Abstract
Purpose
To investigate the risk factors for residual pivot shift test after anterior cruciate ligament (ACL) reconstruction based on a multicenter prospective cohort study.
Methods
This study included patients who were registered in the Multicenter Arthroscopic Knee Surgery Study, a prospective longitudinal multicenter cohort study, and who underwent primary ACL reconstruction using autologous hamstring tendon graft between 2013 and 2016. The exclusion criteria included prior injuries or surgeries in the contralateral knee, prior ligamentous injuries in the involved knee, grade 2 or 3 concomitant ligament injuries, and inflammatory or other forms of osteoarthritis. Data from the preoperative period and at 1-year follow-up were used for further analysis, and patients with incomplete data, re-injury and loss to follow-up were also excluded. Logistic regression analysis was conducted with age, gender, Lachman test, pivot shift test, KT measurement, hyperextension, single-bundle vs. double-bundle, meniscus injury sites, and meniscus treatments as the independent variables, and postoperative pivot shift test was used as the dependent variable.
Results
Three hundred and sixty-eight patients were included in the study. Hyperextension knee (P = 0.025) and a preoperative pivot shift test under anesthesia (P = 0.040) were identified as risk factors for a postoperative pivot shift via logistic regression analysis. There were no statistically significant differences in the other variables.
Conclusions
The results from a multicenter cohort study indicated that knee hyperextension and greater preoperative pivot shift under anesthesia were risk factors for residual pivot shift at 1 year after ACL reconstruction. In cases with a preoperative high-grade pivot shift and knee hyperextension, additional anterolateral structure augmentation might be considered in order to eliminate pivot shift and eventually obtain better outcomes after ACL reconstruction.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical results after anterior cruciate ligament (ACL) reconstruction are considered successful as anterior stability is restored. However, even though anterior stability was successfully restored in the majority of patients, anterolateral rotatory instability (ALRI) remains after reconstruction in some patients [8]. This may cause limitations in regular daily activities and in the ability of athletes to participate in sports. The ALRI is a likely reason why some athletes are unable to return to their pre-injury activity level, or why some experience limited performance [10, 19, 25, 32]. Dynamic ALRI in ACL-injured knees is commonly evaluated by the pivot shift test, which has a higher specificity [4]. Several authors have reported that the pivot shift test, in contrast to anterior stability tests such as the instrumented anterior knee laxity test and Lachman test, has significant associations with certain subjective symptoms and functions after ACL reconstruction [2, 17]. A residual pivot shift has also been shown to be correlated with the development of osteoarthritis [15]. Therefore, controlling ALRI is one of the most critical keys to improving outcomes after ACL reconstruction.
Consequently, it is important to identify risk factors for residual ALRI after ACL reconstruction as prognostic factors that maximize a successful outcome. Several studies have investigated risk factors for high-grade pivot shift after ACL injury, such as pivoting sports involvement at the time of injury, abnormal lateral posterior tibial slope, anterolateral capsular injuries, and combined meniscal lesions [5, 21, 22, 29]. However, few studies have investigated risk factors for residual pivot shift after ACL reconstruction.
The evaluation of postoperative results after ACL reconstruction may be concomitantly influenced by various factors, and there may be unexpected bias in comparative studies involving relatively small populations. Recently, multicenter collaborative studies have been conducted on ACL reconstruction, such as a Multicenter Orthopaedic Outcomes Network (MOON) study for ACL reconstruction [13, 20] and the Multicenter ACL Revision Study (MARS) for revision ACL reconstruction [11]. A multicenter study is an accepted way of evaluating surgeries more efficiently and may provide a better basis for the subsequent generalization of its findings. However, even in such large cohort studies, risk factors for residual pivot shift after ACL reconstruction have not been thoroughly investigated.
Therefore, the purpose of this study was to investigate risk factors for residual pivot shift after ACL reconstruction based on a multicenter prospective series of ACL reconstructions. The hypothesis underlying this study was that there would be identifiable risk factors for residual pivot shift after ACL reconstruction.
Materials and methods
The Tokyo Medical and Dental University (TMDU) Multicenter Arthroscopic Knee Surgery (MAKS) Study is a prospective longitudinal multicenter cohort study and was designed to examine the prognosis after all knee ligament and meniscus surgeries. The MAKS Study Group began enrolling patients of more than 30 sports medicine surgeons at 12 academic medical centers (2 high-volume centers with more than 100 ACL reconstruction cases a year and 10 low-volume centers) from August 2013. This study was approved by the Institutional Review Board in Tokyo Medical and Dental University (research protocol identification number: 1547), and all participating sites either obtained local institutional review board approval or delegated their approval to the Institutional Review board in Tokyo Medical and Dental University. Surgeons were allowed to determine surgical indications and surgical methods, although they were required to use the same surgical records and evaluation forms. All surgeons finished the training program in Tokyo Medical and Dental University for the knee arthroscopy subspecialty before participating in the study, and all surgeons were trained to evaluate physical examination findings in the same way.
Patients completed an enrollment form that captured demographic factors including age and gender, as well as social history factors including education level, occupation, and sports participation; characteristics of the injury including the sport or activity at the time of injury. Validated patient-reported outcomes including the Lysholm knee scale [6], Knee injury and Osteoarthritis Outcome Score (KOOS) [33] and International Knee Documentation Committee (IKDC) subjective form [12] were also used for preoperative evaluations. Surgeons completed a data form at the time of surgery that documented physical examination findings under anesthesia, intraoperative findings including meniscus and articular cartilage status, and details of treatment including graft choice, fixation methods, meniscus treatment, and articular cartilage treatment. Patients were then prospectively followed up at 3 months, 1 year, 2 years and every year thereafter. Surgeons completed a postoperative form including all physical examination findings related to knee ligaments and menisci. The Lysholm knee scale, KOOS and IKDC subjective form were also documented at every visit.
Data sources and measurement
In the current study, the inclusion criteria involved patients who underwent primary ACL reconstruction using an autologous hamstring tendon graft between August 2013 and August 2016, and who were followed up for 1 year. The exclusion criteria comprised (1) prior injuries or surgeries in the contralateral knee, (2) prior ligamentous injuries in the involved knee, (3) grade 2 or 3 concomitant ligament injuries, and (4) inflammatory or other forms of osteoarthritis. Data from the preoperative period and at 1-year follow-up were used for further analysis, and patients with incomplete data, patients who were lost to follow-up, and patients who had re-injury within 1 year after surgery were also excluded.
In terms of pivot shift test, the grading system used in the current study included the modification of the IKDC criteria [12] (Grade 0 = negative; Grade 1 = subtle glide, but not negative; Grade 2 = glide, Grade 3 = between grade 2 and 4; Grade 4 = clunk; Grade 5 = between grade 4 and 6; Grade 6 = gross), in order to more strictly evaluate the pivot shift phenomenon. These modified criteria have been shown to have high inter-observer reliability with an ICC of 0.97 (95% confidence interval; 0.94–0.98) [18]. Furthermore, these modified criteria have been validated with a quantitative pivot shift measurement using a triaxial accelerometer. It was shown to be very well correlated with tibial acceleration measured by the triaxial accelerometer [23]. The Lachman test was graded according to the IKDC criteria, comparing the ACL reconstruction knee with the normal contralateral knee [Grade 0 = negative; Grade 1 = nearly normal (3–5 mm); Grade 2 = abnormal (6–10 mm); Grade 3 = severely (> 10 mm)]. Anterior instability was also evaluated with the KT-1000 arthrometer (MEDmetric, San Diego, CA, USA) at the manual maximum pull, being expressed as the difference between the injured and uninjured legs in 0.5 mm increments.
The side-to-side difference of more than two grades using the modified IKDC criteria was defined as residual pivot shift at 1 year after surgery, whereas the preoperative Lachman test and pivot shift test were evaluated under anesthesia by absolute value. In addition, according to the Beighton and Honan criteria, patients with an extension angle either in the uninjured or injured knee of more than 10° were defined as hyperextension [3].
Quantitative variables and statistical analysis
This study aimed to determine the preoperative and intraoperative risk factors for residual pivot shift after ACL reconstruction. Thus, logistic regression analysis was conducted with demographic data (age and gender at the time of surgery), physical examinations under anesthesia before surgery (Lachman test, pivot shift test, KT measurement and hyperextension), surgical procedure (single-bundle vs. double-bundle), meniscus injury sites (anterior/middle/posterior segment) and meniscus treatments (none/meniscectomy/repair) as the independent variables, and the postoperative pivot shift test was used as the dependent variable.
Statistical analysis was performed using the IBM SPSS Statistics (Version 24.0, IBM Corp, Armonk, NY, USA). Logistic regression was performed and the resulting odds ratios (ORs) with 95% confidence intervals (CIs) were calculated for all independent predictors of risk factors for the postoperative positive pivot shift. The Mann–Whitney U test was used to compare clinical outcomes between two groups. P < 0.05 was considered significant. Post hoc power analysis for the logistic regression was performed using G-power 3.1 calculation software (Kiel University, Kiel, Germany) as described previously [1, 9], and revealed that, with an alpha of 0.05, a power of 0.88 and 1.00 were achieved for preoperative pivot shift and knee hyperextension, respectively.
Results
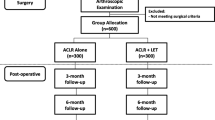
After applying all the exclusion criteria, 368 patients were included in the study (Fig. 1). Detailed results of the positive and negative residual pivot shift (RPS) are shown in Table 1. Forty-eight (13%) patients were classified as having a positive RPS (RPS+), whereas 320 patients were classified as having a negative RPS (RPS−) at 1 year after ACL reconstruction.
According to logistic regression analysis, there were statistically significant differences in knee hyperextension (P = 0.025) and preoperative pivot shift test under anesthesia (P = 0.040). On the other hand, there were no statistically significant differences in age, gender, meniscus injury sites, KT measurement, preoperative Lachman test, meniscus treatment and the surgical procedure between the groups.
In order to investigate the relationship between a residual pivot shift and clinical outcomes, IKDC subjective score, Lysholm score, and KOOS were analyzed between the RPS+ and RPS− groups. However, no between-group differences were noted in these three parameters (Table 2).
Discussion
The most important finding of the current study was that knee hyperextension and preoperative greater pivot shift were risk factors for residual pivot shift 1 year after ACL reconstruction.
The restoration of knee stability is critical to obtaining better outcomes after ACL reconstruction. Knee stability of the reconstructed ACL could be classified into two types: anterior stability and ALRI. Restoring anterolateral rotational stability correlates more with functional outcomes as well as progression of osteoarthritis compared to anterior stability [15, 17]. These results suggest that a residual ALRI patient population may represent a group at an increased risk of poor results after ACL reconstruction, although in the current study, no differences in clinical outcomes were found between RPS+ and RPS− groups at 1 year after surgery probably because of the shortness of the follow-up. Therefore, identifying risk factors for residual ALRI is critical, as it may allow the identification of patients at higher risk of poorer outcomes, and ACL reconstruction should aim to restore anterolateral rotational stability in such high-risk populations.
Several studies have investigated the risk factors for high-grade pivot shift after ACL injury. Song et al. reported that risk factors associated with a grade 3 pivot shift after acute ACL injuries included pivoting sports involvement at the time of injury, abnormal lateral posterior–inferior tibial slope, anterolateral capsular ligament disruptions, and combined lateral meniscal lesions [29]. Brandon et al. reported that a higher pivot shift grade was associated with an increased degree of posterior–inferior tibial slope [5]. Musahl et al. reported that MRI evidence of a concomitant injury to the anterolateral capsule, medial meniscus, or lateral meniscus was associated with increased knee rotatory laxity in patients with an ACL injury [22]. Minami et al. also reported that in ACL-injured patients, the LM posterior root tear was associated with ALRI [21]. However, the association of preoperative ALRI with postoperative residual ALRI has not been thoroughly investigated in past studies. Signorelli et al. reported that preoperative rotational knee laxity measured with a navigation system, was strongly correlated with postoperative rotational laxity at the time of surgery [27]. However, this study only evaluated static rotational laxity, not dynamic ALRI. Katakura et al. reported that preoperative side-to-side acceleration difference of a pivot shift measured by a triaxial accelerometer was correlated with residual ALRI after ACL reconstruction at the time of surgery (in submission), but the evaluation was performed only at the time of surgery. On the other hand, the current study revealed that a preoperative high-grade pivot shift was a significant risk factor for residual pivot shift 1 year after ACL reconstruction.
The role that knee hyperextension plays in the outcome of ACL reconstruction has been evaluated in several studies. Hyperextension causes notch roof impingement in all knees at a certain degree of extension [14]. Kim et al. reported that hyperextension of the knee most strongly predicted postoperative knee instability and function among the clinical indices of joint laxity [16]. Saito et al. showed that anatomic double-bundle ACL reconstruction for extreme knee hyperextension increased superficial graft laceration [26]. Results from the current study also showed that knee hyperextension was a risk factor for residual pivot shift 1 year after ACL reconstruction.
Recently, several kinds of anterolateral structure (ALS) augmentation have been reported to control ALRI, and good clinical outcomes have been reported in terms of the elimination of the pivot shift and lower revision rate [28, 30, 31]. However, its indication varies among surgeons, especially in cases of primary ACL reconstruction [7, 30, 34, 35]. The results of the current study help determine indications for ALS augmentation in cases of primary ACL reconstruction.
There were several limitations to this study. First, the subjective nature of the pivot shift test should be regarded as the primary limitation. Second, a 1-year follow-up period is insufficient. However, the reconstructed ACL is reported to have a greater risk of injury in the first 12 months after surgery [24], suggesting that a residual pivot shift would be detected within 1 year in most cases. Third, whether hyperextension was the cause or consequence of ACL injury was not considered, as we included both the uninjured and injured knees in the definition of hyperextension.
The clinical relevance of this study is that risk factors for residual pivot shift could be identified by preoperative findings of the pivot shift test and knee extension angle, and in cases with higher risk of residual pivot shift, i.e., preoperative high-grade pivot shift and knee hyperextension, additional ALS augmentation might be considered in order to eliminate pivot shift and eventually obtain better outcomes after ACL reconstruction.
Conclusion
The results from a multicenter cohort study indicated that knee hyperextension and a greater preoperative pivot shift under anesthesia were risk factors for residual pivot shift at 1 year after ACL reconstruction.
References
Ahn JH, Lee SH (2016) Risk factors for knee instability after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 24:2936–2942
Ayeni OR, Chahal M, Tran MN, Sprague S (2012) Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 20:767–777
Beighton P, Horan F (1969) Orthopaedic aspects of the Ehlers–Danlos syndrome. J Bone Jt Surg Br 51:444–453
Benjaminse A, Gokeler A, van der Schans CP (2006) Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther 36:267–288
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF (2006) The association between posterior–inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22:894–899
Briggs KK, Kocher MS, Rodkey WG, Steadman JR (2006) Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J Bone Jt Surg Am 88:698–705
Chahla J, Menge TJ, Mitchell JJ, Dean CS, LaPrade RF (2016) Anterolateral ligament reconstruction technique: an anatomic-based approach. Arthrosc Tech 5:e453–e457
Chambat P, Guier C, Sonnery-Cottet B, Fayard JM, Thaunat M (2013) The evolution of ACL reconstruction over the last fifty years. Int Orthop 37:181–186
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160
Georgoulis AD, Papadonikolakis A, Papageorgiou CD, Mitsou A, Stergiou N (2003) Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med 31:75–79
Group M, Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK et al (2010) Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med 38:1979–1986
Hefti F, Muller W, Jakob RP, Staubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1:226–234
Hettrich CM, Dunn WR, Reinke EK, Spindler KP (2013) The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med 41:1534–1540
Jagodzinski M, Leis A, Iselborn KW, Mall G, Nerlich M, Bosch U (2003) Impingement pressure and tension forces of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 11:85–90
Jonsson H, Riklund-Ahlstrom K, Lind J (2004) Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand 75:594–599
Kim SJ, Moon HK, Kim SG, Chun YM, Oh KS (2010) Does severity or specific joint laxity influence clinical outcomes of anterior cruciate ligament reconstruction? Clin Orthop Relat Res 468:1136–1141
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32:629–634
Koga H, Muneta T, Yagishita K, Watanabe T, Mochizuki T, Horie M et al (2014) Effect of femoral tunnel position on graft tension curves and knee stability in anatomic double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 22:2811–2820
Lie DT, Bull AM, Amis AA (2007) Persistence of the mini pivot shift after anatomically placed anterior cruciate ligament reconstruction. Clin Orthop Relat Res 457:203–209
Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP (2016) Factors associated with high-grade Lachman, pivot shift, and anterior drawer at the time of anterior cruciate ligament reconstruction. Arthroscopy 32:1080–1085
Minami T, Muneta T, Sekiya I, Watanabe T, Mochizuki T, Horie M et al (2018) Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc 26:1174–1181
Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y et al (2016) The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med 44:3126–3131
Nakamura K, Koga H, Sekiya I, Watanabe T, Mochizuki T, Horie M et al (2017) Evaluation of pivot shift phenomenon while awake and under anaesthesia by different manoeuvres using triaxial accelerometer. Knee Surg Sports Traumatol Arthrosc 25:2377–2383
Orchard J, Seward H, McGivern J, Hood S (2001) Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med 29:196–200
Ristanis S, Stergiou N, Patras K, Vasiliadis HS, Giakas G, Georgoulis AD (2005) Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy 21:1323–1329
Saito K, Hatayama K, Terauchi M, Hagiwara K, Higuchi H, Takagishi K (2015) Clinical outcomes after anatomic double-bundle anterior cruciate ligament reconstruction: comparison of extreme knee hyperextension and normal to mild knee hyperextension. Arthroscopy 31:1310–1317
Signorelli C, Bonanzinga T, Lopomo N, Marcheggiani Muccioli GM, Bignozzi S, Filardo G et al (2013) Do pre-operative knee laxity values influence post-operative ones after anterior cruciate ligament reconstruction? Scand J Med Sci Sports 23:e219-224
Song GY, Hong L, Zhang H, Zhang J, Li Y, Feng H (2016) Clinical outcomes of combined lateral extra-articular tenodesis and intra-articular anterior cruciate ligament reconstruction in addressing high-grade pivot-shift phenomenon. Arthroscopy 32:898–905
Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Risk factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. Am J Sports Med 44:362–369
Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M et al (2017) Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI study group. Am J Sports Med 45:1547–1557
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 43:1598–1605
Tashman S, Collon D, Anderson K, Kolowich P, Anderst W (2004) Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med 32:975–983
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Vundelinckx B, Herman B, Getgood A, Litchfield R (2017) Surgical indications and technique for anterior cruciate ligament reconstruction combined with lateral extra-articular tenodesis or anterolateral ligament reconstruction. Clin Sports Med 36:135–153
Wagih AM, Elguindy AM (2016) Percutaneous reconstruction of the anterolateral ligament of the knee with a polyester tape. Arthrosc Tech 5:691–697
Acknowledgements
We thank Atsushi Okawa, M.D., Ph.D., for continuous support; Aiko Yamada, Haruno Kroda, Kahaer abula, Yuki Omura and Miyoko Ojima for data registration.
Collaborators
Kawaguchikogyo General Hospital; Akiho Hoshino, M.D., Ph.D., Takashi Ogiuchi M.D., Ph.D., Hideya Yoshimura, M.D., Ph.D., Masaya Hayashi, M.D., Ph.D., Toru Takahashi, M.D., Ph.D., Katsuaki Yanagisawa, M.D., Ph.D., Mio Udo, M.D., Ph.D. Doai Memorial Hospital; Tsuyoshi Nagase, M.D., Ph.D., Tadanori Shimizu, M.D., Ph.D., Ryusuke Saito, M.D., Ph.D. Yokohama Minato Red Cross Hospital; Koji Asano, M.D., Ph.D., Shinpei Kondo, M.D., Ph.D. Tama-hokubu medical center; Jyu Neishin, M.D., Ph.D. Nitobe Memorial Nakano General Hospital; Jun Kitahama, M.D. Suwa Central Hospital; Shinichi Shirasawa, M.D., Ph.D. Nissan Tamagawa Hospital; Tomoyuki Mochizuki, M.D., Ph.D. National Hospital Organization Disaster Medical Center; Masayuki Shimaya, M.D., Ph.D. Mishima General Hospital; Mika Yamaga, M.D., Ph.D. Tsuchiura Kyodo General Hospital; Daisuke Hatsushika, M.D., Ph.D. Soka City Hospital; Arata Yuki, M.D., Ph.D. Tokyo Bay Urayasu Ichikawa Medical Center; Enichi Nakatsuru, M.D. Nerima General Hospital; Shingo Fukagawa, M.D., Ph.D.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
HU analyzed the data and drafted the manuscript. YN and TO conducted the study. TW, MH, KO, HKa, IS and TM collected the data. KK, KH, MK, TH, KI and NA analyzed the data. HKo designed the initial plan, conducted the study and completed the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Study was approved by the Institutional Review Board in Tokyo Medical and Dental University (research protocol identification number: 1547).
Rights and permissions
About this article
Cite this article
Ueki, H., Nakagawa, Y., Ohara, T. et al. Risk factors for residual pivot shift after anterior cruciate ligament reconstruction: data from the MAKS group. Knee Surg Sports Traumatol Arthrosc 26, 3724–3730 (2018). https://doi.org/10.1007/s00167-018-5005-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5005-4