Abstract
Purpose
Patient-specific instruments (PSIs) are helpful tools in high tibial osteotomy (HTO) in patients with symptomatic varus malalignment of the mechanical leg axis. However, the precision of HTO can decrease with malpositioned PSI. This study investigates the influence of malpositioned PSI on axis correction, osteotomy, and implant placement.
Methods
With a mean three-dimensional (3D) model (0.8° varus), PSI-navigated HTOs were computer simulated. Two different guide designs, one with stabilising hooks and one without, were used. By adding rotational and translational offsets of different degrees, wrong placements of PSI were simulated. After 5° valgisation of the postoperative mechanical axis, the distance between joint-plane and osteotomy screws, respectively, were measured. The same simulations were performed in a patient with varus deformity (7.4° varus).
Results
In the mean 3D model, the postoperative mechanical axis was within 3.9°–4.5° valgus with mean value of 4.1° ± 0.1° (correct axis 4.2° valgus). Surgical failure concerning osteotomy occurred in 17 of 76 HTOs. Significantly safer screw placement was observed using PSI with stabilising hooks (p = 0.012). In the case of the 3D model with 7.4° varus deformity, the postoperative mechanical axis was within 3.2°–3.9° valgus with mean value of 3.8° ± 0.2° (correct axis 3.9° valgus). Surgical failure concerning osteotomy occurred in 3 of 38 HTOs. Screws were always within the safety distance.
Conclusion
The clinical relevance of the presented study is that malpositioning of a PSI within the possible degrees of freedom does not have a relevant influence on the axis correction. The most vulnerable plane for surgical failure is the sagittal plane, wherefore the treating surgeon should verify correct guide placement to prevent surgical failure, particularly in this plane.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies have shown that precise axis correction is crucial for a successful surgical outcome in high tibial osteotomy (HTO), because under- or over-correction is a primary reason for clinical failure [2, 5, 8, 10]. Computer-assisted surgical navigation techniques based on image-based systems [7, 10] or patient-specific instrumentations (PSI) have been proposed to improve the intraoperative precision of HTOs [7]. The advantages of PSI include the simulation of preoperative planning and a stepwise intraoperative procedure including assistance in implant placement. However, malpositioning of PSI can result in intraarticular fractures or intraarticular screw positioning. The precision of a PSI surgery relies on the placement of the very first guide (i.e., the basic guide [14]), used to establish a correspondence between the preoperative plan and the intraoperative situation. If the position or orientation of the basic guide is incorrect, the deviation is consequently transferred to all subsequent steps of the surgery.
In this study, the influence of guide malpositioning on HTO was investigated using three-dimensional (3D) computer simulation. Different combinations of displacements and rotations were applied to the optimal guide position, and the effects on the osteotomy plane, the mechanical axis correction, and screw positions and orientations were measured. Investigations of how different guide designs would improve or worsen correct guide placement have been likewise performed.
In line with the leading principle of the best accuracy in HTO, we hypothesized that a translation of 5 mm or a rotation of 2.5° in placing PSI could probably result in a considerable deviation from the aimed postoperative situation. Therefore, it was the goal of this study to assist the treating surgeon by determining the degree and boundaries of malpositioning of PSI that would result in relevant deviation from the planned axis correction in critical osteotomy or in implant placement.
Materials and methods
The local ethical committee approved this study (Zurich Cantonal Ethics Commission, req-2019-0032) and all patients gave their informed consent for their participation in and the publication of this study.
A mean 3D model of a right lower limb was generated from computed tomography (CT) data of 21 healthy subjects using a statistical shape modeling approach described by Albrecht et al. [1].
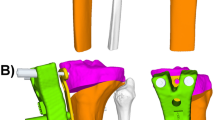
The leg model was imported into the preoperative planning software CASPA (Balgrist CARD AG, Zurich, Switzerland). An antero-posterior (AP)-projected 3D mechanical axis of 0.8° varus was calculated using a measurement method similar to the one described by Fürnstahl et al. [6]. For study purposes, it was assumed that a valgisation of the mechanical axis by 5° has to be performed (postoperative mechanical axis of 4.2° valgus). Based on this assumption, the corresponding HTO was simulated [6], and two different generations of MyOsteotomy® PSI were created by providing anatomical models and planned correction angle to the manufacturer of the PSI system (Medacta/Balgrist CARD AG; Switzerland) as shown in Fig. 1. The second generation of the PSI guides includes two additional stabilising arms extending to the anterior and posteromedial part of the proximal tibia.
With the MyOsteotomy® system (Medacta SA, Castel San Pietro, Switzerland), the navigation of an HTO is performed by applying first a pre-reduction guide containing a cutting slit to guide the osteotomy and four drill sleeves used to set four Schanz pins. The Schanz pins are used as reference pins to apply the post-reduction guide and to navigate plate and screw placement, as the positions and directions of the pins correspond with the uniaxial locking screws of the implant. In this study, a Tomofix Medial High Tibial Plate (Depuy-Synthes Oberdorf, Switzerland) (MHT) was used.
The 3D models of the first- and second-generation pre-reduction guides were imported into the CASPA software to simulate incorrect placements by modifying the original guide positions. Incorrect placements were simulated by applying rotations and translations of different magnitude to the guide, according to the coordinate system in the centre of mass of the Tomofix plate (Fig. 2). The coordinate system of a correctly placed Tomofix plate was selected due to the correspondence of the position of the plate to the surgical approach. The x-axis (red) of the coordinate system corresponded to the plate’s length axis. The y-axis (green) was defined normal to the x-axis in the postero-anterior direction. The z-axis (blue) pointed away from the bone surface, being normal to both the x- and y-axis. Translational malpositioning was simulated by shifting the guide in a proximal and distal direction along the x-axis in steps of 5 mm, 10 mm, 15 mm, and 20 mm. Rotational malpositioning of the guide was simulated by rotating the guide from its original position by 2.5°, 5°, 7.5°, 10°, and 15° in clockwise and counter-clockwise directions around each of the three axes. Therefore, a total of 76 simulations with malpositioned guides with or without stabilising arms have been performed with the mean 3D model. For each of the two guide designs, 30 incorrect rotational (clockwise and counter-clockwise rotation of the guide around all three axes) and eight incorrect translational malpositions (proximal and distal shift of the guide) were simulated. Impossible transformations causing guide-bone intersections were identified visually and handled as follows. If an intersection between guide and bone model was identified, the transformation applied previously was inverted in a step-wise manner until the intersection was resolved. Cases in which the undersurface of the guide was not in sufficient contact with the bone were treated as follows: while partial loss of guide-bone contact can be possible due to soft-tissue structures, transformation in which greater than 80% of the guide undersurface was not in contact with the bone have been classified as impossible.
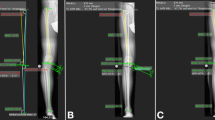
After simulation of HTO, the postoperative outcome was assessed and compared with the original planning with respect to the following parameters. Parameter one was the change in the postoperative mechanical axis “post-MA” (Fig. 3a). The AP-projected 3D mechanical axis was also determined using a measurement method similar to the one described by Fürnstahl et al. [6]. The second parameter, “dist-ost”, assessed the change on the osteotomy plane by measuring the minimum distance between the osteotomy and a 3D plane representing the proximal tibia plateau (Fig. 3b). A computer script was used to loop through all surface points of the osteotomised distal fragment, calculating the normal distance between each point and the plateau plane. A distance of 15 mm or more between osteotomy plane and the tibia plateau was defined as “good”, a distance of 10–15 mm was defined as “ok”, and a distance of less than 10 mm was a “failed” osteotomy. These thresholds were defined according to medial high tibial plate (MHT) surgical technique by DePuy Synthes [3], in which the minimum distance between the osteotomy and joint plane was defined as 10 mm. The third parameter, “dist-screw”, represented the distance of the implant screw that was minimal to the plateau plane (Fig. 3c). The screw-plateau distance was calculated as the distances between the plateau plane and each of the cylinders representing the implant screws. We aimed for a minimum safety distance of 5 mm between the screw and tibia plateau.
Mechanical axis “post-MA” distance between osteotomy and joint plane “dist-ost” and between screws and joint plane “dist-screw”: a in red, the preoperative mechanical axis. In green, the postoperative mechanical axis. b Measurement between osteotomy and joint plane marked in red. c Measurement between screws and joint-plane marked in red. In grey, the cylinders representing the proximal four screws in the Tomofix plate
In the same manner as stated for the 3D mean model, a 3D model of a patient’s left lower limb with worn medial compartment and 7.4° varus deformity and a medial proximal tibial angle of 85.2° was generated. Afterward, the leg model was imported into the CASPA software (Balgrist CARD AG, Zurich, Switzerland). With the pathologic AP-projected 3D mechanical axis and the planning through the Fujisawa point [5], a corresponding valgisation by 11.3° was calculated (postoperative mechanical axis of 3.9° valgus). Afterward, the corresponding HTO was simulated using the guides with additional stabilising arms. Overall, 38 different guide malpositions were simulated. The malpositions included eight incorrect translational (proximal and distal shift of the guide) and 30 incorrect rotational malpositions (clockwise and counter-clockwise rotation of the guide around all three axes). The assessment of the malpositioning of the guides was conducted using the same malpositions as in the simulation with 3D mean model.
Two independent readers performed all 3D simulations and measurements with the mean model and the patient model. Reader 1 performed 3D simulations and measurements in the mean model twice to test–retest reliability.
Statistical analysis
The initial data inspection showed various outcome variables to have non-normal distributions, as assessed with Kolmogorov–Smirnov tests. Therefore, nonparametric inference tests were used for statistical analysis. The analysis was conducted with SPSS statistical software (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.). Where values were not computable due to guide-bone collision (with the parameters described previously in the text), the parameter values in correct position were used for imputation. The Mann–Whitney U test was used to test for a significant influence of using the stabilising hook on the distance and angle measurements. Tests were applied on the full dataset as well as on two sub-datasets, with one dataset being translational and one dataset being rotational variation only. The angular data spread was small. Therefore, the use of conventional statistics rather than circular statistics was unproblematic. Distance measurements were categorised as in the text. The Fisher exact test was used to test for the effect of the stabilising hook on categorised variables. Significance was set at α < 0.05. Test–retest reliability and interrater reliability were described with the intraclass correlation coefficient (ICC). For test–retest reliability, absolute agreement based on a two-way mixed effects model of the single measurement type was employed. Interrater reliability was assessed based on absolute agreement using a two-way random effects model of the single measurement type.
Results
Concerning measurements of the mean 3D model in translational malpositioning, a proximal translated guide results in a postoperative mechanical axis with higher degrees of valgisation (up to + 0.3°), a distal translated guide in lower degrees of valgisation of up to − 0.3° (range 3.9–4.5°, mean value of 4.1° ± 0.1°) in comparison to the correct valgisation (4.2°) (Fig. 4a). Overall, a rotational malpositioned guide is more frequently associated with lower degrees of valgisation with the exception of in the coronal plane, in which a rotation of 2.5° can result in higher degrees of valgisations (range 4.2°–4.4°) (Fig. 4b).
Mechanical axis “post-MA”: statistical evaluation in the mean 3D model with a translational and b rotational malpositioning. For graphical visualisation, boxplots were used, with the ends of the whiskers indicating 1.5 times the interquartile range (IQR) between the lower and upper quartiles, and outliers denoted with a circle. The dotted line depicts the correct valgisation with a postoperative mechanical axis of 4.2° valgus
Evaluation of the influence on the distance between the osteotomy plane and tibial plateau showed that a ≥ 5 mm proximally translated guide resulted in an increased risk of a failed osteotomy (Fig. 5a). Regarding rotational malpositioning of the guide design without stabilising arms, wrong rotation in either the sagittal (≥ 5° rotation) or the coronal (≥ 2.5° rotation) plane resulted in a total of 13 “failed” osteotomies and 25 osteotomies that were “ok” or “good” (Fig. 5b). If osteotomies were performed with the guide containing hooks, only four “failed” osteotomies (all with wrong rotation in the sagittal plane with ≥ 5° rotation) and 34 osteotomies that were “ok” or “good” were observed (Fig. 5b).
Distance between osteotomy and joint plane “dist-ost”: statistical evaluation in the mean 3D model with a translational und b rotational malpositioning. For graphical visualisation, boxplots were used, with the ends of the whiskers indicating 1.5 times the interquartile range (IQR) between the lower and upper quartiles, and outliers denoted with a circle
A significant difference between the groups with respect to screw placement (p = 0.012) was noted. Screw placement below the safety distance of 5 mm could be observed solely in the group without stabilising arms (n = 7, proximal translation ≥ 5 mm, coronal rotation ≥ 7.5°) (Fig. 6). Concerning the postoperative mechanical axis in the model of the patient, no overcorrection was observed (range 3.2°–3.9°, mean value 3.8° ± 0.2°) in comparison to the correct valgisaton (3.9°) (Fig. 7).
Distance between screws and joint plane “dist-screw”: statistical evaluation in the mean 3D model with a translational and b rotational malpositioning. For graphical visualisation, boxplots were used, with the ends of the whiskers indicating 1.5 times the interquartile range (IQR) between the lower and upper quartiles, and outliers denoted with a circle
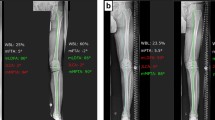
Mechanical axis “post-MA”: statistical evaluation in the patient 3D model with varus deformity with a translational and b rotational malpositioning. For graphical visualisation, boxplots were used, with the ends of the whiskers indicating 1.5 times the interquartile range (IQR) between the lower and upper quartiles, and outliers denoted with a circle. The dotted line depicts the correct valgisation with a postoperative mechanical axis of 3.9° valgus
Referring to the distance between the osteotomy and joint plane, no surgical failure (i.e., “dist-ost” < 10 mm) was observed in translational malpositioning; whereas, rotational malpositioning of ≥ 7.5° in sagittal plain caused a surgical failure in three simulations (Fig. 8).
Distance between osteotomy and joint plane “dist-ost”: statistical evaluation in the patient 3D model with varus deformity with a translational und b rotational malpositioning. For graphical visualisation, boxplots were used, with the ends of the whiskers indicating 1.5 times the interquartile range (IQR) between the lower and upper quartiles, and outliers denoted with a circle
The evaluation of the screw placements showed all screws within the safety distance of greater than 5 mm.
Reliability analysis showed excellent test–retest reliability and excellent interrater reliability with a minimum intraclass correlation coefficient (ICC) of 0.996 for all assessed outcome measures.
Discussion
The most important finding of the present study was that the use of PSI in HTO could be considered as a safe and accurate surgical aid. It was already shown that high accuracy in desired postoperative axis correction can be achieved using PSI in HTO [11, 13]. Further, it could be demonstrated that a misplaced guide within the possible degrees of freedom was shown to have no relevant influence on the postoperative mechanical axis in both models (i.e., mean 3D model and patient model). Likewise, it was shown that the use of guides with additional stabilising hooks could significantly reduce the risk of an incorrectly placed screw. Most likely the reason is the stabilising properties of the hooks on the cone-shaped anatomy of the proximal tibia. Using this generation of guides in both models, every screw placement was within the defined safety margin of 5 mm. Regarding the risk of an osteotomy too close to the joint plane, overall 17 of 76 HTOs with malpositioned guides led to a “failed” osteotomy in the mean model. Eight resulted in malpositioning in the sagittal plane, five in coronal plane, and four in proximal translation. Thereby the hooks seem to reduce the risk for a “failed” osteotomy, although these results are not statistically different in the two groups. Due to the obviously superior stabilising properties of the hooks, simulations on the patient model were performed only with this generation of guides. Here, 3 of 38 HTOs with malpositioned guides led to a “failed” osteotomy, all caused by sagittal plane malpositioning.
However, it is important to notice that these investigations only considered the mechanical axis in AP projection. An analysis of the changes of the posterior tibial slope will be addressed in a future study. The posterior tibial slope could possibly be more affected by a malpositioned guide, especially if malpositioning in the sagittal plane occurs. Various studies have already demonstrated that the posterior tibial slope is unintentionally affected by HTO [4, 9, 12].
Several studies analysed the performance of PSI and navigation systems for improving the precision of the reduction task in osteotomies of the knee, hip, and ankle [15,16,17]. All these studies assessed the accuracy of PSI systems in vivo by comparing the postoperative position and orientation of the reduced anatomy with the one from the preoperative plan. A limitation of such approaches is that reasons for a loss of precision remain unknown. Cadaver experiments can be carried out to perform a more comprehensive error analysis, but the effort for organising and performing cadaver experiments is very high. Our approach was based on computer simulation only, but it was a cost-effective alternative to cadaver experiments if the influence of a large parameter set on the surgical outcome has to be studied.
A limitation of this study is the use of a mean 3D model consisting solely 21 healthy knees, from which some deviation from the standard population can be expected. It would be favorable to use a model consisting of a higher number of healthy knees, reducing deviation from the standard population. However, concerning the law of “Hoffendings inequality”, a sample size of 21 knees should already convert close to the healthy mean standard population.
Another limitation of this study is that guide designs of just a single manufacturer were used. In our investigation, the MyOsteotomy® PSI system was the reference system; but, future studies could use our simulation-based approach to investigate different PSI systems in the same way.
Furthermore, it has to be noted that only two different degrees of valgisations have been simulated (i.e., 5° and 11.3° valgisation), likely covering the range of valgisation in daily practice. Although these two different scenarios provide comparable results, probably higher degrees of valgisations could lead to different results.
Although the here presented study shows no relevant influence on axis correction in high tibial osteotomy, with malpositioning of PSI within the possible degrees of freedom, the treating surgeon should verify correct guide placement nevertheless, since it has been shown that a proximal translation of already 5 mm can result in surgical failure. Regarding rotational malpositioning; correct guide placement should be verified especially in the sagittal plain, as it could be shown that the sagittal plain is the most vulnerable plain for surgical failure.
Conclusion
The clinical relevance of the presented study is that malpositioning of a PSI within the possible degrees of freedom does not have a relevant influence on axis correction in high tibial osteotomy. The most vulnerable plane for surgical failure is the sagittal plane, and the treating surgeon should verify correct guide placement, particularly in this plane.
References
Albrecht T, Luthi M, Gerig T, Vetter T (2013) Posterior shape models. Med Image Anal 17:959–973
Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ (2008) Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br 90:1548–1557
DePuy Synthes (2017) TomoFix Medial High Tibial Plate (MHT). Surgical technique. DSEM/TRM/0115/0288(3)
El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S (2010) Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med 38:323–329
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 10:585–608
Fürnstahl P, Schweizer A, Graf M, Vlachopoulos L, Fucentese S, Wirth S et al (2016) Surgical treatment of long-bone deformities: 3D preoperative planning and patient-specific instrumentation. Computational radiology for orthopaedic interventions. Springer, New York, pp 123–149
Hasan K, Rahman QA, Zalzal P (2015) Navigation versus conventional high tibial osteotomy: systematic review. SpringerPlus 4:271
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am 69:332–354
Jo HS, Park JS, Byun JH, Lee YB, Choi YL, Cho SH et al (2018) The effects of different hinge positions on posterior tibial slope in medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 26:1851–1858
Lutzner J, Gross AF, Gunther KP, Kirschner S (2010) Precision of navigated and conventional open-wedge high tibial osteotomy in a cadaver study. Eur J Med Res 15:117–120
Munier M, Donnez M, Ollivier M, Flecher X, Chabrand P, Argenson JN et al (2017) Can three-dimensional patient-specific cutting guides be used to achieve optimal correction for high tibial osteotomy? Pilot study. Orthop Traumatol Surg Res 103:245–250
Ozel O, Yucel B, Mutlu S, Orman O, Mutlu H (2017) Changes in posterior tibial slope angle in patients undergoing open-wedge high tibial osteotomy for varus gonarthrosis. Knee Surg Sports Traumatol Arthrosc 25:314–318
Perez-Mananes R, Burro JA, Manaute JR, Rodriguez FC, Martin JV (2016) 3D surgical printing cutting guides for open-wedge high tibial osteotomy: do it yourself. J Knee Surg 29:690–695
Vlachopoulos L, Schweizer A, Meyer DC, Gerber C, Fürnstahl P (2016) Three-dimensional corrective osteotomies of complex malunited humeral fractures using patient-specific guides. J Shoulder Elbow Surg 25:2040–2047
Weigelt L, Fürnstahl P, Hirsiger S, Vlachopoulos L, Espinosa N, Wirth SH (2017) Three-dimensional correction of complex ankle deformities with computer-assisted planning and patient-specific surgical guides. J Foot Ankle Surg 56:1158–1164
Yang JC, Chen CF, Luo CA, Chang MC, Lee OK, Huang Y et al (2018) Clinical experience using a 3D-printed patient-specific instrument for medial opening wedge high tibial osteotomy. Biomed Res Int 2018:9246529
Zheng P, Xu P, Yao Q, Tang K, Lou Y (2017) 3D-printed navigation template in proximal femoral osteotomy for older children with developmental dysplasia of the hip. Sci Rep 7:44993
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The local ethical committee approved this study (Zurich Cantonal Ethics Commission, req-2019-0032).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jud, L., Fürnstahl, P., Vlachopoulos, L. et al. Malpositioning of patient-specific instruments within the possible degrees of freedom in high-tibial osteotomy has no considerable influence on mechanical leg axis correction. Knee Surg Sports Traumatol Arthrosc 28, 1356–1364 (2020). https://doi.org/10.1007/s00167-019-05432-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05432-3