Abstract
Purpose
The purpose was to analyse the correlation between meniscal extrusion and position changes of the anterior horn and posterior horn after medial meniscal allograft transplantation.
Methods
Patients (n = 68) who underwent medial MAT were included. Anatomical positions of the anterior horn and posterior horn were measured, before and after surgery, using magnetic resonance images in the coronal and sagittal planes. The absolute and relative delta values of the anatomical positions were obtained, and the absolute and relative meniscal extrusion measurements were taken.
Results
In the coronal plane, the absolute position change of anterior horn showed moderate positive correlation with the absolute and relative meniscal extrusion. The relative position change of anterior horn showed moderate positive correlation with the absolute and relative meniscal extrusion. The absolute position change of posterior horn showed moderate positive correlation with the absolute and relative meniscal extrusion. The relative position change of posterior horn showed moderate positive correlation with the absolute and relative meniscal extrusion. In the sagittal plane, both absolute and relative position change of anterior horn showed no correlation with the absolute and relative meniscal extrusion, respectively. Both absolute and relative position changes of posterior horn showed nonsignificant weak correlation with the absolute and relative meniscal extrusion, respectively.
Conclusion
Transplanting the meniscus close to its native position may reduce subluxation in medial meniscal allograft transplantation. As position changes in the coronal plane can affect the meniscal subluxation more than changes in the sagittal plane, the tibial bone tunnel should be carefully created in the correct anatomical position to avoid a large amount of coronal deviation.
Level of evidence
Retrospective case series, IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Meniscal allograft transplantation (MAT) is a surgical treatment for restoration of the meniscus by transplanting the meniscal allograft to its native position. The transplanted meniscal allograft fills up the joint space and restores the biomechanics of the joint to approximately those of the normal knee. As a result, MAT reduces pain, improves knee function in appropriately indicated patients. It potentially delays degeneration of the articular cartilage in the affected compartment [5, 6, 11, 18, 19, 24, 26, 30].
However, previous studies revealed frequent occurrences of meniscal allograft extrusions following MAT [9, 14,15,16]. The area of the tibia that is protected by the meniscus is reduced when the meniscus extrudes beyond the edge of the tibial plateau. Therefore, the meniscus might not adequately absorb and distribute the weight-bearing load applied to the articular cartilage. This may reduce the expected benefits of MAT [1, 3]. Previous studies have attempted to determine the factors that cause meniscal allograft extrusion after MAT. Size mismatch between the knee joint and meniscal allograft, inappropriate fixation of the allograft, excessive peripheral suture tension, non-anatomic allograft placement, and preexisting osteophytes in the tibial plateau were determined to be possible risk factors for meniscal extrusion [4, 9, 13, 14]. However, the definitive cause and clinical significance of meniscal extrusion following MAT remains unclear.
After MAT, the meniscal anterior horn (AH) and the posterior horn (PH) may shift to other anatomical positions compared to their native anatomical positions. However, the effect of these anatomical position changes of both horns on the meniscal extrusion has not yet been clearly identified. The present study assessed these changes after MAT as a risk factor for meniscal extrusion. The authors analysed if there was a correlation between meniscal extrusion and anatomical position changes of both horns. The present study is the first to use magnetic resonance imaging (MRI) after MAT to directly measure the absolute and relative values of the amount of change in the position of the meniscal both horns and to analyse the correlations between such positional changes and meniscal extrusion.
Findings of this study might investigate the effect of anatomical position change of the meniscus on the meniscal extrusion. Therefore, it may emphasize the importance of anatomical restoration of the meniscus during MAT for successful result. The authors hypothesized that greater anatomical position changes of the AH and PH would be positively correlated with the meniscal extrusion.
Materials and methods
Patients that underwent medial MAT, using a bone-plug technique, from 1999 to 2014 at Seoul Asan medical center were included in this study. All MAT surgeries were performed by a single experienced surgeon who had performed more than 500 MAT surgeries. The indications for medial MAT included patients less than 55 years old, normal axial alignment of the lower extremities without apparent alignment deformity on standing radiographs, and persistent medial knee pain caused by the medial meniscal deficiency. The contraindications for medial MAT included extensive grade III or grade IV degenerative osteoarthritis, uncorrected knee instability, axial malalignment of the lower extremities, skeletal immaturity, and an age more than 55 years. However, localized grade III or IV articular cartilage degeneration, confined to the area covered by the meniscus, was not considered as a contraindication.
Preoperative sizing of the meniscal allograft
Sizing radiographs, including anteroposterior (AP) and lateral radiographs of the knee, were obtained before surgery for measurement of allograft size. All radiographs were obtained as true AP and lateral radiographs. We used a metallic 100-mm radio-opaque rod placed under fluoroscopy to correct for magnification and inaccurate bony measurement. Size of the medial meniscal allograft was measured according to the method described by Pollard et al. [21] Based on this method, lateral radiographs were used to measure sagittal length of the medial meniscus. Sagittal length of the medial meniscus was 80% of the sagittal tibial plateau (measured at the joint between a line parallel to the anterior tibia above the tibial tuberosity, and a line tangent to the posterior plateau margin perpendicular to the joint line). The medial meniscal width was equal to coronal length from the peak of the medial tibial eminence to medial margin of the tibial plateau on AP radiographs. After determining the appropriate size of the meniscal allograft, the desired meniscal size was communicated to the tissue bank (Cellumed, Seoul, Republic of Korea), which provided a fresh-frozen medial meniscal allograft that never exceeded a 5% mismatch of coronal or sagittal length.
Surgical technique
The bone plug of the PH was prepared with a diameter of 8 mm and that of the AH was prepared with a diameter of 10 mm. The bone plug of each meniscal horn was ligated using an unabsorbable suture, and the posteromedial side of the meniscus was sutured with two leading sutures. The space through the intercondylar notch was widened to allow easy passage of the PH by partially removing the bony intercondylar notch. The tibial tunnel was created from the anteromedial side of the proximal tibia to the anatomical center of the PH using a tibial tunnel guide which is used in anterior cruciate ligament (ACL) reconstruction. Afterward, to allow the sutures of the PH to pass through the tibial tunnel to the outside, a wire was passed through the tibial tunnel from outside to inside. In the posteromedial side of the knee, an accessory skin incision was made to access to the posteromedial capsule. An anterior arthrotomy was performed along the medial side of the patella and patellar tendon. Through the anterior arthrotomy, a wire was introduced to the posteromedial compartment and penetrated through the posteromedial capsule. Using the posteromedial approach, the leading sutures linked to the posteromedial side of the allograft were retrieved out of the joint. Using the wire that had already been introduced through the tibial tunnel, the sutures of the PH were pulled out of the tibia. Then the allograft was inserted through the anterior arthrotomy and the bone plug of the PH was introduced to the native PH footprint.
The conventional inside-out meniscal repair was performed on the PH and the mid-body of the meniscus. A tibial tunnel guide and a reamer were used to create the anterior tibial tunnel. The sutures of the AH were pulled out of the joint through the anterior tibial tunnel and the bone plug of the AH was fixed to the tunnel. Then the sutures of the AH and the PH that were already retrieved through the tibial tunnel were ligated together firmly. While viewing through an arthroscope to ensure that no excessive tension was applied, the leading sutures and each conventional inside-out sutures were firmly ligated. To prevent the extrusion of the meniscal allograft caused by excessive tension, ligation of each inside-out sutures was performed under direct visualization of the arthroscope. After optimal allograft positioning and seating in the joint were confirmed, the tension of ligation was applied until the allograft was not shifted to periphery of the joint. For the far anterior meniscal region, the outside-in meniscal repair technique was performed.
Patients used crutches the first 2 weeks after surgery to avoid weight-bearing activity. Weight-bearing activity was gradually increased to 50% of body weight 4 weeks post-surgery and to full weight-bearing after 6 weeks post-surgery.
MRI evaluation for the anatomical positions of the anterior horn and the posterior horn
The modified percentage reference method, developed by Wilmes et al. [28, 29] was used to measure the meniscal anatomical position. It provides a reproducible and precise determination of the meniscal tibial insertion. Although originally performed using plain radiographs, Kim et al. [7, 8] modified the method using magnetic resonance image (MRI). The modified method measures preoperative and postoperative positions of the meniscal AH and PH following MAT in coronal and sagittal planes [7, 8]. As knee size differs between patients, both the absolute and relative values of the meniscal horns were measured.
Anatomical positions of the AH and PH were evaluated using sagittal and coronal planes with a proton density-weighted fast spin echo MRI. Sagittal images were acquired with a 1.5 mm slice thickness, and coronal images were acquired in 2.5 mm slice thicknesses. A digital caliper in the picture archiving and communication system (PACS) was used for the MRI measurements.
A preoperative MRI was obtained a day before surgery and a postoperative MRI was obtained approximately 1 year after surgery for the evaluation of the meniscal horn positions. Patients were allowed to walk with full weight-bearing at the postoperative MRI. The knee joint was maintained in the same position during MRI examination; therefore, the bias resulting from different knee positions was avoided. The affected knee was fixed with a lower limb immobilizing device, flexed by 15°, and the patella was forward facing in all patients during examination.
Measurement of the anterior horn
The value for coronal position of the AH was obtained from an MRI crossing the midline of the knee on the coronal plane. Two parallel lines (line A: lateral; line B: medial) were drawn tangential to the lateral and medial border of the tibial plateau. Midpoint of the tibial attachment (point X) was marked on the other coronal MR image showing the broadest tibial attachment of the AH. The two images were merged using Adobe Photoshop software version 13.0.1 (Adobe Systems Inc., San Jose, CA). Absolute value for the coronal position of the AH was the distance between point X and line A. Relative values for the anatomical position of the AH were obtained by dividing the distance between point X and line A by the distance between line A and B on the merged image (Fig. 1).
On an MRI image crossing the midline of the knee on the coronal plane, two parallel lines (line A: lateral; line B: medial) were drawn tangential to the lateral and medial border of the tibial plateau. The midpoint of the tibial attachment (point X) was marked on a second coronal MRI image showing the broadest tibial attachment of the AH and the two images were merged. Absolute value for the coronal position of the AH was the distance between point X and line A. The relative values for the anatomical position of the AH were obtained by dividing the distance between point X and line A by the distance between lines A and B on the merged image. The border of the AH was demarcated with a yellow line
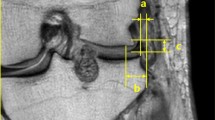
The value for sagittal position of the AH was obtained from an MRI crossing the midline of the knee on the sagittal plane. Line A was drawn parallel to the anterior border of the tibial plateau, and line B was drawn tangential to the bony ridge of the posterior intercondylar area and parallel to the tibial shaft. Line C was drawn perpendicular to line B and tangential to the medial intercondylar spine. Reference point a was at the intersection of lines A and C. Reference point b was at the intersection of line B and line C. The midpoint of the AH (point X) was marked on the other sagittal image showing the broadest tibial attachment of the AH. The two images were merged. Absolute value for the sagittal position of the AH was the distance between points a and X. Relative value for the anatomical position of the AH was obtained by dividing the distance between points a and X by the distance between points a and b. (Fig. 2).
On an MRI image crossing the midline of the knee on the sagittal plane, line A was drawn parallel to the anterior border of the tibial plateau, and line B was drawn tangential to the bony ridge of the posterior intercondylar area and parallel to the tibial shaft. Line C was drawn perpendicular to line B and tangential to the medial intercondylar spine. Reference point A was at the intersection of lines A and C. The midpoint of the AH (point X) was marked on a second sagittal image showing the broadest tibial attachment of the AH. The two images were merged and the absolute value for the sagittal position of the AH was the distance between points A and X. Relative values for the anatomical position of the AH were obtained by dividing the distance between points A and X by the distance between points A and B. The border of the AH was demarcated with a yellow line
The value for postoperative coronal position of the AH was obtained from an MRI crossing the midline of the knee on the coronal plane. Two parallel lines (line A: lateral; line B: medial) were drawn tangential to the lateral and medial border of the tibial plateau. Midpoint of the AH bone plug (point X) was marked on the other coronal MR image showing the broadest AH bone plug. The two images were merged. Absolute value for the coronal position of the AH was the distance between point X and line A. Relative values for the anatomical position of the AH were obtained by dividing the distance between point X and line A by the distance between lines A and B on the merged image.
The value for postoperative sagittal position of the AH was obtained from an MRI crossing the midline of the knee on the sagittal plane. Line A was drawn parallel to the anterior border of the tibial plateau, and line B was drawn tangential to the bony ridge of the posterior intercondylar area and parallel to the tibial shaft. Line C was drawn perpendicular to line B and tangential to the medial intercondylar spine. Reference point a was at the intersection of lines A and C. Reference point b was at the intersection of line B and line C. The midpoint of the AH bone plug (point X) was marked on the other sagittal image showing the broadest AH bone plug. The two images were merged. Absolute value for the sagittal position of the AH was the distance between points a and X. Relative value for the anatomical position of the AH was obtained by dividing the distance between points a and X by the distance between points a and b.
Measurement of the posterior horn
The value for the coronal position of the PH was obtained from an MRI crossing the midline of the knee on the coronal plane. Two parallel lines (line A: lateral; line B: medial) were drawn tangential to the lateral and medial border of the tibial plateau. Midpoint of the PH (point Y) was marked on a coronal MRI showing the broadest tibial attachment of the PH. The two images were merged. Absolute value for the coronal position of the PH was the distance between point Y and line A. Relative values for the anatomical position of the PH were obtained by dividing the distance between point Y and line A by the distance between line A and B on the merged image (Fig. 3).
On an MRI image crossing the midline of the knee on the coronal plane, two parallel lines (line A: lateral; line B: medial) were drawn tangential to the lateral and medial border of the tibial plateau. The midpoint of the tibial attachment (point Y) was marked on a second MRI image showing the broadest tibial attachment of the PH. The two images were merged. The absolute value for the coronal position of the PH was the distance between point Y and line A. Relative values for the anatomical position of the PH were obtained by dividing the distance between point Y and line A by the distance between lines A and B on the merged image. The border of the PH was demarcated with a yellow line
The value for the sagittal position of the PH was obtained from an MRI crossing the midline of the knee on the sagittal plane. Line A was drawn parallel to the anterior border of the tibial plateau and line B was drawn tangential to the bony ridge of the posterior intercondylar area and parallel to the tibial shaft. Line C was drawn perpendicular to line B and tangential to the medial intercondylar spine. Reference point a was at the intersection of lines A and C. Reference point b was at the intersection of lines B and line C. The midpoint of the tibial attachment (point Y) was marked on the other sagittal MRI showing the broadest tibial attachment of the PH. The above two images were merged. Absolute value for the sagittal position of the PH was the distance between points a and Y. Relative values for the anatomical position of the PH were obtained by dividing the distance between points a and Y by the distance between points a and b (Fig. 4).
On an MRI image crossing the midline of the knee on the sagittal plane, line A was drawn parallel to the anterior border of the tibial plateau, and line B was drawn tangential to the bony ridge of the posterior intercondylar area and parallel to the tibial shaft. Line C was drawn perpendicular to line B and tangential to the medial intercondylar spine. Reference point A was at the intersection of lines A and C. The midpoint of the tibial attachment (point Y) was marked on a second sagittal MRI showing the broadest tibial attachment of the PH. The above two images were merged and the absolute value for the sagittal position of the PH was the distance between points A and Y. Relative values for the anatomical position of the PH were obtained by dividing the distance between points A and Y by the distance between points A and B. The border of the PH was demarcated with a yellow line
The value for postoperative coronal position of the PH was obtained from an MRI crossing the midline of the knee on the coronal plane. Two parallel lines (line A: lateral; line B: medial) were drawn tangential to the lateral and medial border of the tibial plateau. Midpoint of the PH bone plug (point Y) was marked on a coronal MRI showing the broadest PH bone plug. The two images were merged. Absolute value for the coronal position of the PH was the distance between point Y and line A. Relative values for the anatomical position of the PH were obtained by dividing the distance between point Y and line A by the distance between lines A and B on the merged image.
The value for postoperative sagittal position of the PH was obtained from an MRI crossing the midline of the knee on the sagittal plane. Line A was drawn parallel to the anterior border of the tibial plateau, and line B was drawn tangential to the bony ridge of the posterior intercondylar area and parallel to the tibial shaft. Line C was drawn perpendicular to line B and tangential to the medial intercondylar spine. Reference point a was at the intersection of lines A and C. Reference point b was at the intersection of line B and line C. The midpoint of the PH bone plug (point Y) was marked on the other sagittal MRI showing the broadest PH bone plug. The above two images were merged. Absolute value for the sagittal position of the PH was the distance between points a and Y. Relative values for the anatomical position of the PH were obtained by dividing the distance between points a and Y by the distance between points a and b.
MRI evaluation of the meniscal subluxation
Meniscal subluxation caused by inappropriate fixation of the allograft or excessive peripheral suture tension may occur immediately following MAT. Therefore, the meniscal subluxation was measured at two time points, 2 days and 1 year after surgery. The digital caliper in PACS was used for measurements on MR images. Length of subluxation beyond the margin of tibial articular cartilage might differ among MRIs. Therefore, an image showing the longest subluxation was used for measurement. Meniscal subluxation was measured using the method described by Verdonk et al. [23]. In the coronal plane, the amount of meniscal subluxation was defined as the distance between the outer margin of the proximal tibial plateau at the proximal articular surface and the outer edge of the subluxated meniscus. The absolute value of subluxation ‘a’ was defined as the portion of the meniscus that was displaced beyond the outer margin of the proximal tibial plateau. Due to varying knee sizes among individual patients, the amount of meniscal subluxation was reported as a relative value as well as an absolute value for standardization. The relative value of meniscal subluxation was defined as the relative percentage of extrusion (RPE), calculated as the absolute value of the subluxated portion of the meniscus ‘a’ divided by the absolute value of the entire meniscal width ‘b’ (Fig. 5).
The absolute value of subluxation ‘a’ was defined as the portion of the meniscus that was displaced beyond the outer margin of the proximal tibial plateau. The relative value of meniscal subluxation was defined as the relative percentage of extrusion, which was calculated as the absolute value of the subluxated portion of the meniscus ‘a’ divided by the absolute value of the entire meniscal width ‘b’
Comparing the pre- and postoperative anatomical position of the meniscus
As described earlier, absolute and relative values of the anatomical positions of both horns in coronal and sagittal planes were determined. The mean delta values of the AH and PH in coronal and sagittal planes from each patient was calculated by subtracting the value of the pre-surgical position from that of the post-surgical position. Based on these calculations, degree of anatomical position changes of both horns were obtained.
In the coronal plane, the position of the meniscal horns relative to the vertical line tangent to the margin of the lateral tibial plateau was measured. If there was a positive difference (pre-surgical value subtracted from the post-surgical value), the meniscal horn had moved in the medial direction after surgery. In contrast, if there was a negative difference, the meniscal horn had moved in the lateral direction after surgery. In the sagittal plane, the position of the meniscal horns relative to the anterior reference point was measured. If there was a positive difference (pre-surgical value subtracted from the post-surgical value), the meniscal horn had moved in a posterior direction. In contrast, if there was a negative difference, the horn had moved in an anterior direction.
This study was approved by University of Ulsan, Seoul Asan medical center (ID number of approval: 2016-1283).
Statistical analysis
According to previous study, correlation between meniscal extrusion and the anatomical position change was approximately 0.3 [14]. Based on our clinical experience, post-power calculations were performed assuming that the correlations were 0.3, 0.35, 0.4, 0.45, and 0.5, respectively. As a result, the power was 0.39, 0.51, 0.63, 0.75 and 0.85 at the significance level of 0.05. That meant that we had enough power only when the correlation was close to 0.5 [2]. This is consistent with the analysis results in the text.
Absolute values and RPEs of meniscal subluxation immediately after surgery and 1 year after surgery were statistically compared. A paired t test was used to compare the values between the two time points. p < 0.05 was considered statistically significant.
Correlation was determined using the Pearson correlation coefficient between the degree of the meniscal allograft subluxation and the position change of both horns in sagittal and coronal planes following MAT. SPSS version 16.0 for Windows (SPSS, Chicago, IL) was used for the statistical analysis. A Pearson correlation coefficient (r) between + 1 and + 0.7 indicates a strong positive linear relationship, between + 0.7 and + 0.3 indicates a moderate positive linear relationship, and between + 0.3 and + 0.1 indicates a weak positive linear relationship. A value between − 0.1 and 0.1 indicates no correlation between two factors. A value between − 0.1 and − 0.3 indicates a weak negative linear relationship, between − 0.3 and − 0.7 indicates a moderate negative linear relationship, and between − 0.7 and − 1 indicates a strong negative linear relationship [20].
The MRI evaluation and measurements were performed by two orthopaedic surgeons. They measured the anatomical position of both horns and the meniscal subluxation independently. The results of measurement were completely blinded to each other to minimize the interobserver bias.
Each surgeon also performed the measurement twice at an interval of a month to minimize the intra-observer bias. The results of measurement used for statistical analysis were the mean value of the both measurements.
For assessment of the reliability of the measured values from the two observers, the study used the intraclass correlation coefficient (ICC), which quantifies the proportion of the difference due to measurement variability. The criteria for the reliability of the measured values using the ICC were as follows: less than 0.5—poor; between 0.5 and 0.75—moderate; between 0.75 and 0.9—good; more than 0.9—excellent [10]. The ICC values of pre- and postoperative meniscal anterior and posterior horn positions and meniscal subluxation measured by the two observers are as follows. The mean ICC for interobserver reliability of the preoperative AH position was 0.78 in the coronal plane and 0.79 in the sagittal plane. The mean ICC for interobserver reliability of the postoperative AH position was 0.81 in the coronal plane and 0.78 in the sagittal plane. The mean ICC for intra-observer reliability of the preoperative AH position was 0.88 in the coronal plane and 0.83 in the sagittal plane. The mean ICC for intra-observer reliability of the postoperative AH position was 0.87 in the coronal plane and 0.86 in the sagittal plane.
The mean ICC for interobserver reliability of the preoperative PH position was 0.74 in the coronal plane and 0.77 in the sagittal plane. The mean ICC for interobserver reliability of the postoperative PH position was 0.82 in the coronal plane and 0.79 in the sagittal plane. The mean ICC for intra-observer reliability of the preoperative PH position was 0.85 in the coronal plane and 0.89 in the sagittal plane. The mean ICC for intra-observer reliability of the postoperative PH position was 0.91 in the coronal plane and 0.85 in the sagittal plane.
The mean ICC for interobserver and intra-observer reliabilities of the meniscal subluxation were 0.91 and 0.9, respectively.
Results
76 patients underwent medial MAT using a bone-plug technique from 1999 to 2014 at the authors’ institution. Eight of those patients did not have a postoperative MRI 1 year after surgery and were excluded from the study. 68 patients (56 males and 12 females) were included in the present study. The mean age of the participants was 34.8 (standard deviation, SD 9.4) years.
The right knee was affected in 36 (52.9%) patients and the left knee was affected in 32 (47.1%) patients. 24 (35.3%) patients had a previous medial meniscal repair on the ipsilateral knee, 46 (67.7%) of the patients underwent a primary or revision reconstruction of the ACL, and the remaining 3 (4.4%) patients previously underwent a reconstruction of the posterior cruciate ligament on the ipsilateral knee. However, none of the patients had undergone a previous medial or lateral MAT on the ipsilateral knee (Table 1).
Anatomical position change of the anterior horn
In the coronal plane, the mean absolute delta value of the AH position was 5.9 (SD 4.4, range − 4.0 to 16.6) mm. Therefore, the AH of the meniscal allograft shifted medially by a mean value of 5.9 mm, after medial MAT compared with the native medial meniscus. The mean relative delta value of the AH position was 5.9 (SD 4.8, range − 4.9 to 17.5)%. Therefore, the AH of the meniscal allograft shifted medially by a mean value of 5.9%, after medial MAT compared with the native medial meniscus.
In the sagittal plane, the mean absolute delta value of the AH position was 4.3 (SD 2.8, range − 0.8 to 12.2) mm. Therefore, the AH of the allograft shifted posteriorly by a mean value of 4.3 mm after medial MAT compared with the native medial meniscus. The mean relative delta value of the AH position was 6.5 (SD 3.9, range − 1.3 to 18.6)%. Therefore, the AH of the allograft shifted posteriorly by a mean value of 6.5% after medial MAT compared with the native medial meniscus (Table 2).
Anatomical position change of the posterior horn
In the coronal plane, the mean absolute delta value of the PH position was 2.5 (SD 2.5, range − 2.8 to 8.4) mm. Therefore, the PH of the allograft shifted medially by a mean value of 2.5 mm, after medial MAT compared with the native medial meniscus. The mean relative delta value of the PH position was 2.2 (SD 2.8, range − 6.4 to 9.1)%. Therefore, the PH of the meniscal allograft shifted medially by a mean value of 2.2%, after medial MAT compared with the native medial meniscus.
In the sagittal plane, the mean absolute delta value of the PH position was 1.7 (SD 2.5, range − 3.0 to 10.9) mm. Therefore, the PH of the allograft shifted posteriorly by a mean value of 1.7 mm after medial MAT compared with the native medial meniscus. The mean relative delta value of the PH position was 2.9 (SD 4.6, range − 5.4 to 12.6)%. Therefore, the PH of the allograft shifted posteriorly by a mean value of 2.9%, after medial MAT compared with the native medial meniscus (Table 3).
Subluxation of the meniscal allograft
The mean absolute value of the meniscal subluxation was 2.8 (SD 1.5, range − 2.2 to 5.8) mm, and the mean RPE of the meniscal subluxation was 25.7 (SD 13.9, range − 15.3 to 50.2)% 2 days after surgery. The mean absolute value of the meniscal subluxation was 2.9 (SD 1.6, range − 2.6 to 6.0) mm, and the mean RPE of the meniscal subluxation was 26.5 (SD 14.4, range − 18.8 to 49.6)% 1 year after surgery.
The mean absolute value of the meniscal subluxation was not significantly different between 2 days and 1 year after surgery (p > 0.05, n.s.). The mean RPE was also not significantly different between 2 days and 1 year after surgery (n.s.).
Correlation between meniscal subluxation and the absolute anatomical position change of both horns
In the coronal plane, the Pearson correlation coefficient (r) between the absolute value of meniscal extrusion and the absolute delta value of the AH position was 0.54 (p < 0.01), and the Pearson correlation coefficient between the RPE and the absolute delta value of the AH position was 0.58 (p < 0.01) (Fig. 6). In the sagittal plane, there was no significant correlation between the absolute value of meniscal extrusion and the absolute delta value of the AH position (r = 0.01, n.s.), and between the RPE and the absolute delta value of the AH position (r = 0.06, n.s.), respectively.
In the coronal plane, the Pearson correlation coefficient (r) between the absolute value of meniscal extrusion and the absolute delta value of the PH position was 0.58 (p < 0.01), and the Pearson correlation coefficient between the RPE and the absolute delta value of the PH position was 0.47 (p < 0.01). (Fig. 7). In the sagittal plane, there was no significant correlation between the absolute value of meniscal extrusion and the absolute delta value of the PH position (r = 0.15, n.s.), and between the RPE and the absolute delta value of the PH position (r = 0.13, n.s.), respectively.
Correlation between meniscal subluxation and the relative anatomical position change of both horns
In the coronal plane, the Pearson correlation coefficient (r) between the absolute value of meniscal extrusion and the relative delta value of the AH position was 0.41 (p < 0.01), and the Pearson correlation coefficient between the RPE and the relative delta value of the AH position was 0.42 (p < 0.01) (Fig. 8). In the sagittal plane, there was no significant correlation between the absolute value of meniscal extrusion and the relative delta value of the AH position (r = − 0.03, n.s.), and between the RPE and the relative delta value of the AH position (r = 0.03, n.s.), respectively.
In the coronal plane, the Pearson correlation coefficient (r) between the absolute value of meniscal extrusion and the relative delta value of the PH position was 0.54 (p < 0.01), and the Pearson correlation coefficient between the RPE and the relative delta value of the PH position was 0.43 (p < 0.01) (Fig. 9). In the sagittal plane, there was no significant correlation between the absolute value of meniscal extrusion and the relative delta value of the PH position (r = 0.13, n.s.), and between the RPE and the relative delta value of the PH position (r = 0.16, n.s.), respectively.
Discussion
The most important finding of this study was that deviation of the AH and PH in the coronal plane positively affected the meniscal extrusion after medial MAT. The results show there was a moderate positive correlation between the meniscal extrusion and the position change of the AH and PH in the coronal plane.
Extrusion of the native meniscus is caused by degeneration of the articular cartilage or meniscus. Injury of the meniscus alters the matrix integrity of collagen fibres, which decreases the radial stiffness of the meniscus. This histological change causes extrusion of the meniscus beyond the articular margin. If extrusion displaces the meniscus to an abnormal anatomical position, the amount of articular cartilage, not protected by the meniscus, increases.
Wang et al. [27] reported that meniscal extrusion was significantly associated with reduced tibial cartilage volume, increased tibial plateau area, increased prevalence of subchondral bone marrow lesions, and bone cysts in both the medial and lateral compartments.
Meniscal extrusion occurs in knee joints after MAT as well as in native knee joints [12, 22]. Several preoperative or intraoperative factors are associated with these allograft extrusions after MAT. In a study by Jeon et al. [4], 88 patients with tibial osteophytes in the lateral compartment underwent lateral MAT. Of these, 44 underwent osteophyte excision along with MAT, whereas the remaining 44 only underwent MAT. The absolute meniscal extrusion was significantly greater in the non-excision group at 1 year after surgery. They found that osteophytes in the tibial plateau were associated with postoperative meniscal allograft extrusion. Lee et al. [14] analysed the correlation between meniscal allograft extrusion and bony trough obliquity on axial MRI after lateral MAT. Results showed increased risk of graft extrusion as the trough angle on the axial plane increased. An increased trough angle on the axial plane was associated with non-anatomic lateral placement of the posterior horn. Lee et al. [17] compared the meniscal extrusion between standard rehabilitation group with immobilization for 5–7 days and delayed rehabilitation group with immobilization for the first 3 weeks. They found that delayed rehabilitation showed less coronal graft extrusion, compared with standard rehabilitation.
Several factors have been associated with postoperative extrusion; however, no studies have directly analysed the association between allograft extrusion and the change in anatomic location of the meniscal AH and PH before and after surgery. To our knowledge, this is the first study to analyse the correlation of meniscal extrusion after calculating delta values by comparing the anatomical locations of both horns before and after surgery in the coronal and sagittal planes. Based on the results of this study, change in location of the AH and PH in the coronal plane showed a positive correlation with meniscal extrusion. This implies that close restoration to the original anatomic location of the native meniscus during MAT is helpful to prevent meniscal extrusion.
In MAT, non-anatomic placement of the meniscal horn compared to the native anatomic position might adversely alter the contact mechanics of the knee, which might affect the ability of a meniscal transplant to prevent cartilage degeneration [25]. Considering the adverse biomechanical alteration due to non-anatomic placement of the meniscal allograft and the positive correlations between meniscal position change and meniscal extrusion found in this study, the goal of MAT should be to reconstruct the meniscus as close as possible to the native anatomical position. Shifts of the AH and PH in the coronal plane can directly displace the mid-body of the meniscus laterally or medially compared with shifts in the sagittal plane. Therefore, the meniscal allograft should be placed as close to its native position as possible, especially, in the coronal plane.
In the case of the AH, the position of the anterior bone plug is dependent on the position of the posterior bone plug. If the posterior bone plug has already shifted from the native position, the anterior bone plug has a greater chance of similar deviation. Therefore, correct placement of the posterior bone plug is critical for anatomic restoration of the meniscus. The remnants of the native PH occupy a broad area, and its distinction from surrounding tissue is unclear; thus, it is difficult to determine the precise midpoint of the native PH under an arthroscope. Several anatomic structures might disturb appropriate insertion, placement, and maintenance of the guide during MAT. Thus, it is technically demanding to insert and place the guide in the center of the native PH footprint [8].
The present study has several limitations. First, a relatively small number of patients were included in this study. Second, even though this study found a correlation between anatomical position change of the meniscus and meniscal extrusion, the effect of the present study on clinical outcome was not analysed. Therefore, further studies performed with a longer follow-up period and clinical evaluation might be required. Third, the mean absolute delta value of PH was 2.5 mm in coronal plane and 1.7 mm in the sagittal plane. In this study, however, magnetic resonance images were acquired with a 1.5-mm slice thickness in sagittal plane and 2.5-mm slice thicknesses in the coronal plane. Therefore, slice thickness might be a limitation for measurement of the anatomical position of the meniscal horn.
Conclusion
Transplanting the meniscus close to its native position may reduce subluxation in medial MAT. As position change in the coronal plane can affect the meniscal subluxation more than changes in the sagittal plane, the tibial bone tunnel should be carefully created in the correct anatomical position to avoid a large amount of coronal deviation.
Change history
18 December 2018
The article Meniscal extrusion is positively correlated with the anatomical position changes of the meniscal anterior and posterior horns, following medial meniscal allograft transplantation.
References
Emmanuel K, Quinn E, Niu J, Guermazi A, Roemer F, Wirth W et al (2016) Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis—data from the osteoarthritis initiative. Osteoarthritis Cartilage 24:262–269
Guenther WC (1977) Desk calculation of probabilities for the distribution of the sample correlation coefficient. Am Stat 31:45–48
Guermazi A, Eckstein F, Hayashi D, Roemer FW, Wirth W, Yang T et al (2015) Baseline radiographic osteoarthritis and semi-quantitatively assessed meniscal damage and extrusion and cartilage damage on MRI is related to quantitatively defined cartilage thickness loss in knee osteoarthritis: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage 23:2191–2198
Jeon B, Kim JM, Kim JM, Lee CR, Kim KA, Bin SI (2015) An osteophyte in the tibial plateau is a risk factor for allograft extrusion after meniscus allograft transplantation. Am J Sports Med 43:1215–1221
Kim JH, Lee S, Ha DH, Lee SM, Jung K, Choi W (2018) The effects of graft shrinkage and extrusion on early clinical outcomes after meniscal allograft transplantation. J Orthop Surg Res 13:181–187
Kim JM, Lee BS, Kim KH, Kim KA, Bin SI (2012) Results of meniscus allograft transplantation using bone fixation: 110 cases with objective evaluation. Am J Sports Med 40:1027–1034
Kim NK, Bin SI, Kim JM, Lee CR (2016) Does lateral meniscal allograft transplantation using the keyhole technique restore the anatomic location of the native lateral meniscus? Am J Sports Med 44:1744–1752
Kim NK, Bin SI, Kim JM, Lee CR (2015) Does medial meniscal allograft transplantation with the bone-plug technique restore the anatomic location of the native medial meniscus? Am J Sports Med 43:3045–3054
Kim YS, Kang KT, Son J, Kwon OR, Choi YJ, Jo SB et al (2015) Graft extrusion related to the position of allograft in lateral meniscal allograft transplantation: biomechanical comparison between parapatellar and transpatellar approaches using finite element analysis. Arthroscopy 31:2380–2391
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Lee AS, Kang RW, Kroin E, BVerma NK, Cole BJ (2012) Allograft meniscus transplantation. Sports Med Arthrosc Rev 20:106–114
Lee DH (2018) Incidence and extent of graft extrusion following meniscus allograft transplantation. Biomed Res Int 2018:5251910
Lee DH, Kim JM, Jeon JH, Cha EJ, Bin SI (2015) Effect of sagittal allograft position on coronal extrusion in lateral meniscus allograft transplantation. Arthroscopy 31:266–274
Lee DH, Kim JM, Lee BS, Kim KA, Bin SI (2012) Greater axial trough obliquity increases the risk of graft extrusion in lateral meniscus allograft transplantation. Am J Sports Med 40:1597–1605
Lee DH, Kim SB, Kim TH, Cha EJ, Bin SI (2010) Midterm outcomes after meniscal allograft transplantation: comparison of cases with extrusion versus without extrusion. Am J Sports Med 38:247–254
Lee DH, Lee CR, Jeon JH, Kim KA, Bin SI (2015) Graft extrusion in both the coronal and sagittal planes is greater after medial compared with lateral meniscus allograft transplantation but is unrelated to early clinical outcomes. Am J Sports Med 43:213–219
Lee DW, Lee JH, Kim DH, Kim JG (2018) Delayed rehabilitation after lateral meniscal allograft transplantation can reduce graft extrusion compared with standard rehabilitation. Am J Sports Med 46:2432–2440
Lee DW, Park JH, Chung KS, Ha JK, Kim JG (2017) Arthroscopic medial meniscal allograft transplantation with modified bone plug technique. Arthrosc Tech 6:e1437–e1442
Mahmoud A, Young J, Bullock-Saxton J, Myers P (2018) Meniscal allograft transplantation: the effect of cartilage status on survivorship and clinical outcome. Arthroscopy 34:1871–1876
Mukaka MM (2012) A guide to appropriate use of correlation coefficient in medical research. Malawi Med J 24:69–71
Pollard ME, Kang Q, Berg EE (1995) Radiographic sizing for meniscal transplantation. Arthroscopy 11:684–687
Saltzman BM, Cotter EJ, Stephens JP, Cvetanovich GL, Madden B, Wang K et al (2018) Preoperative tibial subchondral bone marrow lesion patterns and associations with outcomes after isolated meniscus allograft transplantation. Am J Sports Med 46:1175–1184
Verdonk P, Depaepe Y, Desmyter S, De Muynck M, Almqvist KF, Verstraete K et al (2004) Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc 12:411–419
Verdonk R, Volpi P, Verdonk P, Bracht HVD, Laer MV, Almqvist KF et al (2013) Indications and limits of meniscal allografts. Injury 44:S21–S27
von Lewinski G, Kohn D, Wirth CJ, Lazovic D (2008) The influence of nonanatomical insertion and incongruence of meniscal transplants on the articular cartilage in an ovine model. Am J Sports Med 36:841–850
Vundelinckx B, Vanlauwe J, Bellemans J (2014) Long-term Subjective, clinical, and radiographic outcome evaluation of meniscal allograft transplantation in the knee. Am J Sports Med 42:1592–1599
Wang Y, Wluka AE, Pelletier JP, Martel-Pelletier J, Abram F, Ding C et al (2010) Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees. Rheumatology 49:997–1004
Wilmes P, Anagnostakos K, Weth C, Kohn D, Seil R (2008) The reproducibility of radiographic measurement of medial meniscus horn position. Arthroscopy 24:660–668
Wilmes P, Lorbach O, Weth C, Kohn D, Seil R (2011) Radiographic guided drilling of bony tibial tunnels for fixation of meniscus transplants using percentage references. Knee Surg Sports Traumatol Arthrosc 19:168–173
Zhang H, Chen S, Qiu M, Zhou A, Yan W, Zhang J (2018) Lateral meniscus allograft transplantation with platelet-rich plasma injections: a minimum two-year follow-up study. Knee 25:568–576
Funding
No external funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
The original version of this article was revised: Due to a retrospective Open Access cancellation.
Rights and permissions
About this article
Cite this article
Kim, NK., Bin, SI., Kim, JM. et al. Meniscal extrusion is positively correlated with the anatomical position changes of the meniscal anterior and posterior horns, following medial meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc 27, 2389–2399 (2019). https://doi.org/10.1007/s00167-018-5195-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5195-9