Abstract
Purpose
Valgus deformities of the lower extremity influence patellofemoral joint kinematics. However, studies examining the clinical outcome after treatment of patellar instability and maltracking due to valgus deformity are rare in recent literature. This study’s purpose is to analyze the clinical results after combined distal femoral osteotomy (DFO) for treatment of patellar instability.
Methods
From 2010 to 2016, 406 cases of patellofemoral instability and maltracking were treated. Twenty cases of recurring (≥ 2) patellar dislocations with genu valgum and unsuccessful conservative treatment were included in the study. A radiological analysis was performed, and anteroposterior (AP), lateral and long leg standing radiographs were analyzed, and the leg axis was pre- and postoperatively measured. At least 12 months postoperatively, the clinical leg axis, range of motion (ROM), apprehension sign, Zohlen sign, and J-sign were physically examined. Pain level and knee function were objectified on a visual analogue scale (VAS). The Lysholm, Kujala, and Tegner scores, re-dislocation rate, and patient satisfaction were also examined.
Results
20 combined DFOs on 18 patients with a median age of 23 years (15–55 years) were performed. The preoperative mechanical leg axis was 6.5° ± 2.0° valgus, and the mean tibial tuberosity to trochlear groove (TT-TG) distance was 19.1 ± 4.8 mm. All patients reported multiple dislocations. Intraoperatively, 71% presented III°–IV° cartilage lesions, located retropatellarly in 87% and correlating negatively with the postoperative Lysholm score (r = − 0.462, p = 0.040). The leg axis was corrected by 7.1° ± 2.6°, and in 17 cases, the tibial tubercle was additionally medialized by 10 ± 3.1 mm. All patellae were re-stabilized with medial patellofemoral ligament reconstruction. After a median period of 16 (12–64) months, the pain level decreased from 8.0 ± 1.4 to 2.3 ± 2.1 (VAS p ≤ 0.001) and knee function improved from 40.1 ± 17.9 to 78.5 ± 16.6 (Kujala p ≤ 0.001), 36.1 ± 19.5 to 81.6 ± 11.7 (Lysholm p ≤ 0.001), and 2.0 (1–5) to 4.0 (3–6) (median Tegner p ≤ 0.001). No re-dislocation was observed.
Conclusion
Combined DFO is a suitable treatment for patellar instability and maltracking due to genu valgum, as it leads to very low re-dislocation rates, a significant reduction of pain, and a significant increase of knee function with good-to-excellent results in the short-term follow-up. However, a high prevalence of substantial cartilage lesions is observed, causing postoperative limitations of knee function.
Level of evidence
IV, retrospective cohort study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple contributing factors for patellar instability and maltracking have been identified to date [2, 13, 14]. Osseous deformities, such as trochlear dysplasia or torsional deformities of the lower limb, are now considered more carefully due to their large impact on patellar tracking and stability [5, 8, 9, 20, 21]. In general, good results have been reported after torsional osteotomy or trochleoplasty [8, 9, 20]. Surgical techniques involving tibial tuberosity are commonly performed and have been increasingly examined [1, 14].
Deformities of the leg axis, related to valgus or varus deformities, have been proven to considerably influence patellar tracking [19]. Moreover, it seems reasonable that a valgus position of the femorotibial angle may alter the force vector on the patella in a way that leads to increased lateralization of the patella.
A recently published study on a series of eight patients (ten knees) with valgus malalignment and patella-related symptoms of pain or subluxation has reconfirmed the suggested influence of valgus deformities on the patella [26]. However, studies examining the clinical outcome after combined DFO in the treatment of valgus deformities with patellar instability are rare in the recent literature.
This study’s purpose is to analyze the clinical results after treatment of patellofemoral instability caused by valgus malalignment of the leg axis with combined DFO. Here, the term “combined osteotomy” refers to the combination of multiple surgical procedures in addition to the osteotomy, depending on the pathologies of the knee joint present. This study hypothesizes that good-to-excellent results can be achieved in terms of knee function and reduction of pain as well as low re-dislocation rates if all predisposing risk factors are addressed. To the best of our knowledge, this study has the largest number of cases of all studies published to date.
Materials and methods
All recorded cases of lateral patellar instability or maltracking, which were treated in the study clinic from 2010 to 2016, were reviewed. A retrospective single-center cohort study was conducted to analyze the outcomes of patients who experienced patellar instability due to valgus deformities of the leg axis in the frontal plane and who were treated with a combined medially closing-wedge distal femoral osteotomy (cwDFO).
Inclusion criteria were recurring dislocations of the patella (≥ 2 dislocations) of the affected knee with simultaneous presentation of a relevant valgus deformity of the leg axis, leading to a combination of patellar instability and maltracking. According to the authors’ clinical experience, deformities of ≥ 5° accompanied by patellar maltracking are considered “relevant” and indicative for a DFO. However, in recent literature, no cut-off value has yet been described. Knees with a mechanical axis deformity of < 5°, which presented patellar maltracking, as well as cartilage lesions in the lateral femorotibial compartment, were also subjected to DFO. Higher grade deformities (types 3e and 4 according to Frosch et al. [13]), which would essentially affect patellar tracking, were excluded. Unsuccessful conservative treatment after the first dislocation was reported in all cases. A detailed radiological analysis prior to surgery, including standard anteroposterior (AP) and lateral radiographs and magnetic resonance imaging (MRI) of the knee, was mandatory to measure patella height, tibial tuberosity to trochlear groove (TT-TG) distance and trochlear morphology, and to assess the cartilage status. The leg axis in the frontal plane was determined by measurement of standing long leg radiographs. Torsional MRI or computer tomography (CT) scans of both sides were used to identify torsional deformities if they were suspected. Maltracking was initially evaluated clinically with the J-sign/reversed J-sign test and on transverse MRI scans at the time of first contact with the patient. It was then reconfirmed by direct arthroscopic dynamic visualization at the beginning of every surgery and throughout the procedure. The TT-TG distance was measured from MRI scans of the knee according to Schoettle et al. [24]. A distance of 16 mm with intraoperatively reconfirmed maltracking of the patella was indicative of an additional tibial tuberosity transfer [5, 29]. Patella height was measured on lateral radiographs of the knee, according to Caton-Deschamps [4]. Common scoring systems—visual analogue scale (VAS), Kujala’s anterior knee pain score, Lysholm score, and Tegner activity index—were determined preoperatively and at least 1 year after surgery [17, 27]. An experienced orthopedic resident and a senior orthopedic surgeon performed the clinical examination at the time of follow-up, patellar tracking was re-evaluated as described above, and the re-dislocation rate was evaluated. All complications which needed surgical revision were recorded and analyzed. To analyze patient satisfaction, the patients were asked if they were satisfied with the overall outcome of the surgery and whether they would choose to undergo the same surgical procedure again, if they had to make a decision to do so again. A minimum follow-up of 1 year was conducted.
The treatment algorithm was based on a classification of patellar instability according to Frosch et al. [13]. In addition to genu valgum, all concomitant deformities were considered and appropriately treated in ranking order (Fig. 1). The influence of each procedure on patellar tracking was intraoperatively checked by direct arthroscopic visualization. Medial patellofemoral ligament (MPFL) reconstruction was indicated in the presence of recurring patellar instability, which was observed in all cases of the study cohort.
Treatment algorithm of patellar maltracking and instability. The therapeutic algorithm is based on the classification by Frosch et al. [15]. Type 1 shows a low risk to re-dislocate. Type 2 includes instable patellae without maltracking. Type 3 unites maltracking and instability, due to different predisposing risk factors, including genu valgum, as shown above. Type 4 presents a severe dysplastic trochlea and type 5 does not present instability but maltracking of the patella. Multiple risk factors can occur simultaneously to present a combined deformity, causing patellar maltracking, each of which should be addressed separately, in descending order (blue arrow). All cases of patella instability require stabilization by MPFL reconstruction (green arrow)
Exclusion criteria were first-time traumatic patellar dislocations (with or without flake fracture) and direct trauma to the patella, as well as an unattempted conservative treatment approach. Complex traumas to the knee with ligament injury or traumatic knee dislocations were also excluded, as were patients who did not wish to participate in the study. According to the classification by Frosch et al. [13], higher grades of accompanying trochlea dysplasia (Dejour B-D) or torsional deformities were also excluded from the study.
Surgical technique and postoperative protocol
An arthroscopy was performed at the beginning of every surgery to visualize patellar tracking and evaluate the cartilage status in accordance with the International Cartilage Repair Society (ICRS). Preoperative planning was performed following the rules defined by Paley et al. [22]. A medial subvastus approach was developed to access the medial metaphysis of the femur in all cases. A biplanar osteotomy was performed with an oscillating saw. After osteosynthesis, patellar tracking was re-evaluated.
In the case of persistent maltracking and a pathologically increased TT-TG distance, the tibial tubercle was osteotomized according to Elmslie-Trillat [15], creating a fragment of approximately 5 cm, which was then medialized, under arthroscopic visualization of patellar tracking. The distance of medialization was measured intraoperatively.
The MPFL was reconstructed in all cases, according to a modified version of Schoettle’s technique [25]. A gracilis graft was harvested and fixed in the patella by two suture anchors and by an absorbable interference screw at the anatomical femoral insertion site.
Postoperative AP and lateral radiographs were performed to check for correct implant positioning and gap closure. After initial mobilization during the hospital stay, a standing long leg radiograph in the frontal plane under full-weight bearing was assessed.
The postoperative rehabilitation protocol included partial weight bearing (20 kg body weight) for 6 weeks, and a limited range of motion of 60° for 2 weeks, and 90° of flexion for another 2 weeks. After 6 weeks, full-weight bearing with a free range of motion (ROM) was allowed.
An IRB approval was given by the ethics committee of the Medical Chamber of Hamburg, Germany (ID PV5191).
Statistical analysis
Clinical and radiological results were summarized with mean and standard deviation (SD). The differences in the pre- and postoperative outcome data were applied with paired t tests. Correlations between variables were analyzed. Effects were described with parameter estimates and p values, with a significance level of < 0.05.
Calculations were performed with the statistical analysis software IBM SPSS® Statistics Version 21.0.0.0 (IBM, Armonk, NY, USA) and by a biometrician at Asklepios Proresearch (Hamburg, Germany).
Primary outcome of this study was the change of the Lysholm score values as a result of the intervention. The null hypothesis was that no differences in terms of the Lysholm score would be observed.
Based on the publication of Dickschas et al. [6] and own previous research mean differences of at least 15 and a standard deviation of the differences of at most 20 were expected. With a sample size of 20, the power to detect differences in means will be 90%, using a paired t test with a 5% two-sided significance level.
Results
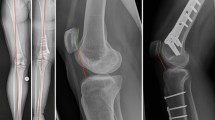
From 2010 to 2016, 406 cases of patellar instability and maltracking were surgically treated, 31 of which were treated due to a valgus deformity of the lower limb. A total of 23 cases (21 patients) were treated with a varizating medial cwDFO. Three patients were lost to follow-up, leaving a total of 18 patients (20 cases) with a median age of 23 years (range of 15–55 years) who were included in the study. Among all included cases, eight knees had undergone surgical treatment, such as MPFL reconstruction, medial retinacular tightening, or lateral retinacular release, before first contact with the study clinic. All of the patients had experienced recurrent dislocations of the patella (Fig. 2).
23-year-old patient with recurrent patellar dislocations and a valgus deformity of the lower limb. The standing X-ray image of the whole leg showed a valgus deformity of 8° on the left side (a). A cwDFO was performed. The preoperatively determined angle of correction was marked by two k-wires (b). A Hohmann retractor was used to protect the dorsal soft tissue (c), and the osteotomy is performed, followed by the osteosynthesis (d). The procedure was complemented by a tibial tubercle transfer and an MPFL reconstruction (e). After 1 year, the patient was pain-free and without re-dislocation
The preoperative measurement of the mechanical leg axis in the frontal plane showed a mean angle of 6.5° ± 2.0° valgus. The mean TT-TG distance was 19.1 ± 4.8 mm, and the average patella height was normal, with a Caton–Deschamps index (CDI) of 1.15 ± 0.1. Table 1 displays the most significant data of the study collective.
Arthroscopically, we found advanced cartilage lesions (III°–IV°, as defined by the ICRS) in 71% of the operated knees (n = 14), 87% (n = 12) of which were located retropatellarly (Figs. 3, 4).
20-year-old patient with recurring patella dislocations. The preoperative X-ray of the leg axis showed a bilateral valgus deformity of 7.5° (a). Previously, a soft-tissue stabilizing surgery failed to stabilize the patella. The axial plane of the MRI revealed IV° retropatellar cartilage lesions and a lateralized patella (b). A mild trochlea dysplasia type A (according to Dejour) was seen. The cartilage lesions were reconfirmed arthroscopically (c). In addition, an increased TT-TG distance of 16.5 mm was measured. A medial cwDFO was performed, correcting the leg axis by 8°, combined with a medialization of the tibial tubercle by 8 mm and a reconstruction of the MPFL. A postoperative standing X-ray image of the whole leg documented a neutralized leg axis after cwDFO, tibial tubercle transfer, and MPFL reconstruction (d)
Among the study population, we performed 20 cwDFOs, correcting the mechanical leg axis by 7.1° ± 2.6°, on average, to normal values (Fig. 5). A tibial tuberosity transfer was performed in 17 cases with an average medialization of 10 ± 3.1 mm to physiological values. In all the cases, an MPFL reconstruction was performed, using autologous gracilis or semitendinosus grafts (Figs. 2, 3).
Intraoperative setting of a varizating, minimal invasive cwDFO. The size of the medial wedge is marked by k-wires in accordance with the preoperative planning of the osteotomy (a). The osteotomy is performed with an oscillating saw with guidance from the k-wires. Care should be taken to avoid soft-tissue damage (b). After the osteotomy is completed, the wedge can be removed using a small clamp (c). d Empty gap after removing the wedge. The gap is then gently closed and the osteosynthesis is performed with a plate
After a median follow-up period of 16 (12–64) months, no re-dislocation was observed. The knee function was improved significantly by the surgery (p < 0.001), and patients experienced a significant postoperative improvement of pain on the VAS (p < 0.001). In addition, the patients’ level of activity significantly increased compared to the level prior to the surgery (p = < 0.001) (Fig. 6; Table 2).
Illustration of pre- and postoperative pain level and knee function. An overall improvement of the patients’ status following the surgery was found. The level of pain on VAS (a) and Kujala score (c) was reduced significantly (p ≤ 0.001). Furthermore, patients’ knee function increased significantly in terms of Lysholm (c) and Tegner (d) (p ≤ 0.001)
We found a negative correlation between the degree of cartilage lesion according to the ICRS definition, and the preoperative (r = − 0.576, p = 0.008), and the postoperative Lysholm scores (r = − 0.462, p = 0.040).
The results led to a patient satisfaction rate of 100%, considering that all of the patients reported that they would choose the same surgical procedure again. Clinically, no persistence of patellar maltracking was observed.
One patient reported irritation caused by the osteosynthesis material, which was treated successfully by plate removal. We observed no further complications, and all osteotomies healed in an appropriate period of time.
Discussion
The most important finding of this study is that excellent clinical results can be achieved by combined DFO in terms of significant pain reduction and significant functional improvement, leading to a high patient satisfaction of 100% after a median follow-up of 16 months, with no reported re-dislocation of the patella.
A high prevalence of advanced retropatellar cartilage lesions was found within the study collective, while a negative correlation with the knee function before (r = − 0.576, p = 0.008) and after surgery (r = − 0.462, p = 0.040) was observed.
Deformities of the lower limbs are known to influence patellofemoral kinematics and to alter the physiological tracking of the patella, thus leading to patellofemoral maltracking and instability [13, 14, 26]. McWalter et al. found the patella to be located more proximally in full extension in the presence of valgus deformities [19]. Functionally, this situation may lead to an increased Q-angle, contributing to a less stable tracking of the patella [7]. However, studies examining the clinical outcome after DFO as a treatment of patellar instability and maltracking are rare in recent literature.
Swarup et al. reported on successful treatment in ten cases of genua valga with subluxated patellae by DFO, including two bifocal (tibial and femoral) osteotomies and one torsional osteotomy [26]. In seven of the ten included knees, the authors found a significant reduction of the preoperative pain level on the VAS from 5.6 to 1.6 and a significant improvement of the Kujala score from 53.3 to 77.4, an observation that is confirmed by our findings. The authors found no re-dislocations at the time of follow-up [26]. However, their collective presented mostly subluxed patellae, without additional medial stabilization, and consisted of a rather heterogenic cohort, which makes a direct comparison rather difficult [26]. We found significant improvement of the Lysholm score from 36.1 ± 19.5 to 81.6 ± 11.7 and the Kujala score from 40.1 ± 17.9 to 78.5 ± 16.6, as well as a significant reduction of pain on the VAS from 8.0 ± 1.4 to 2.3 ± 2.1. In the presented study, all patients had experienced recurring patellar dislocations, which were accompanied by clinically relevant maltracking. A high prevalence of advanced cartilage lesions in 71% of the cases (III°–IV° according to the ICRS) might be responsible for a comparably higher preoperative level of pain and a more restricted knee function.
Dickschas et al. also recently investigated patellofemoral dysbalance due to genua valga in 19 cases which were treated by femoral varization [6]. Twelve knees presented patellar instability, while in seven cases, sole anterior knee pain was reported. In addition to cwDFO, the implemented procedures included two open-wedge DFO and six torsional corrections of the femur, as well as tibial tuberosity transfer in some cases, and they observed no re-dislocation and a significant improvement of Lysholm score from 76 to 92 (p < 0.001) and Kujala score from 72 to 87 (p = 0.009). No MPFL reconstruction was described [6].
In this presented study, the procedures are clearly defined as medial cwDFO, leading to greater homogenization of the implemented procedures. MPFL reconstruction was performed in all cases, due to an omnipresent instability of the patellofemoral joint.
In general, treatment of patellofemoral instability should be based on a 2-column model, consisting of patellar maltracking and patellar instability [11, 12]. As to the presence of patellofemoral instability, not only the maltracking has to be restored; recurrent dislocations essentially require a reconstruction of medially stabilizing structures, such as the MPFL, which is most effectively achieved using autologous semitendinosus or gracilis grafts [3, 18]. Analogous recommendations have been given in cases of torsional deformities, where the patellofemoral joint stability primarily depends on the integrity of the medial patellofemoral ligament [16].
Furthermore, in the presence of patellar instability due to genu valgum, combined deformities with the interaction of various pathologies can be frequently observed, each of which must be considered and specifically addressed if clinically necessary [13]. Therefore, the combination of DFO with additional procedures may be necessary to restabilize and recenter the patella.
The population of this study showed a mean valgus deformity of 6.5° ± 2.0°, with recurrent patellar dislocations in all cases. In addition, we measured pathological TT-TG distanced with an average of 19.1 ± 4.8 mm, which again outlines the extent to which combined procedures are required to effectively address patellar maltracking due to a multifactorial problem. A pathologically increased TT-TG distance with an arthroscopically reconfirmed maltracking may require an additional medialization of the tibial tubercle, which was performed in 17 of the 20 cases presented in the current study.
However, no clear recommendation has yet been given in the literature concerning the angle of the femorotibial deformity, which defines the point of surgical indication for a varus osteotomy, in cases of patellar maltracking and instability due to genu valgum. For patellofemoral instability, we generally indicate a corrective osteotomy if the measured leg axis is ≥ 5° valgus. In the treatment of osteoarthritis of the knee, however, it has been shown that a valgus angle of 3° leads to a 2.5 times higher risk of disease progression and a 5.9 times higher risk of sustaining cartilage lesions [10, 11]. Therefore, a DFO can be taken into consideration earlier if the valgus deformity is found to cause patellofemoral instability and in the simultaneous presence of femorotibial cartilage lesions, especially in the lateral compartment [11].
Preoperatively a poor knee function was observed (Lysholm 36.1) with high levels of pain (VAS 8.0) and a low activity level (median Tegner 2.0). This may partially be explained by the high prevalence of III°–IV° cartilage lesions (71%), which correlate negatively with the preoperative (r = − 0.576, p = 0.008) and the postoperative Lysholm scores (r = − 0.462, p = 0.040). Salonen et al. found progressive deterioration of cartilage after a 5-year follow-up of asymptomatic single-time traumatic patellar dislocations in the absence of further predisposing destabilizing pathologies [23]. The patients enrolled in this study, however, presented severe combined pathologies concerning the leg axis and the TT-TG distance. These deformities are known to alter physiological patellar tracking, causing early deterioration of the patellofemoral cartilage, which may potentially increase the patients’ limitation of knee function [11, 28].
One limitation of this study was its retrospective character. In addition, further bias may have resulted from the wide variance of the follow-up period after which the patients were examined. Moreover, there was no control group, which resulted from the lack of alternative treatment options for the described deformity pattern. Furthermore, the surgical therapy consisted of multiple combined procedures to address all relevant pathologies.
Conclusion
Combined DFO is a suitable treatment for patellar instability and maltracking due to genu valgum, with a very low re-dislocation rate, a significant reduction of pain, and a significant increase of knee function, which showed excellent results in the short-term follow-up. A high incidence of substantial cartilage lesions is observed, which may be responsible for pre- and postoperative limitations of knee function.
References
Balcarek P, Jung K, Frosch KH, Sturmer KM (2011) Value of the tibial tuberosity–trochlear groove distance in patellar instability in the young athlete. Am J Sports Med 39:1756–1761
Balcarek P, Oberthur S, Hopfensitz S, Frosch S, Walde TA, Wachowski MM et al (2014) Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc 22:2308–2314
Bitar AC, Demange MK, D’Elia CO, Camanho GL (2012) Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 40:114–122
Caton JH, Dejour D (2010) Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop 34:305–309
Dejour D, Le Coultre B (2007) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc 15:39–46
Dickschas J, Ferner F, Lutter C, Gelse K, Harrer J, Strecker W (2018) Patellofemoral dysbalance and genua valga: outcome after femoral varisation osteotomies. Arch Orthop Trauma Surg 138:19–25
Dickschas J, Harrer J, Bayer T, Schwitulla J, Strecker W (2016) Correlation of the tibial tuberosity–trochlear groove distance with the Q-angle. Knee Surg Sports Traumatol Arthrosc 24:915–920
Dickschas J, Harrer J, Pfefferkorn R, Strecker W (2012) Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg 132:289–298
Dickschas J, Tassika A, Lutter C, Harrer J, Strecker W (2017) Torsional osteotomies of the tibia in patellofemoral dysbalance. Arch Orthop Trauma Surg 137:179–185
Felson DT, Niu J, Gross KD, Englund M, Sharma L, Cooke TDV et al (2013) Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis Rheum 65:355–362
Frosch K-H, Schmeling A (2015) A new classification system of patellar instability and patellar maltracking. Arch Orthop Trauma Surg 136:1–13
Frosch KH, Akoto R, Schmeling A (2014) Patella dislocation in athletes. Chirurg 85:879–887
Frosch KH, Schmeling A (2016) A new classification system of patellar instability and patellar maltracking. Arch Orthop Trauma Surg 136:485–497
Frosch S, Balcarek P, Walde TA, Schuttrumpf JP, Wachowski MM, Ferleman KG et al (2011) The treatment of patellar dislocation: a systematic review. Z Orthop Unfall 149:630–645
Hall MJ, Mandalia VI (2016) Tibial tubercle osteotomy for patello-femoral joint disorders. Knee Surg Sports Traumatol Arthrosc 24:855–861
Kaiser P, Schmoelz W, Schoettle P, Zwierzina M, Heinrichs C, Attal R (2017) Increased internal femoral torsion can be regarded as a risk factor for patellar instability—a biomechanical study. Clin Biomech 47:103–109
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Ma LF, Wang F, Chen BC, Wang CH, Zhou JW, Wang HY (2013) Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: a randomized controlled trial. Arthroscopy 29:891–897
McWalter EJ, Cibere J, MacIntyre NJ, Nicolaou S, Schulzer M, Wilson DR (2007) Relationship between varus-valgus alignment and patellar kinematics in individuals with knee osteoarthritis. J Bone Jt Surg Am 89:2723–2731
Nelitz M, Dreyhaupt J, Lippacher S (2013) Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med 41:1005–1012
Nelitz M, Dreyhaupt J, Williams SR, Dornacher D (2015) Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. Int Orthop 39:2355–2362
Paley D, Pfeil J (2000) Principles of deformity correction around the knee. Orthopade 29:18–38
Salonen EE, Magga T, Sillanpaa PJ, Kiekara T, Maenpaa H, Mattila VM (2017) Traumatic patellar dislocation and cartilage injury: a follow-up study of long-term cartilage deterioration. Am J Sports Med 45:1376–1382
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity–trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13:26–31
Schottle PB, Romero J, Schmeling A, Weiler A (2008) anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 128:479–484
Swarup I, Elattar O, Rozbruch SR (2017) Patellar instability treated with distal femoral osteotomy. Knee 24(3):608–614
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:42–49
Vivod G, Verdonk P, Drobnic M (2014) Long-term clinical and radiographic outcome of patello-femoral realignment procedures: a minimum of 15-year follow-up. Knee Surg Sports Traumatol Arthrosc 22:2747–2755
Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G (2013) The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc 21:318–324
Acknowledgements
Each author certifies that no financial support was received for this study.
Funding
The study was funded by Asklepios Kliniken Hamburg GmbH (#3209).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was given by the ethics committee of the Medical Chamber of Hamburg, Germany (ID PV5191).
Rights and permissions
About this article
Cite this article
Frings, J., Krause, M., Akoto, R. et al. Combined distal femoral osteotomy (DFO) in genu valgum leads to reliable patellar stabilization and an improvement in knee function. Knee Surg Sports Traumatol Arthrosc 26, 3572–3581 (2018). https://doi.org/10.1007/s00167-018-5000-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5000-9