Abstract
Purpose
To compare clinical outcomes and tunnel widening following anterior cruciate ligament reconstruction (ACLR) performed with an all-inside technique (Group A) or with a bioabsorbable tibial screw and suspensory femoral fixation (Group B).
Methods
Tunnel widening was assessed using computed tomography (CT) and a previously validated analytical best fit cylinder technique at approximately 1-year following ACLR. Clinical follow-up comprised evaluation with IKDC, KSS, Tegner, Lysholm scores, and knee laxity assessment.
Results
The study population comprised 22 patients in each group with a median clinical follow-up of 24 months (range 21–27 months). The median duration between ACLR and CT was 13 months (range 12–14 months). There were no significant differences in clinical outcome measures between groups. There were no differences between groups with respect to femoral tunnel widening. However, there was a significantly larger increase in tibial tunnel widening, at the middle portion, in Group B (2.4 ± 1.5 mm) compared to Group A (0.8 ± 0.4 mm) (p = 0.027), and also at the articular portion in Group B (1.5 ± 0.8 mm) compared to Group A (0.8 ± 0.8 mm) (p = 0.027).
Conclusion
Tibial tunnel widening after ACLR using hamstring tendon autograft is significantly greater with suspensory femoral fixation and a bioabsorbable tibial interference screw when compared to an all-inside technique at a median follow-up of 2 years. The clinical relevance of this work lies in the rebuttal of concerns arising from biomechanical studies regarding the possibility of increased tunnel widening with an all-inside technique.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 1995, Morgan et al. first described all-inside anterior cruciate ligament reconstruction (ACLR) using both tibial and femoral sockets, and the avoidance of drilling complete tunnels. Although there are now many variations of all-inside ACLR, recent systematic review has demonstrated that the overall strategy is associated with low graft failure rates and significant improvements in clinical outcomes with respect to knee function, pain, stability, and patient satisfaction at short-term follow-up. However, there are only a small number of comparative studies [8, 17, 23] and therefore the proposed benefits over standard techniques remain unproven. One of the theoretical benefits is a decrease in the incidence of tunnel widening (TW) [12]. This is a phenomenon that frequently occurs after ACLR, particularly with hamstring tendon grafts. It is reported to occur predominantly in the first 6 weeks after surgery. The main clinical concern with tunnel widening is that in the event of graft failure, enlargement of tunnels can compromise single stage revision ACLR, and result in the need for bone grafting and a two-stage procedure.
The pathophysiology of tunnel widening is multifactorial. Mechanical, surgical and biological factors have all been implicated in the etiology [4, 5, 16, 28]. However, the interaction between factors is not completely understood and for this reason, the rate of tunnel widening after ACLR must be specifically evaluated for different variations of surgical technique. To the knowledge of the authors only one previous study has specifically evaluated tunnel widening after all-inside ACLR in a comparative study. Mayr et al. demonstrated that femoral tunnel widening after all-inside ACLR using suspensory fixation was significantly greater than following ACLR with aperture fixation with interference screws for both tibial and femoral tunnels [18]. Although the latter is a frequently used technique, a multi-national registry based review of contemporary practice reveals that in Denmark, Norway, Sweden and the UK the most popular graft choice is hamstring tendon autograft fixed with an interference screw on the tibia and suspensory femoral fixation [25]. The aim of this study was therefore to compare tunnel widening following this technique against all-inside ACLR. The study hypothesis was that a significantly greater degree of tibial tunnel widening would be observed with the all-inside technique when compared to ACLR fixed with an interference screw on the tibia and suspensory femoral fixation.
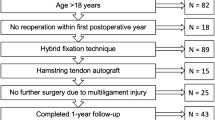
Materials and methods
Patients who underwent hamstring tendon autograft ACLR for a chronic ACL rupture (> 3 months from the date of injury) with either the graftlink all-inside technique [14] or with suspensory femoral fixation and a tibial interference screw between January 2016 and June 2016 were considered for study eligibility. Patients were excluded if they had sustained a multi-ligament injury, or had a Segond fracture, but patients with meniscal and/or chondral injuries were included. Further exclusion criteria were a history of previous knee injury/surgery, patients aged over 40 years and those with a body mass index (BMI) greater than 30. Informed consent was obtained from all patients.
Surgical technique
For both surgical techniques, the tunnels were drilled corresponding to graft diameter. The femoral tunnel center was located at approximately 40% of the proximal–distal distance of the lateral notch and was centered between the lateral intercondylar ridge and the posterior articular margin. This point was centered over the lateral bifurcate ridge at a distance equivalent to the planned tunnel radius, plus an additional 2.5 mm from the posterior articular cartilage. The center of the tibial tunnel was located at 40% of the medial–lateral width of the interspinous distance, in line with the posterior edge of the lateral meniscal anterior horn, approximately 15 mm anterior–posterior cruciate ligament [1].
Group A: all-inside ACLR
In the all-inside group, patients underwent ACL reconstruction performed with the graftlink technique [14]. The harvested semitendinosus tendon was quadrupled to obtain a final graft length of no more than 75 mm, and sewn in linkage with a TightRope-RT adjustable loop cortical button (Arthrex, Naples, FL, USA) and a high strength suture (No. 0 FiberWire; Arthrex, Naples, FL, USA) on each side of the graft. Standard anterolateral (AL) and anteromedial portals were used. With a standard guide set at 60–65°, a 25-mm tibial socket was created at the anatomic ACL insertion point using a specific retrodrill (Flipcutter, Arthrex, Naples, FL, USA). A 25-mm femoral socket was created with an outside-in technique using a standard guide set approximately 100°–110° and the same retrodrill as on the tibial side. Using a shuttle suture on both sides, the graft was introduced into the knee through the AM portal and fixed first on femoral side, then on tibial side with the “flip-then-fill technique” [14].
Group B: femoral suspensory fixation and tibial interference screw
Patients underwent ACLR with an outside-in technique and doubled semitendinosus and gracilis tendons (DGST) autograft. The tibial tunnel was drilled over a wire that was placed in the anatomic tibial ACL insertion point using the Arthrex footprint guide set at 60°–65° with a standard anterograde drill. On the femoral side, a 25-mm bone socket was drilled with an outside-in technique and using the Arthrex footprint guide with drill sleeve set at approximately 100°–110° employing a Flipcutter retrodrill (Arthrex, Naples, USA). The graft was then passed fixed with an adjustable loop length device on the femur (TightRope-RT Arthrex, Naples, FL, USA) and an absorbable interference screw (Deltascrew, Arthrex, Naples, FL, USA), sized 1 mm greater than graft diameter, on the tibia.
Postoperative rehabilitation
All patients were placed in an extension brace for 2 weeks. Isometric exercises were commenced on the second postoperative day and patients were encouraged with progressive weight bearing as tolerated. After 2 weeks, the brace was removed and an emphasis placed on regaining full range of motion. Cycling and swimming were permitted from 4 weeks onwards. Patients participated in progressive functional activities including running at 3 months and a return to sport specific training at 6–8 months after surgery.
Postoperative clinical evaluation
As part of the standardized follow-up for ACLR at our institution, all patients underwent standard knee ligament examination, specifically including an evaluation of Lachman’s test, side-to-side laxity difference testing using a knee laxity-testing device (KT-1000; MEDmetric, San Diego, CA, USA) and the pivot-shift test. The Lachman test was graded as negative (normal anterior–posterior translation with a firm end point), positive 1+ (increased anterior–posterior translation as compared with the contralateral side with a firm end point) and positive 2+ (increased anterior–posterior translation as compared with contralateral side with no firm end point). The pivot-shift test was graded 0 (negative), 1 (glide), 2 (jerk), and 3 (subluxation) [10]. In addition, the IKDC Knee Examination Form, Knee Society Score (KSS) for pain and function, and Tegner and Lysholm scores were recorded pre-operatively and at final follow-up.
Radiological evaluation
All patients underwent post-operative CT to assess tunnel widening at approximately 1 year following ACLR [16]. A 16-slice MSCT scanner Philips MX 8000 with post-process multislab reconstruction on sagittal and coronal planes (slice thickness 1 mm, retrorecons 0.75 mm) was used for the evaluation. Scanning was performed from a level just above the femoral tunnel to a level below the external aperture of the tibial tunnel. The CT images were exported to an image analysis software (Mimics v1.6, Materialise, Leuven, Belgium) and a manual segmentation of the bone structures, bone tunnels and fixation devices was performed using bone-soft tissue density variation. The segmentation process relies on using bone-soft tissue density variation on CT images, adjusting a density range to highlight bone anatomy on CT scan images. Manual revision of the CT images was performed to correct errors, and assure that the outline of the bone and tunnels was appropriately filled. This allowed the creation of a specific 3D bone model of the knee joint for all patients (Fig. 1a, b).
CT images of all patients were exported to an image analysis software (Mimics v1.6, Materialise, Leuven, Belgium) and a manual segmentation of the bone structures, bone tunnels and fixation devices was performed, allowing for the creation of a specific 3D bone model of the knee joint for all patient (a left knee, anterior view of an all inside technique; b left knee, posterior view of an all inside technique)
Tunnel diameter was evaluated using the best fit cylinder technique reported in detail by Crespo et al. who used the Mimics v1.6, Materialise software, that allows an analytical cylinder to be fitted to the 3D cast of the entire tunnel length and then measured [Fig. 2a–c]. This method was selected because Crespo et al. [3] demonstrated that this method provided a high correlation with the drill sizes used, demonstrated high inter-rater agreement concluded that this was the best method to evaluate ACL tunnel size in a 3D model. Moreover, it has previously been validated, and has demonstrated high intraobserver and interobserver reliability and accuracy intraclass correlation coefficient (95% CI): 0.745 [0.553–0.862] and intra-rater agreement (ICC [95% CI]) were totally automated, with total agreement (ICC of 1.00). The measurement accuracy was ± 0.02 mm [3, 26].
a Right knee, 3D model of tibia, bone socket and fixation device of an all-inside technique; b right knee, 3D cast of tibial bone socket of an all-inside technique; c right knee, creation of an analytical best fit cylinder fitted to the 3D cast of the articular portion of the tibial bone socket of an all-inside technique
In the tibial tunnel of Group B, careful attention was paid to the position of the interference screw: when the screw head was found to protrude from the bone tunnel (Fig. 3 a, b), thereby artificially enlarging the diameter of the best fit cylinder, to avoid this bias, a line of the tunnel border was drawn through the screw. To assess changes in tunnel widening in both groups, the diameters of the tunnels measured at follow-up (T1) were compared with the diameter of the drill used at surgery (T0) in each patient.
Statistical analysis
Institutional review board approval from University of Rome La Sapienza was granted for the study.
Statistical analysis generated standard descriptive statistics: means, standard deviations, and proportions. The Wilcoxon test was used to evaluate differences between pre-operative and follow-up results in each group. The Mann–Whitney U test was applied to verify differences between the two groups. Statistical significance was set at P < 0.05. The Statistical Package for Social Sciences (SPSS) software version 22 was used for all calculations. A sample size calculation for a continuous outcome superiority trial was performed using the sealedenvelope.com online based software and published tunnel widening data from Mayr et al. [18]. This demonstrated that 40 patients were required to have a 90% chance of detecting, as significant at the 5% level, an increase in the primary outcome measure from 111.1 ± 10.8% (tibial tunnel widening reported by Mayr et al. [18] with an interference screw) in the control group to 122.4% (tibial tunnel widening with an all-inside technique) in the experimental group.
Results
The overall study population comprised of 44 patients (22 in each group) who underwent ACLR for a chronic ACL injury. The mean time between injury and surgery was 8 months (range 5–13 months). The median duration of clinical follow-up after ACLR was 24 months (range 21–27 months). The median duration of time between ACLR and post-operative CT evaluation was 13 months (range 12–14 months).
The baseline characteristics of the two groups are shown in Table 1.
No significant differences were detected between the two groups with respect to any of the clinical or patient-reported outcome measures assessed. This information is summarized in Tables 2 and 3.
Radiological evaluation
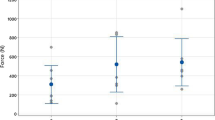
Tunnel widening data are summarized in Table 4. In Group A, the mean drill diameter at T0 was 9.3 ± 0.5. This was significantly increased at T1 by 30% to a mean femoral tunnel diameter of 12.1 ± 0.9 mm at the middle portion (P = 0.02), and by 28% to a mean diameter of 12 ± 1.7 mm at the articular portion (P = 0.04). The mean tibial tunnel diameter was increased at T1 by 8% to 10.1 ± 0.6 mm at the middle portion (n.s.) and significantly increased by 9% to 10.1 ± 1 mm at the articular portion (P = 0.02).
In Group B, the mean drill diameter at T0 was 8.6 ± 0.5. This was significantly increased at T1 by 23% to a mean femoral tunnel diameter of 10.6 ± 1.2 mm at the middle portion (P = 0.01) and by 25% to 10.8 ± 1 mm at the articular portion (P = 0.01). The mean tibial tunnel diameter increased significantly by 27% to 11.1 ± 1.6 mm at the middle portion (P = 0.01) and 17% to 10.1 ± 1.2 mm at the articular portion (P = 0.02).
The differences in tunnel widening between groups are summarized in Table 5. No differences were found between groups with respect to femoral tunnel widening. However, there was a significantly larger increases in tunnel widening on the tibial side, at the middle portion, in Group B (2.4 ± 1.5 mm) compared to Group A (0.8 ± 0.4 mm) (P = 0.027), and also at the articular portion in Group B (1.5 ± 0.8 mm) compared to Group A (0.8 ± 0.8 mm) (P = 0.027).
Discussion
The main findings of this study were that tibial tunnel widening was significantly greater following ACLR performed with femoral suspensory fixation and a tibial interference screw fixation when compared to the all-inside technique and that there was no significant differences between groups with respect to femoral tunnel widening or clinical outcomes.
The potential reasons for the differences between groups with respect to tibial tunnel widening can be considered with respect to biomechanical and biological issues, respectively. It is recognized that tunnel widening is greater with hamstring tendon grafts when compared to BTB and also that most tunnel widening occurs in the first 6 weeks after surgery. This suggests that reducing the time to graft to bone healing, by improving the biological environment, may reduce the extent of tunnel widening. Bone ingrowth has been reported to be slowest at the tunnel apertures and this may be a result of the “synovial bathing effect” [27]. It is postulated that retrograde drilling may reduce this effect because it is associated with less subchondral bone fragmentation as well as fewer fracture fragments at the tibial tunnel aperture compared to anterograde drilling [19]. Retrograde drilling may therefore limit the amount of synovial fluid migration from the joint to the bone tunnel [27]. This is partly supported by Lanzetti et al. [13] who reported that when using cortical suspensory fixation, femoral sockets created using an outside-in technique were associated with significantly less widening than those sockets created with a trans-tibial technique. Similarly, the use of a cortical adjustable loop length device, which allows complete filling of sockets by the graft may also reduce the empty space available for synovial fluid migration [24].
Suspensory fixation may offer other biological advantages over interference screw fixation. Several authors have reported that interference screws provide a limited tendon–bone contact area because much of the tunnel circumference is occupied by the screw itself, while adjustable loop systems provide a greater contact zone [15, 29], and allow “four-zone direct graft healing” which has been associated in animal study with the absence of tunnel widening on radiographic and histologic assessments [29]. In contrast, from a biomechanical perspective, it is suggested that extra-cortical suspensory fixation may actually increase the risk of tunnel widening due to graft micro-motion within the tunnels on the longitudinal axis (the “bungee cord effect”) and transverse axis (the “windshield wiper effect”) [8]. This is therefore a concern with the all-inside technique which uses two adjustable loop suspensory fixation devices, particularly because of recent reports of loop lengthening with adjustable suspensory fixation devices, which may result in increased graft micro-motion. However, some recent biomechanical studies showed no significant loop lengthening using two adjustable loop suspensory devices for femoral tibial fixation [21, 22]. Moreover, no evidence of increased tunnel widening was noted in this study with the all-inside technique, when compared to a standard technique, and this allowed us to reject the study hypothesis.
Bioabsorbable screws are also associated with other disadvantages. Despite their widespread use, they are well recognized for their association with migration, cyst formation, biological/immunological responses to the screw itself, and tunnel widening [2, 20]. However, to the knowledge of the authors, specific data on tunnel widening with the bioabsorbable DeltaScrew (Arthrex, Naples, FL, USA) used for tibial fixation, in association with suspensory femoral fixation, has not been published. It should be emphasized that bioabsorbable screws should not be considered as a single category because different biomaterial compositions may be associated with different degrees of tunnel widening. Karikis et al. [11], in a study of patients undergoing ACLR with interference screw fixation in both femoral and tibial tunnels, demonstrated a reduction in the tibial tunnel diameter at a mean follow-up of 5 years when a bioabsorbable screw was used (Matryx; ConMed Linvatec, Largo, FL, USA). It is not possible to determine whether the differences in tibial tunnel widening between the current study and the findings of Karikis et al. are due to the material properties of the respective screws or due to difference in other aspects of the surgical technique, including the femoral fixation or the length of follow-up.
There is a complex interplay of biomechanical and biological factors that influence tunnel widening after ACLR. Although the exact mechanisms through which tunnel widening occurred in the different groups in this study cannot be determined, it can be concluded that tibial tunnel widening in all-inside ACLR is significantly lower than in patients undergoing tibial fixation with a bioabsorbable screw. It could also be stated that the use of sockets instead of full tunnels confers preservation of bone for revision surgery but this was not specifically evaluated in the current study.
This study demonstrated excellent overall clinical results in both groups. However, it is unlikely that it was adequately powered to detect a difference in clinical outcomes between groups. Despite that it is important to highlight that the outcomes of ACLR in the all-inside group showed excellent return to sport, knee stability, low graft rupture rate and a high Lysholm, Tegner and IKDC score. This is in keeping with other authors reporting the outcomes of all-inside ACLR.
This study has some limitations. The primary limitation was the retrospective design, which has inherent limitations due to the risk of bias and confounding. However, patients included in both groups were not significantly different demographically. The assumption that the tunnel diameter at T0 was the same as the drill diameter used could also be considered a limitation but this choice was determined by the reliability between drill diameter and CT measurements in the early post-operative period reported by previous authors [9, 30], and the benefit of minimizing radiation exposure. The overall study population was relatively small but this was based upon a sample size calculation and inclusion of an adequate number of patients to evaluate tunnel widening. A further limitation was that the median follow-up period was only 2 years. This was considered to be appropriate because Fink et al. [6] and Harris at al [7] reported that most tunnel enlargement occurs within the first 6 weeks after surgery, and Mayr et al. [18] reported that the tunnels usually increased in size up to 6 months postoperatively, and decreased slightly after a year.
The clinical relevance of this work lies in the rebuttal of concerns arising from biomechanical studies regarding the possibility of increased tunnel widening with an all-inside technique.
Conclusions
Tibial tunnel widening after ACLR using hamstring tendon autograft is significantly greater with suspensory femoral fixation and a bioabsorbable tibial interference screw when compared to an all-inside technique at a median follow-up of 2 years.
References
Burnham JM, Malempati CS, Carpiaux A, Ireland ML, Johnson DL (2017) Anatomic femoral and tibial tunnel placement during anterior cruciate ligament reconstruction: anteromedial portal all-inside and outside-in techniques. Arthrosc Tech 6(2):e275–e282
Colombet P, Graveleau N, Jambou S (2016) Incorporation of hamstring grafts within the tibial tunnel after anterior cruciate ligament reconstruction: magnetic resonance imaging of suspensory fixation versus interference screws. Am J Sports Med 44(11):2838–2845
Crespo B, Aga C, Wilson KJ, Pomeroy SM, LaPrade RF, Engebretsen L, Wijdicks CA (2014) Measurements of bone tunnel size in anterior cruciate ligament reconstruction: 2D versus 3D computed tomography model. J Exp Orthop 1(1):2
De Beus A, Koch JE, Hirschmann A, Hirschmann MT (2017) How to evaluate bone tunnel widening after ACL reconstruction—a critical review. Muscles Ligaments Tendons J 7(2):230–239
Fahey M, Indelicato PA (1994) Bone tunnel enlargement after anterior cruciate ligament replacement. Am J Sports Med 22(3):410–414
Fink C, Zapp M, Benedetto KP, Wolfgang H, Hoser C, Rieger M (2001) Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthroscopy 17(2):138–143
Harris NL, Indelicato PA, Bloomberg MS, Meister K, Wheeler DL (2002) Radiographic and histologic analysis of the tibial tunnel after allograft anterior cruciate ligament reconstruction in goats. Am J Sports Med 30(3):368–373
Höher J, Möller HD, Fu FH (1998) Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction? Knee Surg Sports Traumatol Arthrosc 6(4):231–240
Iorio R, Di Sanzo V, Vadalà A, Conteduca J, Mazza D, Redler A et al (2013) ACL reconstruction with hamstrings: how different technique and fixation devices influence bone tunnel enlargement. Eur Rev Med Pharmacol Sci 17(21):2956–2961
Irrgang JJ, Ho H, Harner CD, Fu FH (1998) Use of the international knee documentation committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6(2):107–114
Karikis I, Ejerhed L, Sernert N, Rostgård-Christensen L, Kartus J (2017) Radiographic tibial tunnel assessment after anterior cruciate ligament reconstruction using hamstring tendon autografts and biocomposite screws: a prospective study with 5-Year follow-up. Arthroscopy 33(12):2184–2194
Kim SG, Kurosawa H, Sakuraba K, Ikeda H, Takazawa S, Takazawa Y (2005) Development and application of an inside to-out drill bit for anterior cruciate ligament reconstruction. Arthroscopy 21 (8):1012
Lanzetti RM, Monaco E, De Carli A, Grasso A, Ciompi A, Sigillo R, Argento G, Ferretti A (2016) Can an adjustable-loop length suspensory fixation device reduce femoral tunnel enlargement in anterior cruciate ligament reconstruction? A prospective computer tomography study. Knee 23(5):837–841
Lubowitz JH, Ahmad CS, Anderson K (2011) All-inside anterior cruciate ligament graft-link technique: Second generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy 27(5):717–727
Lubowitz JH, Schwartzberg R, Smith P (2015) Cortical suspensory button versus aperture interference screw fixation for knee anterior cruciate ligament soft-tissue allograft: a prospective, randomized controlled trial. Arthroscopy 31(9):1733–1739
Marchant MH Jr, Willimon SC, Vinson E et al (2010) Comparison of plain radiography, computed tomography, and magnetic resonance imaging in the evaluation of bone tunnel widening after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18(8):1059–1064
Mayr R, Heinrichs CH, Eichinger M, Coppola C, Schmoelz W, Attal R (2015) Biomechanical comparison of 2 anterior cruciate ligament graft preparation techniques for tibial fixation: adjustable-length loop cortical button or interference screw. Am J Sports Med 43(6):1380–1385
Mayr R, Smekal V, Koidl C, Coppola C, Fritz J, Rudisch A, Kranewitter C, Attal R (2017) Tunnel widening after ACL reconstruction with aperture screw fixation or all-inside reconstruction with suspensory cortical button fixation: volumetric measurements on CT and MRI scans. Knee 24(5):1047–1054
McAdams TR, Biswal S, Stevens KJ, Beaulieu CF, Mandelbaum BR (2008) Tibial aperture bone disruption after retrograde versus antegrade tibial tunnel drilling: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 16(9):818–822
Mermerkaya MU, Atay OA, Kaymaz B, Bekmez S, Karaaslan F, Doral MN (2014) Anterior cruciate ligament reconstruction using a hamstring graft: a retrospective comparison of tunnel widening upon use of two different femoral fixation methods. Knee Surg Sports Traumatol Arthrosc 23(8):2283–2291
Monaco E, Bachmaier S, Fabbri M, Lanzetti RM, Wijdicks CA, Ferretti A (2018) Intraoperative workflow for all-inside anterior cruciate ligament reconstruction: an in vitro biomechanical evaluation of preconditioning and knot tying. Arthroscopy 34(2):538–545
Monaco E, Fabbri M, Lanzetti RM, Del Duca A, Labianca L, Ferretti A (2017) Biomechanical comparison of four coupled fixation systems for ACL reconstruction with bone socket or full-tunnel on the tibial side. Knee 24(4):705–710
Mulcahey MK, David TS, Epstein DM, Alaia MJ, Montgomery KD (2014) Transtibial versus anteromedial portal anterior cruciate ligament reconstruction using soft-tissue graft and expandable fixation. Arthroscopy 30(11):1461–1467
Osti M, Krawinkel A, Hoffelner T, Benedetto KP (2015) Quantification of tibial bone loss in antegrade versus retrograde tunnel placement for anterior cruciate ligament reconstruction. Int Orthop 39(8):1611–1614
Prentice HA, Lind M, Mouton C, Persson A, Magnusson H, Gabr A, Seil R, Engebretsen L, Samuelsson K, Karlsson J, Forssblad M, Haddad FS, Spalding T, Funahashi TT, Paxton LW, Maletis GB (2018) Patient demographic and surgical characteristics in anterior cruciate ligament reconstruction: a description of registries from six countries. Br J Sports Med 52(11):716–722
Robbrecht C, Claes S, Cromheecke M, Mahieu P, Kakavelakis K, Victor J, Bellemans J, Verdonk P (2014) Reliability of a semi-automated 3D-CT measuring method for tunnel diameters after anterior cruciate ligament reconstruction: a comparison between soft-tissue single-bundle allograft vs. autograft. Knee 21(5):926–931
Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF (1993) Tendon healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Jt Surg Am 75(12):1795–1803
Sabzevari S, Rahnemai-Azar AA, Shaikh HS, Arner JW, Irrgang JJ, Fu FH (2017) Increased lateral tibial posterior slope is related to tibial tunnel widening after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 25(12):3906–3913
Smith PA, Stannard JP, Pfeiffer FM, Kuroki K, Bozynski CC, Cook JL (2016) Suspensory versus interference screw fixation for arthroscopic anterior cruciate ligament reconstruction in a translational large-animal model. Arthroscopy 32(6):1086–1097
Vadalà A, Iorio R, De Carli A, Argento G, Di Sanzo V, Conteduca F et al (2007) The effect of accelerated, brace free, rehabilitation on bone tunnel enlargement after ACL reconstruction using hamstring tendons: a CT study. Knee Surg Sports Traumatol Arthrosc 15(4):365–371
Funding
No external funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Edoardo Monaco, Andrea Ferretti and Angelo De Carli declares to be consultant for Arthrex.
Ethical approval
All procedure performed in the study involving humans participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Monaco, E., Fabbri, M., Redler, A. et al. Anterior cruciate ligament reconstruction is associated with greater tibial tunnel widening when using a bioabsorbable screw compared to an all-inside technique with suspensory fixation. Knee Surg Sports Traumatol Arthrosc 27, 2577–2584 (2019). https://doi.org/10.1007/s00167-018-5275-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5275-x