however, results may be limited to the heterogenous study cohort with different sizes and locations of chondral defects. To limit the progression of OA symptoms, results may suggest the repair of osteochondral defects at the time point of ACLR.
The incidence of OA after ACLR has been reported as high as 26% within 5 years [20]. However, these rates are often based on clinical research studies where patients are not necessarily seeking medical care and are not necessarily clinical diagnoses of OA. For example, many clinical research studies have reported OA from diagnostic X-rays from research follow-up visits [26, 33]. The current study is an analysis of diagnoses and procedures from a healthcare database. Follow-up visits under 1 year are known to be routine post-ACLR; however, the results from the current analysis beyond this time may represent actual health care utilization from patients whose symptoms are sufficient to cause them to seek medical attention. Much of the prior literature reports prevalence of OA signs in patients who may or may not exhibit OA symptoms and may or may not be independently seeking medical attention for pain or disability. Therefore, the lower rates and proportions reported in the current study are still cause for alarm—not only because of the potential impact on patient outcomes but also the short time that elapsed between ACLR surgery and a new diagnosis of OA.
Several limitations exist regarding the use of a large database. The criteria for OA diagnosis are unknown for these individuals, as incidence of OA was queried from an insurer’s database from ICD-9 codes entered by a licensed medical provider. Selection bias and potential inaccuracies of self-reporting and documentation may influence outcomes and analyses from database studies. For example, there may be inconsistency in coding for various procedures or diagnoses that may impact our results. In addition, since the database does not include actual radiographs, it is impossible to determine the severity of PTOA in this population. This database was also limited to one healthcare insurance company with the assumption that the presented rates are consistent with other healthcare providers and are a proper cross-sectional representation of the United States healthcare system. In addition, PearlDiver currently only records data from an 8-year increment. This study implemented a review of longitudinal data from 2007 to 2015. Individuals in which were identified as having ACLR may not have yet reached follow-up time points, thus, reducing incidence rates at that time period. Strengths of a commercial database study include blinding of data attainment, increasing validity, and decreasing potential bias.
Conclusion
Approximately 12% of patients presenting within 5 years following ACLR are diagnosed with OA. Demographic factors associated with an increased risk of a diagnosis of PTOA within 5 years after ACL are age, sex, BMI, tobacco use, and concomitant meniscal surgery. Clinicians should be cognizant of these risk factors to develop risk profiles in patients with the common goal to achieve optimal long-term outcomes after ACLR.
References
Anderson DD, Chubinskaya S, Guilak F, Martin JA, Oegema TR, Olson SA et al (2011) Post-traumatic osteoarthritis: improved understanding and opportunities for early intervention. J Orthop Res 29:802–809
Ardern CL, Webster KE, Taylor NF, Feller JA (2011) Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med 45:596–606
Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K (2014) Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med 42:1049–1057
Berenbaum F, Eymard F, Houard X (2013) Osteoarthritis, inflammation and obesity. Curr Opin Rheumatol 25:114–118
Blagojevic M, Jinks C, Jeffery A, Jordan KP (2010) Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthr Cartil 18:24–33
Blyth MJG, Gosal HS, Peake WM, Bartlett RJ (2003) Anterior cruciate ligament reconstruction in patients over the age of 50 years: 2- to 8-year follow-up. Knee Surg Sports Traumatol Arthrosc 11:204–211
Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA (2006) Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma 20:739–744
Chockalingam PS, Glasson SS, Lohmander LS (2013) Tenascin-C levels in synovial fluid are elevated after injury to the human and canine joint and correlate with markers of inflammation and matrix degradation. Osteoarthr Cartil 21:339–345
Cinque ME, Dornan GJ, Chahla J, Moatshe G, LaPrade RF (2017) High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients. Am J Sports Med 46(8):2011– 2019
Collins JE, Katz JN, Donnell-Fink LA, Martin SD, Losina E (2013) Cumulative incidence of ACL reconstruction after ACL injury in adults role of age, sex, and race. Am J Sports Med 41:544–549
Cooper C, Inskip H, Croft P, Campbell L, Smith G, McLaren M et al (1998) Individual risk factors for hip osteoarthritis: obesity, hip injury and physical activity. Am J Epidemiol 147:516–522
Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD et al (2014) Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med 42:1058–1067
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M et al (2014) The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73:1323–1330
Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC (2017) Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg 99:897–904
Desai N, Bjornsson H, Samuelsson K, Karlsson J, Forssblad M (2014) Outcomes after ACL reconstruction with focus on older patients: results from The Swedish National Anterior Cruciate Ligament Register. Knee Surg Sports Traumatol Arthrosc 22:379–386
Dudhia J (2005) Aggrecan, aging and assembly in articular cartilage. Cell Mol Life Sci 62:2241–2256
Englund M, Lohmander LS: Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum 50:2811–2819
Felson DT, Goggins J, Niu JB, Zhang YQ, Hunter DJ (2004) The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum 50:3904–3909
Felson DT, Zhang YQ, Hannan MT, Naimark A, Weissman B, Aliabadi P et al (1997) Risk factors for incident radiographic knee osteoarthritis in the elderly—the Framingham study. Arthritis Rheum 40:728–733
Harris K, Driban JB, Sitler MR, Cattano NM, Hootman JM (2015) Five-year clinical outcomes of a randomized trial of anterior cruciate ligament treatment strategies: an evidence-based practice paper. J Athl Train 50:110–112
Heijink A, Gomoll AH, Madry H, Drobnic M, Filardo G, Espregueira-Mendes J et al (2012) Biomechanical considerations in the pathogenesis of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 20:423–435
Jiang LY, Tian WJ, Wang YC, Rong JS, Bao CD, Liu YP et al (2012) Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis. Jt Bone Spine 79:291–297
Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD (2013) A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train 48:810–817
Khan T, Alvand A, Prieto-Alhambra D, Culliford DJ, Judge A, Jackson WF et al (2018) ACL and meniscal injuries increase the risk of primary total knee replacement for osteoarthritis: a matched case-control study using the Clinical Practice Research Datalink (CPRD). Br J Sports Med. https://doi.org/10.1136/bjsports-2017-097762
Lohmander LS, Englund PM, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35:1756–1769
Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50:3145–3152
Losina E, Weinstein AM, Reichmann WM, Burbine SA, Solomon DH, Daigle ME et al (2013) Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res (Hoboken) 65:703–711
Magnussen RA, Borchers JR, Pedroza AD, Huston LJ, Haas AK, Spindler KP et al (2018) Risk factors and predictors of significant chondral surface change from primary to revision anterior cruciate ligament reconstruction a MOON and MARS cohort study. Am J Sports Med 46:557–564
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr et al (2014) Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 42:2363–2370
Melton JTK, Murray JR, Karim A, Pandit H, Wandless F, Thomas NP (2011) Meniscal repair in anterior cruciate ligament reconstruction: a long-term outcome study. Knee Surg Sports Traumatol Arthrosc 19:1729–1734
Mihata LCS, Beutler AI, Boden BP (2006) Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer, and basketball players—implications for anterior cruciate ligament mechanism and prevention. Am J Sports Med 34:899–904
Nordenvall R, Bahmanyar S, Adami J, Mattila VM, Fellander-Tsai L (2014) Cruciate ligament reconstruction and risk of knee osteoarthritis: the association between cruciate ligament injury and post-traumatic osteoarthritis. A population based nationwide study in Sweden, 1987–2009. Plos One 9:7
Oiestad BE, Holm I, Engebretsen L, Aune AK, Gunderson R, Risberg MA (2013) The prevalence of patellofemoral osteoarthritis 12 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 21:942–949
Roos H, Adalberth T, Dahlberg L, Lohmander LS (1995) Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthr Cartil 3:261–267
Sanders TL, Kremers HM, Bryan AJ, Larson DR, Dahm DL, Levy BA et al (2016) Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 44:1502–1507
Schmitt LC, Paterno MV, Hewett TE (2012) The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 42:750–759
Sharma L, Lou C, Cahue S, Dunlop DD (2000) The mechanism of the effect of obesity in knee osteoarthritis—the mediating role of malalignment. Arthritis Rheum 43:568–575
Spindler KP, Huston LJ, Wright RW, Kaeding CC, Marx RG, Amendola A et al (2011) The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction a population cohort study. Am J Sports Med 39:348–359
Thomas AC, Hubbard-Turner T, Wikstrom EA, Palmieri-Smith RM (2017) Epidemiology of posttraumatic osteoarthritis. J Athl Train 52:491–496
Tourville TW, Johnson RJ, Slauterbeck JR, Naud S, Beynnon BD (2013) Assessment of early tibiofemoral joint space width changes after anterior cruciate ligament injury and reconstruction a matched case-control study. Am J Sports Med 41:769–778
von Porat A (2004) High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis 63:269–273
Zhang YQ, Jordan JM (2010) Epidemiology of osteoarthritis. Clin Geriatr Med 26:355–369
Funding
This study was not externally funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Ethical approval
All data from PearlDiver are de-identified and anonymous and were, thus, deemed exempt by the University’s Institutional Review Board.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bodkin, S.G., Werner, B.C., Slater, L.V. et al. Post-traumatic osteoarthritis diagnosed within 5 years following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 28, 790–796 (2020). https://doi.org/10.1007/s00167-019-05461-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05461-y