Abstract
Purpose
To study the pattern of migration and clinical results up to 10 years of uncemented versus cemented fixation of the femoral component in total knee arthroplasty.
Methods
Randomized controlled trial was conducted of 41 patients (23 women, 18 men) under the age of 60 years using radiostereometric analysis.
Results
About two-thirds of the cemented implants and half of the uncemented implants stabilized between 2 and 10 years, while the remainder displayed a small annual increase of maximum total point motion of 0.09–0.10 mm/year. At 10 years there were no statistically significant differences in migration or clinical results between the groups.
Conclusion
Uncemented fixation with titanium fiber mesh coating of the femoral component in total knee arthroplasty works equally as well as cemented fixation up to 10 years. An annual migration of 0.1 mm seems compatible with excellent long-term performance.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The demands for total knee arthroplasty (TKA) in younger patients are increasing [1,2,3]. This group of patients has a more active way of life than older patients and a longer life expectancy which set higher requirements on the longevity of the implants. However, the results of TKA in younger patients are inferior mainly due to aseptic loosening [3,4,5].
Aseptic loosening of the femoral component seems to be less common than that of the tibial component. However, femoral loosening has been reported both for cemented [6,7,8] and uncemented [6] designs. Age of the patient seems to be important; Bozic et al. [9], in a large revision database, found that femoral component revisions were more commonly reported in patients aged 55–64 years compared to older patients.
The optimum mode of fixation of the femoral component is still uncertain. Despite good early fixation, cement monomer may be toxic and the curing heat creates damage to the bone [10, 11]. Osteolytic activity at the cement–bone interface has been found both in hip and knee replacement [12, 13]. On the other hand, uncemented fixation does not provide good early fixation, but stabilizes gradually and has been found beneficial for the fixation of tibial components in younger patients [14, 15]. Furthermore, cement debris is avoided and theoretically there is a potential for lasting, biological fixation. Also, retaining the prosthesis in case of infection seems more possible in uncemented designs [16].
Only three studies are found in the literature comparing uncemented (UC) and cemented (C) femoral component fixation in TKA using high-resolution techniques [17,18,19], all reporting results after 2 years. No long-term studies using high-resolution techniques have been published and indeed no long-term studies concerning younger patients. The importance of studying the pattern of migration over longer time periods has been stressed by Pijls et al. [20] stating that a particular migration pattern may be normal for one design or fixation, but pathological for another. Such studies have been performed for the tibial component in TKA [14, 21,22,23,24,25], whereas this has not been the case for the femoral component.
Some years ago, results using radiostereometric analysis (RSA) of femoral component fixation up to 2 years in patients younger than 60 years was presented and the type of fixation (cemented/uncemented) was randomized [17]. No differences in migration between cemented and uncemented fixation were found. This patient cohort has now been followed for 10 years and these results are presented here.
The purpose of this study was twofold: first, to assess the long-term pattern of migration for cemented and uncemented fixation of the femoral component in TKA; and second, to correlate this with the clinical result. The hypothesis is that there are no differences between the groups in either long-term migration or clinical results.
Materials and methods
This study was approved by the Ethics Committee of Umeå University (Um dns 03-004). The study was not registered since this was not common practice at the time for start of this study.
The recruitment process for the patients in the study has been described in detail in Gao et al. [17]. The patients were operated between 2003 and 2004 at Falu General Hospital, Sweden. Inclusion criteria were primary osteoarthritis (OA) or posttraumatic OA, age less than 60 years, and body weight less than 120 kg. Exclusion criteria were inflammatory arthropathy and malignancy. Forty-one patients (23 women and 18 men) were operated. The median age at operation was 55 (range 33–59) years. In six patients (two women and four men), both knees were operated during the same operation, however only the first operated knee (usually the right) was included in this study. All patients were operated by one of the authors (AH). The operations were performed through a midline parapatellar capsular incision. An intramedullary guide was used for the distal femoral cut, and extramedullary technique for the proximal tibial cut. A patella component was not routinely used, but was necessary in six patients (2 in the cemented group and 4 in the uncemented group). Indication for patella component was substantial erosion of patella with concave articular surface. The posterior cruciate ligament was retained in all cases, but balanced when necessary. In knees receiving cemented femoral components, the bone was irrigated with high-pressure lavage and thereafter dried before application of cement to obtain optimum cement interdigitation [26]. Vacuum-mixed Palacos bone cement with gentamicin (Schering Plough, Labo, Belgium) was used. The femoral component was kept under pressure while the cement was curing. Before inserting the femoral component, five to nine tantalum beads (1 mm in diameter) were inserted into the distal femoral metaphysis.
Randomization between cemented and uncemented fixation of the femoral component was performed at operation by opening a sealed opaque envelope. These envelopes had been prepared before commencement of the study, each envelope containing a leaflet with either “cement” or “no cement” printed. The envelopes were shuffled and then sequentially numbered and kept in a locker outside the operation ward. After the bony cuts had been made, ligament balancing and trial reduction had taken place, the randomization envelope was brought to the operation theater. The patients were blinded as to the type of fixation received.
A cobalt-chrome NexGen Cruciate Retaining (CR) Option (Zimmer, Warsaw, USA) femoral component with a commercially pure titanium fiber mesh under-surface was used in both groups. The fiber-metal coating consisted of a titanium alloy with 50% porosity and a pore size of 200–300 µm [27].
For the radiostereometric analysis (RSA), the femoral components were equipped by the manufacturer with four tantalum beads encased in titanium rods which were attached to the anterior and posterior flanges of the component (Fig. 1). Further, two tantalum beads in titanium rods were attached at the tip of the two pegs. These latter two markers were however difficult to visualize on the RSA radiographs and were, therefore, not used in the present study.
The NexGen Option CR femoral component was equipped by the manufacturer with four tantalum beads encased in titanium rods which were attached to the anterior and posterior parts of the component (arrows). Further, two tantalum beads in titanium rods were attached at the tip of the two pegs. These latter two markers were difficult to visualize on the RSA radiographs and were, therefore, not used in the present study
Due to logistical reasons, the tibial component in the first 22 patients operated was an uncemented monoblock trabecular metal cruciate retaining (CR) tibial component (Zimmer, Warsaw, USA), whereas in the last 19 patients operated, a cemented modular fixed bearing NexGen Option CR tibial component (Zimmer, Warsaw; USA) was used. The articular geometry of these two tibial implants was identical. The results of the tibial component fixation after 5 and 10 years of these patients have been presented previously [14, 23].
Postoperatively, all patients were allowed immediate full weight bearing with the assistance of two crutches for the first 6 weeks.
Measurement of implant migration was performed with radiostereometric analysis (RSA) using UmRSA software (v 6.0, RSA Biomedical, Umeå, Sweden). The initial RSA examination was performed at a mean of 4 (Standard Deviation, [SD] 2) days postoperatively, and thereafter at 6 weeks, 3, 12, and 24 months, and 10 years. The patients were examined supine using a bi-planar calibration cage (Cage 10, RSA Biomedical, Umeå Sweden). The upper limit for “mean error of rigid body fitting” (a measure of marker stability) was set at 0.30, and was in reality 0.23 (95% confidence interval [CI] 0.21–0.25) for the markers in femur and 0.09 (0.07–0.10) for the markers in the femoral component. The upper limit for the “condition number” (a measure of the quality of dispersion of the markers in each segment, the lower the better) was set at 100 and was in reality mean 72 (95% CI 63–81) for the femur, and 39 (37–41) for the femoral implant. There was a median (range) of five (3–8) markers visible in the femur and four in the implant.
The relative movements of the femoral component represented by its tantalum markers in relation to bone were measured using the markers in the femoral metaphysis as the fixed reference segment. The rotations of the femoral component were measured around the transverse (x), vertical (y) and sagittal (z) axes of the knee, respectively. The proportion of components displaying positive or negative values of rotation around the three axes (i.e. direction of rotation) was also calculated. The translations were expressed as migration of the geometrical midpoint (centroid) of the four femoral component tantalum markers along the three cardinal axes. Also, the vectorial length of the three-dimensional translation vector of the marker that moved the most was also measured (i.e. maximum total point motion, MTPM). For components displaying increasing MTPM between 2 and 10 years, the annual migration was calculated.
The repeatability of the RSA measurements was calculated using double examination obtained at all examinations up to 10 years as described by Ranstam et al. [28]. Significant rotations at the 95% significance level were > 0.37° (transverse), > 0.25° (longitudinal) and > 0.20° (sagittal). The corresponding values for x, y and z-translations were > 0.23, 0.26 and 0.32 mm, respectively.
The presence and size of radiolucent lines (RLL) were analyzed on the RSA radiographs as described by the Knee Society [29].
Clinical evaluation was performed using the knee, pain, and function score of the Knee Society [30].
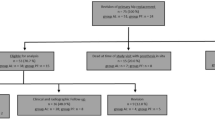
A flowchart of the study according to Consort is depicted in Fig. 2. In one uncemented knee, by mistake, there was no postoperative radiograph obtained which precluded further RSA investigations. This patient was, however, followed clinically up to 10 years.
Statistical analysis
Before any patients were enrolled into this study, a power calculation was performed. Based on the results of a previous RSA study on femoral component fixation [18], it was calculated that to find a difference in MTPM of 0.5 mm (SD 0.6) between the groups, a minimum of 18 patients per group were required with α = 0.05 and power = 0.80. To account for losses, 41 patients were randomized. As the initial plan was to follow the patients for 2 years, the present 10 year follow-up is formally a retrospective analysis of prospectively collected data.
Since the main interest of the study was the amount and progression of migration, only absolute values of parameters for which both negative and positive values were possible were analyzed (the sign being an indication of the direction of the movement).
The migration data were not normally distributed (tested by Shapiro–Wilk and Pearson’s tests for normality). Therefore, the median and interquartile range are presented. For comparison between groups at 10 years, Mann–Whitney U test was used. Wilcoxon signed rank test was used for comparison of change in migration between 2 and 10 years. Analysis of clinical parameters was done by Mann–Whitney U test.
Any p value < 0.05 was considered significant.
For patients with bilateral operations, only the first-operated knee was included in the statistical calculations.
Results
Between the 2-years examination and the follow-up at 10 years, six patients were lost to follow-up (Fig. 2). In the C group, one man had deceased, one man had moved abroad, one woman was revised due to knee instability following a fall, and one woman was too infirm to attend. In the UC group, one woman was deceased and one man was too sick to attend. No patient was revised due to loosening of either the femoral or tibial component.
Radiostereometry
There were no statistically significant differences in migration between the C and UC groups at 10 years (Table 1). The majority of the implants in both groups (70%) rotated externally, whereas rotation into flexion/extension and varus/valgus was more evenly distributed in both groups.
In both groups, the majority of the implants (> 80%) translated proximally. Translations along the other two axes were more evenly distributed in both groups. Either of the two markers on the posterior condyles displayed the largest MTPM in both groups.
The change in migration from 2 to 10 years for rotations and MTPM is shown in Figs. 3, 4, 5 and 6. About one-third of the C implants and half of the UC implants displayed increasing MTPM between 2 and 10 years with a mean annual migration of 0.10 (range 0.03–0.36) mm and 0.09 (range 0.06–0.19) mm, respectively.
Box plot displaying absolute values of rotation of the femoral component around the transverse axis of the knee (flexion/extension) at 2 and 10 years postoperatively in the cemented and uncemented groups. The line in the box represents the median, the box the inter-quartile range, and the whiskers the 10th and 90th percentiles. Change in migration between 2 and 10 years; cemented (n.s.), uncemented (n.s.) (Wilcoxon signed rank test)
Box plot displaying absolute values of rotation of the femoral component around the longitudinal axis of the knee (internal/external rotation) at 2 and 10 years postoperatively in the cemented and uncemented groups. For legend, see Fig. 2. Change in migration between 2 and 10 years; cemented (n.s.), uncemented (n.s.) (Wilcoxon signed rank test)
Box plot displaying absolute values of rotation of the femoral component around the sagittal axis of the knee (varus/valgus rotation) at 2 and 10 years postoperatively in the cemented and uncemented groups. For legend, see Fig. 2. Change in migration between 2 and 10 years; cemented (n.s.), uncemented (n.s.) (Wilcoxon signed rank test)
Box plot displaying maximum migration (MTPM) of the femoral component in the cemented and uncemented groups. For legend, see Fig. 2. Change in migration between 2 and 10 years; cemented (n.s.), uncemented p = 0.04 (Wilcoxon signed rank test)
Conventional radiography
The thin (< 1 mm) radiolucent lines (RLL) seen at the 2 years follow-up were unchanged in size and distribution at the 10 years follow-up. No new RLL developed between 2 and 10 years.
Clinical
At 10 years, there were no clinically relevant differences in Knee Society knee, pain or function scores, or in the range of knee motion between the two groups (Table 2).
Discussion
The most important finding in this study is that the small migration of the femoral component in total knee arthroplasty up to 10 years does not differ between uncemented and cemented designs. The annual increase in migration (MTPM) of 0.01 mm/year or less between 2 and 10 years is compatible with good long-term results with regard to fixation for both cemented and uncemented components. This is the first study to present the long-term pattern of migration of the cemented and uncemented femoral component in TKA of the NexGen design using RSA.
For the tibial component in TKA, RSA performed within the early postoperative years has been used to evaluate the quality of fixation between different designs of implants and fixation techniques. By combining short-term RSA data with long-term clinical follow-up studies, Pijls et al. found that the magnitude of the early migration between 1 and 2 years was associated with long-term risk for aseptic loosening of the tibial component [31]. To use short-term RSA-data as a prognostic tool for long-term fixation, however, requires that several short-term studies purposely are extended 5 to 10 or more years, since different types of designs or modes of fixation may differ in their pattern of migration [25]. In knee arthroplasty, this has been done for several designs of TKA and types of fixation [14, 21,22,23,24,25]. For the femoral component, on the other hand, no such studies had been published which motivated the authors to extend the follow-up of this randomized trial up to 10 years.
In the present study, about two-thirds of the C implants and half of the UC implants stabilized between 2 and 10 years, while the remainder displayed a small annual increase of MTPM of 0.09–0.10 mm/year. For the tibial component, an annual migration (MTPM) of < 0.20 mm/year between 1 and 2 years [32] or ≤ 0.10 mm/year between 2 and 5 years [33] has been found compatible with good long-term results. The good clinical outcome up to 10 years of the present study and the similar clinical results to that of Park and Kim [34] suggest that an annual migration rate (MTPM) of 0.09–0.10 mm may be acceptable for good long-term performance for the femoral component irrespective of the mode of fixation.
The type of surface coating or texture of the uncemented implant may be of importance. The femoral component of the present study as well as that of Nilsson et al. [18] and Park and Kim [34] had porous fiber titanium mesh coating, which seemed to work excellently. Other uncemented designs with clinical results equal to cemented design have been equipped with various types of porous coatings [7, 35,36,37,38,39] or hydroxyapatite coating [19, 40]. Smooth or grit blasted surface seems to result in inferior fixation [6].
The thin (< 1 mm) radiolucent lines (RLL) which had developed up to 2 years in about half of the implants in both groups [17] did not progress between 2 and 10 years. Radiolucent lines around the femoral component are difficult to determine, and the results vary in the literature. Park and Kim [34] found RLLs > 1 mm in only about 5% of the C and UC knees at 14 years follow-up, whereas Illgen et al. [37] reported radiolucent lines in the uncemented femoral components in about 13% at 10 years.
A limitation of the study is the small numbers of patients. However, no implants were revised for loosening and the results at 10 years were similar to those of 2 years. Another, theoretical, weakness would be the use of two different tibial components with different fixation. However, the articulating surfaces were identical which suggests similar forces on to the femoral component. The strengths of the study are several: randomization between cemented and uncemented fixation, investigation of younger patients using radiostereometry, and the long follow-up.
From a clinical perspective, it is safe to use the femoral component of NexGen design without cement.
Conclusion
Uncemented fixation with titanium fiber mesh coating of the femoral component in total knee arthroplasty works equally well as cemented fixation up to 10 years. An annual migration of 0.1 mm seems compatible with excellent long-term performance.
References
Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ (2009) Future young patient demand for primary and revision joint replacement. Clin Orthop Relat Res 467:2606–2612
Leskinen J, Eskelinen A, Huhtala H, Paavolainen P, Remes V (2012) The incidence of knee arthroplasty for primary osteoarthritis grows rapidly among baby boomers: a population-based study in Finland. Arthritis Rheum 64:744–753
W-Dahl A, Robertsson O, Lidgren (2010) Surgery for knee arthritis in younger patients: a Swedish Register Study. Acta Orthop 81:161–164
Gie TJ, Novak C, Sinner P, Ma W, Mehle S (2007) Knee arthroplasty in the young patient: survival in a community register. Clin Orthop Relat Res 464:83–87
Julin J, Jämsen E, Puolakka T, Konttinen Y, Moilanen T (2010) Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis: a follow-up study of 32,019 patients in the Finnish Arthroplasty Register. Acta Orthop 81:413–419
Chockalingam S, Scott G (2000) The outcome of cemented vs cementless fixation of a femoral component in total knee replacement (TKR) with the identification of radiological signs for the prediction of failure. Knee 7:233–238
Khaw FM, Kirk LMG, Morris RW, Gregg PJ (2002) A randomized, controlled trial of cemented versus cementless press-fit condylar total knee replacement. Ten-year survival analysis. J Bone Jt Surg Br 84:658–666
Pulido L, Abdel MP, Lewallen DG, Stuart MJ, Sanchez-Sotelo J, Hansen AD, Pagnano MW (2015) Trabecular metal tibial component were durable and reliable in primary total knee arthroplasty: a randomized clinical trial. Clin Orthop Relat Res 473:34–42
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51
Mjöberg B (1986) Loosening of the cemented hip prosthesis. The importance of heat injury. Acta Orthop Scand 57(Suppl 221):3–40
Stürup J, Nimb L, Kramhøft M, Jensen JS (1994) Effect of polymerization heat and monomers from acrylic cement on canine bone. Acta Orthop Scand 65:20–33
Bos I, Fredebold D, Diebold J, Löhrs U (1995) Tissue reaction to cemented hip sockets. Histologic and morphometric autopsy study of 25 acetabula. Acta Orthop Scand 66:1–8
Kim Y-H, Choi Y, Kim J-S (2010) Osteolysis in well-functioning fixed- and mobile-bearing TKAs in younger patients. Clin Orthop Relat Res 468:3084–3093
Henricson A, Nilsson KG (2016) Trabecular metal tibial component still stable at 10 years: an RSA study of 33 patients less than 60 years. Acta Orthop 87:504–510
Nilsson KG, Henricson A, Norgren B, Dalén T (2006) Uncemented HA-coated implant is the optimum fixation for TKA in the young patient. Clin Orthop Relat Res 448:129–139
Dixon P, Parish EN, Cross MJ (2004) Arthroscopic debridement in the treatment of the infected total knee arthroplasty. J Bone Jt Surg Br 86:39–42
Gao F, Henricson A, Nilsson KG (2009) Cemented versus uncemented fixation of the femoral component of the NexGen CR total knee replacement in patients younger than 60 years: a prospective randomized controlled RSA study. Knee 16:200–206
Nilsson KG, Kärrholm J, Linder L (1995) Femoral component migration in total knee arthroplasty: randomized study comparing cemented and uncemented fixation of the Miller–Galante I design. J Orthop Res 13:347–356
Uvehammer J, Kärrholm J, Carlsson L (2007) Cemented versus hydroxyapatite fixation of the femoral component of the Freeman–Samuelson total knee replacement: a radiostereometric analysis. J Bone Jt Surg Br 89:39–44
Pijls BG, Plevier JWM, Nelissen RGHH (2018) RSA migration of total knee replacements: a systematic review meta-analysis. Acta Orthop 89:320–328
van Hamersveld KT, Marang-van de Mheen PJ, Tsonaka R, Valstar ER, Toksvig-Larsen S (2017) Fixation and clinical outcome of uncemented peri-apatite-coated cemented total knee arthroplasty. Five-year follow-up of a randomized controlled trial using radiostereometric analysis (RSA). Bone Jt J 99:1467–1476
van Hamersveld KT, Marang-van de Mheen PJ, van der Heide HJ, van der Linden-van der Zwaag HMJ, Valstar ER, Nelissen RGHH (2018) Migration and clinical outcome of mobile-bearing versus fixed-bearing single-radius total knee arthroplasty: a randomized controlled trial. Acta Orthop 89:190–196
Henricson A, Rösmark D, Nilsson KG (2013) Trabecular metal tibial component still stable at 5 years: an RSA study of 36 patients less than 60 years. Acta Orthop 84:398–405
Nilsson KG, Kärrholm J, Carlsson L, Dalén T (1999) Hydroxyapatite coating versus cemented fixation of the tibial component in total knee arthroplasty. Prospective randomized comparison of hydroxyapatite-coated and cemented tibial components with 5-year follow-up using radiostereometry. J Arthroplasty 14:9–20
Pijls BG, Valstar ER, Kaptein BL, Fiocco M, Nelissen RGGH (2012) The beneficial effect of hydroxyapatite lasts: a randomized radiostereometric trial comparing hydroxyapatite-coated, uncoated, and cemented tibial components for up to 16 years. Acta Orthop 83:135–141
Vanlommel J, Luyckx JP, Labey L, Innocenti B, De Corte R, Bellemans J (2011) Cementing the tibial component in total knee arthroplasty: which technique is best? J Arthroplasty 26:492–496
Rahbek O, Kold S, Zippor B, Overgaard S, Søballe K (2005) The influence of surface porosity on gap-healing around intra-articular implants in presence of migrating particles. Biomaterials 26:4728–4736
Ranstam J, Ryd L, Önsten I (2000) Accurate accuracy measurement: review of basic principles. Acta Orthop Scand 71:106–108
Ewald F (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Pijls BG, Valstar ER, Nouta KA, Plevier JW, Fiocco M, Middeldorp S, Nelissen RGHH (2012) Early migration of tibial components is associated with late revision; a systemic review and meta-analysis of 21,000 knee arthroplasties. Acta Orthop 83:614–624
Ryd L, Albrektsson BE, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S (1995) Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Jt Surg Br 77:377–383
Wilson DAJ, Richardson G, Hennigar AW, Dunbar MJ (2012) Continued stabilization of trabecular metal tibial monoblock total knee arthroplasty components at 5 years—measured with radiostereometric analysis. Acta Orthop 83:36–40
Park JW, Kim YH (2011) Simultaneous cemented and cementless total knee replacement in the same patients: a prospective comparison of long term outcomes using an identical design of NexGen prosthesis. J Bone Jt Surg Br 93:1479–1486
Bouras T, Bitas V, Fennema P, Korovessis P (2017) Good long-term results following cementless TKA with a titanium plasma coating. Knee Surg Sports Traumatol Arthrosc 25:2801–2808
Demey G, Servien E, Lustig S, Selmi TAS, Neyret P (2011) Cemented versus uncemented femoral components in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1053–1059
Illgen R, Tueting J, Enright T, Schreibman K, McBeath A, Heiner J (2004) Hybrid total knee arthroplasty: a retrospective analysis of clinical and radiographic outcomes at average 10 years follow-up. J Arthroplasty 19:95–100
Kim Y-H, Park J-W, Lim H-M, Park E-S (2014) Cementless and cemented total knee arthroplasty in patients younger then fifty five years. Which is better? Int Orthop 38:297–303
Ritter MA, Meneghini R (2010) Twenty-year survivorship of cementless Anatomic Graduated Component total knee arthroplasty. J Arthroplasty 25:507–513
Epinette J-A (2014) Long lasting outcome of hydroxyapatite-coated implants in primary knee arthroplasty: a continuous series of two hundred and seventy total knee athroplasties at fifteen to twenty years of clinical follow-up. Int Orthop 38:305–3011
Funding
This study was supported by institutional grants from Zimmer and Umeå University, Umeå, Sweden.
Author information
Authors and Affiliations
Contributions
AH performed the surgery and the follow-ups, analyzed the data, and wrote and edited the manuscript. RW analyzed the data and wrote and edited the manuscript. SC analyzed the data and edited the manuscript. KGN initiated the study, analyzed data, and also wrote and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of Umeå University (Um dns 03-004)
Rights and permissions
About this article
Cite this article
Henricson, A., Wojtowicz, R., Nilsson, K.G. et al. Uncemented or cemented femoral components work equally well in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27, 1251–1258 (2019). https://doi.org/10.1007/s00167-018-5227-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5227-5