Abstract
Purpose
This study aimed at evaluating the association between the volume of the bone bruises and the magnitude of knee sagittal laxity and presence of meniscal injury in patients with anterior cruciate ligament (ACL) rupture. It was hypothesized that higher volumes of bone bruises will be associated with increased knee laxity and the presence of meniscal injury.
Methods
Patients with clinical diagnosis of ACL injury were referred for magnetic resonance imaging (MRI) and knee sagittal laxity measurement with a mechanical instrumented device (Porto-Knee Testing Device). The femoral and tibial bone bruises were assessed by MRI and the volume measured by manually contouring the bone bruise using a computerized software and computed by a mathematical algorithm combining all measured areas. The ACL rupture type (partial or total), meniscal tear (medial or lateral), and the localization of bone bruise were also analyzed.
Results
Seventy-six ACL-ruptured participants were included and 34 patients displayed bone bruises. Tibiofemoral sagittal laxity was higher in participants with complete ACL rupture (p < 0.05), but not influenced by the volume of bone bruises and meniscal status (n.s.). The volume of bone bruises was not significantly associated with the meniscal lesion or with the tibiofemoral sagittal laxity, independently of the meniscal injury status (n.s.).
Conclusions
The volume of femoral and/or tibial bone bruises was not associated with the type of ACL injury, tibiofemoral sagittal laxity or the status of meniscal injury. Bone bruises must be considered as a radiographic sign of injury and should not be suggestive of injury severity and not overvalued.
Level of evidence
Retrospective cohort study, Level III.
IRB number
0011/0014.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bone bruises, also known as bone marrow edema-like lesions, are characterized by hemorrhage, edema, necrosis, and fibrosis [8, 14], and are associated with ACL ruptures in up to 80% of the cases [26]. They are defined as areas of increased signal intensity of the bone marrow in T2-weighted MRI images, but are often better identified through fat suppression and short tau inversion recovery (STIR) sequences [2, 12]. The MRI has moderate to high sensitivity in identifying bone bruises, with 97% and 100% sensitivity for the posterior aspect of the lateral tibial plateau and lateral femoral condyle, respectively [8, 14].
The tibiofemoral bone bruises may be associated with different localizations, severity, and mechanism of injury. These are believed to be caused by a translational contusion, with direct impact loading of the tibiofemoral joint surfaces in association with bone shear stress during the ligament rupture. The pivot-shift injury usually involves a bone bruise pattern on the posterior aspect of the lateral tibial plateau and at the midportion of the lateral femoral condyle near the condylopatellar sulcus (depending on the knee flexion angle upon injury). The “kissing lesion” bone bruise pattern is frequently found in knee hyperextension injuries, with the bone bruise located in the anterior aspect of the femoral condyles and the anterior aspect of the tibial plateau, or medially if the knee extension is associated with a varus load [19]. In addition, the severity of the tibiofemoral bone bruises might be directly related to the impaction energy imposed on the knee during the ACL rupture [21].
The presence of bone bruises in acute ACL injuries has been highly associated with the prevalence of concomitant meniscal and cartilage injuries. In this sense, bone bruises in acute ACL injuries are associated with meniscal injuries in 72–91% of the cases [10, 15]. Additionally, cartilage lesions may occur concomitantly in 80–94% of the cases [15], and even after the bone bruise has resolved, microscopic lesions of the overlying joint cartilage may still be seen [25].
More recently, there is an increasing interest in assessing the size and volume of the tibiofemoral bone bruises [9, 12, 23, 25]. This feature may be correlated with extent of associated meniscal injuries, chondral defects, knee laxity, and long-term functional knee scores [17, 21]. Nonetheless, there is still a lack of information regarding the association of the degree of knee laxity and the volume of the bone bruises. Further research is needed to better understand the characteristics of bone bruises due to ACL injury and its relation to knee laxity and associated meniscal injuries. Thus, this study aims to evaluate the association between the volume of the bone bruises and the magnitude of knee sagittal laxity in patients with ACL rupture. Additionally, it was aimed to assess the correlation between the bone bruises volume and the presence of meniscal injury. The primary hypothesis was that the amount of tibiofemoral bone bruises is not associated with the grade of knee sagittal laxity. The secondary hypothesis was that the presence of meniscal injury would correlate with a greater amount of tibiofemoral bone bruise.
Materials and methods
This study is a retrospective analysis of prospectively collected data and was approved by the Institutional Ethical Committee (IRB number: 0011/0014). The study protocol was conducted in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration. Standard informed consent was obtained for every participant.
Patients
From January of 2015 to November 2016, all consecutive patients with history of knee injury and clinical signs (positive Lachman, anterior drawer and pivot-shift tests) that lead to the ACL rupture clinical diagnosis were referred for stress laxity measurement under MRI using the Porto Knee Testing Device (PKTD®; Soplast, Valongo, Portugal). The ACL rupture was further confirmed by MRI exam. Inclusion criteria included patients with complete or partial ACL ruptured, between 16 and 65 years of age, with imaging and PKTD evaluation under 8 weeks of the ACL injury. Partial rupture was defined as clinically ACL-deficient knee, with the appearance of some intact fibers or well-defined intact single bundle, or presence of an inhomogeneous intrasubstance but with tight ligament. Patients were excluded from this study when (1) they reported a previous ACL-reconstructed knee, (2) injury to other knee ligaments, (3) bilateral ACL injuries, (4) musculoskeletal conditions other than ACL rupture, and (5) the presence of degenerative knee osteoarthritis.
A total of 76 participants with ACL rupture (48 complete and 28 partial rupture) were included within this study. The mean age was 31.7 ± 12.5 years and there were 78% male participants. Demographic characterization of the complete and partial ACL-ruptured patients is summarized in Table 1.
PKTD evaluation and measurement procedures
The PKTD is a polyurethane laxity testing device used for the measurement of knee multidirectional laxity under MRI examination. PKTD has shown significant correlation with KT-1000 and Lachman for posteroanterior (PA) translation, and with lateral pivot-sift for rotation measures [6, 7]. All the patients were supine with 30° of knee flexion and the foot flexed at 90° in a footplate, locking the talus in the ankle mortise. Through the activation of a plunger integrated into a platform at the posterior proximal calf region, a standardized pressure (4 Bar) is applied to produce an anteriorly directed force on the tibia. Thus, the knee was tested at rest (without pressure) and after the application of PA tibial translation. Patients were instructed to avoid muscle guarding.
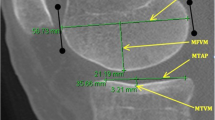
MRI images were obtained using 1.5 T (GE SIGMA LX, Milwaukee, USA) scanner and volume architecture design receive coil. The fast spin echo (FSE) sequence T1 was acquired in both axial and sagittal plane and used for image analysis. Measurements were taken through sets of 1 mm spacing slices and made by the same independent experienced musculoskeletal radiologist. The measurements (in mm) were calculated by the distance from two perpendicular lines to the tibial slope, crossing the most posterior points of the tibial plateau and the femoral condyle. Objective criteria for choosing the most adequate slice are described elsewhere [6, 24]. The difference between the two perpendicular lines was computed for both resting and stress positions, obtaining the PA translations, for the medial and lateral tibial plateaus: MPns, medial plateau position no stress (Fig. 1a); LPns, lateral plateau position no stress (Fig. 1b); MPpa, medial plateau PA translation (Fig. 1c); LPpa, lateral plateau PA translation (Fig. 1d). Moreover, the global anterior translation—sum of medial and lateral PA tibial displacements—was achieved by adding the MPpa and LPpa displacements [6]. All measurements are recorded with one decimal.
Bone bruise volume measurement
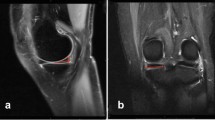
MRI images were obtained using 1.5 T (GE SIGMA LX, Milwaukee, USA) scanner and quadrature transmit receive coil. The imaging protocol included sagittal, axial and coronal proton density (PD) weighted fat-saturated fast spin-echo (FSE) images. The PD-weighted fat-saturated FSE images were used to evaluate and quantify bone bruises and to evaluate the meniscus and ligament integrity. The bone bruise volume was measured when present at the medial and lateral femoral condyles and medial and lateral tibial plateaus. All the bone bruise volume measurements were made by the same independent experienced orthopaedic clinician. The area of bone bruise was identified as an area of high signal intensity compared to the low signal intensity surrounding bone. The MRI sequence was uploaded on ImageJ (http://imagej.nih.gov/ij/) to process the MRI slices into pictures and to highlight the bone bruise and record it as the number of pixels included in the selected area. The bone bruise volume (mm3) was calculated using the following formula: number of voxels × voxel volume. The voxel volume was obtained as follows: pixel resolution × slice thickness [18].
Statistical analysis
The statistical analysis was performed using the Statistical Package for Social Sciences version 24.0® (SPSS, Inc., Chicago, Illinois). The level of significance for all hypothesis tests (p) was set at 0.05. Absolute (n) and relative (%) frequencies were computed for the categorical variables. Continuous variables demonstrated non-normal distribution and were, therefore, presented using median and interquartile range (25 and 75 percentile). The comparison between independent variables was made through Mann–Whitney U test and the Spearman test was used for computing the correlations.
As this was a retrospective study of consecutive patients, no a priori power sample size calculation was performed. We included all consecutive eligible patients who were treated between a timespan of 2 years (January of 2015 to November 2016) and sub-grouped according the respective comparative groups.
Results
Tibiofemoral sagittal laxity
Table 2 displays the laxity measurement results between partial and complete ACL ruptures. Medial and lateral tibial displacements as well as global anterior translation were statistically significantly higher in the complete ACL ruptures group (p < 0.05).
When comparing tibiofemoral sagittal laxity measurements considering the presence of meniscal lesion, there were no statistically significant differences between knees with a meniscal lesion (medial meniscus, lateral meniscus and medial + lateral meniscus) and knees with intact menisci (n.s.; Table 3).
Bone bruises
A total of 34 patients (45%) of the patients displayed tibiofemoral bone bruises. The bone bruises were found most commonly in the lateral femoral condyle (n = 14) and the lateral tibial plateau (n = 28). There were no statistically significant differences in the volume of bone bruise (femoral, tibial or total bruise) between complete and partial ACL ruptures (n.s.; Fig. 2).
The tibiofemoral PA translation was not influenced by the presence of femoral or tibial bruise (n.s.; Table 4). Moreover, the volume of bone bruise was not significantly correlated with the tibiofemoral sagittal laxity, independently of the meniscal injury status (n.s.; Table 5). Additionally, the meniscal status (intact, medial meniscus injury, lateral meniscus injury or medial and lateral meniscus injury) was not correlated with the volume of bone bruise (n.s.; Fig. 3).
Discussion
The main finding of this study is that the tibiofemoral sagittal laxity was not related to the volume of femoral and/or tibial bone bruise. Moreover, the presence of meniscal injury did not influence either the tibiofemoral sagittal laxity or the volume of bone bruise. These results suggest that the pattern and volume of tibiofemoral bone bruises in ACL-ruptured patients is not associated with an increased knee sagittal laxity or the meniscus status.
In the past 3 decades, the prevalence and location of bone bruises in ACL-ruptured patients has been investigated [17]. The evidence of a specific bone bruise pattern during the patient examination is significant as it provides additional clinically relevant information regarding the injury mechanism. The scientific literature reports a wide range of bone bruise prevalence after ACL injury [2, 5, 27]. In the present study, a total of 34 patients (45%) of the patients displayed tibiofemoral bone bruises. The most prevalent anatomical regions that presented bone bruises were the lateral femoral condyle (n = 14) and the lateral tibial plateau (n = 28). These results are in accordance with previous reports in the literature, showing higher prevalence in the lateral femoral condyles and lateral tibial plateau [1, 21, 27], highlighting the pivot-shift mechanism of injury. Additionally, we found 11 bone bruises in the medial femoral condyle (9 of those were in partial ACL ruptures). This is an interesting finding, showing a different bone bruise pattern in ACL partial ruptures, that could be potentially explained by the ACL pivot mechanism [16]. More recently, the size and volume of the bone bruises have gained increasing interest [12, 21, 23, 25]. The evaluation of the bone bruise size and volume may allow a better understanding of the pathophysiology and evolution of the ACL injuries [12]. Nonetheless, the literature concerning the bone bruise volume after ACL injury is still scarce and correlation with clinical symptoms (pain and function) is weak [23].
A recent study by Song et al. [21] investigated the correlation of the prevalence of bone bruises with other associated findings in acute noncontact ACL injuries. In contrast to our results, they found that the presence and severity of bone bruises in the lateral femoral condyles and lateral tibial plateaus were significantly associated with higher grades of knee instability (pivot-shift test, grades II and III). However, it is important to highlight that this study used different methods to measure the bone bruises, as well as to assess the knee instability, which may have led to different results than those reported in the present study. Moreover, although they excluded partial ACL ruptures, the lack of statistical association of bone bruises with increased knee laxity in the present study was independent of the type of ACL rupture. In fact, the extent of bone bruises is affected by factors other than just partial versus complete ACL rupture as body mass index, lower limb alignment and extent of weightbearing at the time of injury, among other factors. Moreover, the present study included partial ACL ruptures as, in some cases, may result in functionally ACL-incompetent knees with abnormal arthrokinematics that may be equivalent to a total rupture [3, 20]. In addition, they found a significant correlation between the presence and severity of lateral compartment bone bruises and presence of lateral meniscal lesions, which has also been reported in previous studies [1, 10, 22, 27]. Along the same lines, the MOON group reporting data from 2318 patients who underwent primary ACL reconstruction without other associated ligament injuries found that the presence of medial or lateral meniscus tears was associated with a one- to twofold increase in the odds of a high-grade Lachman, anterior drawer and pivot-shift tests [13].
In the present study, the meniscal status did not influence the volume of tibiofemoral bone bruise or the degree of tibiofemoral laxity. These results are not corroborated with previous reports in the literature. However, meniscal tear characterization is not always reliable within MRI setting and may lead to false diagnosis [4]. Illingworth and colleagues [9] found a statistically significant relationship between femoral bone bruise volume and the presence of meniscal tears in patients with ACL injury. Song et al. [21] also found an association with the presence and the severity of lateral bone bruise and concomitant lateral meniscal lesions in patients with acute noncontact ACL injuries, and the MOON Group [13] reported that the presence of medial or lateral meniscus tears was associated with increased odds of a high-grade Lachman.
The MOON group performed a multicentre prospective study comprising a cohort of 525 ACL-ruptured patients and investigated which preoperative factors could influence the knee symptoms and pain at the time of index ACL reconstruction surgery. They did not find any significant correlation between the presence and location of the bone bruises and knee symptoms/pain measured by KOOS pain and symptoms subscales and the SF-36 bodily pain subscale [5]. In another study, comprising 81 ACL-reconstructed patients that were prospectively followed for 6 years, the bone bruise severity and volume were measured from the patients’ pre-operative MRI and correlated with knee symptomatology at 2 and 6 years of follow-up. Although they reported that 100% of the patients had at least one bone bruise at the femoral condyles or tibial plateau and that 86% had a bone bruise in two or more locations, the bone bruise volume or severity was not associated with inferior postoperative outcomes at 2- and 6-year follow-up. However, when the bone bruise was present in combination with Outerbridge grade 2 or greater articular cartilage pathology, the patients were 3.4 times more likely to be symptomatic at 6-year follow-up endpoint [11]. Furthermore, other studies have found that the volume of the bone bruises seems to be associated with a higher severity of overlying cartilage matrix damage [18, 25]. However, cartilage damage may occur independently of the presence of bone bruise [26]. The data from these studies suggest that knee symptomatology seems to not be associated with the presence, location, severity, or volume of tibiofemoral bone bruises, but rather with the presence of articular cartilage damage [26]. If not treated correctly at the time of the ACL reconstruction, these cartilage injuries may further develop postoperatively and even progress into early knee osteoarthritis. Hence, when patients with high-risk of developing chondral changes are identified at the time of the ACL reconstruction, conservative and/or surgical strategies should be applied to delay the damage progression.
There are some limitations within this study. Although experimental computerized algorithms have been developed to identify and quantify the volume of the bone bruises [12, 25], due to their complexity, their use is still exclusive to scientific research purposes [17]. Moreover, we acknowledge that the method used for measuring the bone bruise volume is an approximate estimation of its true volume, but our goal was to make these measurements with a simple method that could be easily replicated in any MRI setting, without requiring any special or complex software. In addition, the assessment and correlation of the underlying cartilage damage and the prospective follow-up of this study’s patient cohort could provide important insights into the healing progression of the bone bruises and underlying articular cartilage damage, development of tibiofemoral chondral changes and its association with prospective knee symptomatology. The bone bruises were assessed within 8 weeks following injury which may have influenced the extent of the bone bruise volume.
Although the results of this study did not find a significant association, these are of clinical relevance. The volume of femoral and/or tibial bone bruises is clinically a traumatic sign of injury. However, the volume of bone bruises is not correlated with severity or the amount of laxity or meniscal lesions. Hence, bone bruises must be considered a radiographic sign of injury and should not be suggestive of injury severity and not overvalued.
Conclusion
The volume of femoral and/or tibial bone bruises was not associated with the type of ACL injury, tibiofemoral sagittal laxity or the status of meniscal injury. Bone bruises must be considered as a radiographic sign of injury and should not be suggestive of injury severity and not overvalued.
References
Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM (2013) A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med 41:1801–1807
Bretlau T, Tuxøe J, Larsen L, Jørgensen U, Thomsen HS, Lausten G (2002) Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc 10:96–101
Dejour D, Ntagiopoulos PG, Saggin PR, Panisset J-C (2013) The diagnostic value of clinical tests, magnetic resonance imaging, and instrumented laxity in the differentiation of complete versus partial anterior cruciate ligament tears. Arthroscopy 29:491–499
Dufka FL, Lansdown DA, Zhang AL, Allen CR, Ma CB, Feeley BT (2016) Accuracy of MRI evaluation of meniscus tears in the setting of ACL injuries. Knee 23:460–464
Dunn WR, Spindler KP, Amendola A, Andrish JT, Kaeding CC, Marx RG et al (2010) Which preoperative factors, including bone bruise, are associated with knee pain/symptoms at index anterior cruciate ligament reconstruction (ACLR)? A Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med 38:1778–1787
Espregueira-Mendes J, Andrade R, Leal A, Pereira H, Skaf A, Rodrigues-Gomes S et al (2017) Global rotation has high sensitivity in ACL lesions within stress MRI. Knee Surg Sports Traumatol Arthrosc 25:2993–3003
Espregueira-Mendes J, Pereira H, Sevivas N, Passos C, Vasconcelos JC, Monteiro A et al (2012) Assessment of rotatory laxity in anterior cruciate ligament-deficient knees using magnetic resonance imaging with Porto-knee testing device. Knee Surg Sports Traumatol Arthrosc 20:671–678
Gentili A, Seeger LL, Yao L, Do HM (1994) Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology 193:835–840
Illingworth KD, Hensler D, Casagranda B, Borrero C, van Eck CF, Fu FH (2014) Relationship between bone bruise volume and the presence of meniscal tears in acute anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 22:2181–2186
Jelić Đ, Mašulović D (2011) Bone bruise of the knee associated with the lesions of anterior cruciate ligament and menisci on magnetic resonance imaging. Vojnosanit Pregl 68:762–766
Lattermann C, Jacobs CA, Reinke EK, Scaramuzza EA, Huston LJ, Dunn WR et al (2017) Are bone bruise characteristics and articular cartilage pathology associated with inferior outcomes 2 and 6 years after anterior cruciate. Ligament reconstruction? Cartilage 8:139–145
Li X, Ma BC, Bolbos RI, Stahl R, Lozano J, Zuo J et al (2008) Quantitative assessment of bone marrow edema-like lesion and overlying cartilage in knees with osteoarthritis and anterior cruciate ligament tear using MR imaging and spectroscopic imaging at 3 T. J Magn Reson Imaging 28:453–461
Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP, Group M (2016) Factors associated with high-grade Lachman, pivot shift, and anterior drawer at the time of anterior cruciate ligament reconstruction. Arthroscopy 32:1080–1085
McCauley TR, Moses M, Kier R, Lynch JK, Barton JW, Jokl P (1994) MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. AJR Am J Roentgenol 162:115–119
Nishimori M, Deie M, Adachi N, Kanaya A, Nakamae A, Motoyama M et al (2008) Articular cartilage injury of the posterior lateral tibial plateau associated with acute anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 16:270–274
Noyes FR, Jetter AW, Grood ES, Harms SP, Gardner EJ, Levy MS (2014) Anterior cruciate ligament function in providing rotational stability assessed by medial and lateral tibiofemoral compartment translations and subluxations. Am J Sports Med 43:683–692
Papalia R, Torre G, Vasta S, Zampogna B, Pedersen DR, Denaro V et al (2015) Bone bruises in anterior cruciate ligament injured knee and long-term outcomes. A review of the evidence. Open Access J Sports Med 6:37
Pedersen DR, El-Khoury GY, Thedens DR, Saad-Eldine M, Phisitkul P, Amendola A (2017) Bone contusion progression from traumatic knee injury: association of rate of contusion resolution with injury severity. Open Access J Sports Med 8:9
Sanders TG, Medynski MA, Feller JF, Lawhorn KW (2000) Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics 20:S135–S151
Siebold R, Fu FH (2008) Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy 24:1289–1298
Song G-y, Zhang H, Wang Q-q, Zhang J, Li Y, Feng H (2016) Bone contusions after acute noncontact anterior cruciate ligament injury are associated with knee joint laxity, concomitant meniscal lesions, and anterolateral ligament abnormality. Arthroscopy 32:2331–2341
Spindler KP, Schils JP, Bergfeld JA, Andrish JT, Weiker GG, Anderson TE et al (1993) Prospective study of osseous, articular, and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am J Sports Med 21:551–557
Szkopek K, Warming T, Neergaard K, Jørgensen H, Christensen H, Krogsgaard M (2012) Pain and knee function in relation to degree of bone bruise after acute anterior cruciate ligament rupture. Scand J Med Sci Sports 22:635–642
Tashiro Y, Okazaki K, Miura H, Matsuda S, Yasunaga T, Hashizume M et al (2009) Quantitative assessment of rotatory instability after anterior cruciate ligament reconstruction. Am J Sports Med 37:909–916
Theologis AA, Kuo D, Cheng J, Bolbos RI, Carballido-Gamio J, Ma CB et al (2011) Evaluation of bone bruises and associated cartilage in anterior cruciate ligament—injured and—reconstructed knees using quantitative T 1ρ magnetic resonance imaging: 1-year cohort study. Arthroscopy 27:65–76
Walczak BE, Lukes C, Amendola N, Dunn WR (2017) Limited evidence that the presence of a bone bruise alone affects the clinical outcome of surgically reconstructed anterior cruciate ligaments: a systematic review. J ISAKOS 2:186–190
Yoon KH, Yoo JH, Kim K-I (2011) Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Jt Surg Am 93:1510–1518
Funding
The authors declare that there was no funding of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JEM is the patent holder of the PKTD but does not receive any royalties or fees.
Ethical approval
This study was approved by the Institutional Ethical Committee (IRB number: 0011/0014). The study protocol was conducted in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration.
Rights and permissions
About this article
Cite this article
Bastos, R., Andrade, R., Vasta, S. et al. Tibiofemoral bone bruise volume is not associated with meniscal injury and knee laxity in patients with anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 27, 3318–3326 (2019). https://doi.org/10.1007/s00167-018-5343-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5343-2