Abstract
Purpose
The risk of graft failure after anterior cruciate ligament (ACL) reconstructions with hamstring or patellar tendon was evaluated in a French population of athletes.
Methods
Athletes who had undergone ACL autograft reconstruction and who received rehabilitation care at the European Center for Sports Rehabilitation (CERS; Capbreton, France) were screened for this prospective cohort study. Eligibility criteria included a simple hamstring autograft or patellar tendon autograft surgical technique. Patients were contacted by phone to participate in follow-up during the second year after surgery. The primary endpoint was the graft failure frequency, evaluated with a multivariate logistic model with adjustment for baseline patient characteristics. The secondary endpoint was time to graft failure, analyzed by an adjusted Cox model.
Results
A total of 2424 athletes were included after having a hamstring autograft (semitendinosus and gracilis) or a patellar tendon autograft between 2011 and 2014. Of the 988 athletes who responded to a follow-up phone call (40.7% response rate), 33 were excluded for new contralateral ACL rupture (3.3%), with 955 included for analysis (713 hamstring autografts; 242 patellar-tendon autografts). There were no significant differences between the baseline characteristics of the patients analyzed and the population which did not respond to the questionnaire. A significant difference in the frequency of graft failure was seen, 6.5% for hamstring autografts vs 2.1% for patellar-tendon autografts [adjusted odds ratio (OR) = 3.64, 95% CI (1.55; 10.67); p = 0.007]. Mean time to graft failure was 10.7 vs 17.4 months for hamstring and patellar-tendon autografts respectively [adjusted hazard ratio (HR) = 3.50, 95% CI (1.53; 10.11); p = 0.008]. Age less than 25 years significantly increased the frequency of graft failure [adjusted OR = 3.85 (1.89; 8.72); p < 0.001]. The rate of patients returning to competitive sport after the first graft was not significantly different for the two techniques: 70.8% for hamstring and 77.8% for patellar tendon [adjusted OR = 0.718; 95% CI (0.50; 1.02)].
Conclusions
Graft failure is significantly more frequent after hamstring than patellar tendon autografts in a French population, despite similar rates of return to competition. Athletes aged less than 25 years have a higher risk of failure than those aged ≥ 25 years. Our results are in accordance with recent Scandinavian studies.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ligament reconstruction for an anterior cruciate ligament (ACL) injury is one of the most common surgeries in developed countries. In the US, the annual incidence of ACL reconstruction has been reported to be 36.9 per 100,000 persons [10]. Currently two main reconstruction techniques are used: patellar tendon and hamstring autografts. Over the last few years, hamstring autografts have become the principal technique used, such as has been reported in Denmark where the proportion of hamstring autografts increased from 68% in 2005 to 85% in 2011 [26]. However, very few differences have clearly demonstrated between these two reconstruction techniques [1, 3, 6,7,8, 12, 28]. Patellar tendon autografts are more frequently associated with anterior knee pain [3, 6, 7, 18, 28] while hamstring autografts tend to evolve towards greater residual laxity [3, 12, 38]. Thus, the choice of technique is currently based primarily on the surgeon’s experience. Three Scandinavian studies in large populations published in 2014 [11, 22, 26] demonstrated that revision surgeries were more common after hamstring autografts compared to patellar tendon grafts, however two recent meta-analyses [9, 37] did not find hard evidence supporting this, and suggested that further studies are needed.
Published data vary, with notably all studies that demonstrate higher rates of revision surgeries being from the same country. We have hypothesized that graft failure was more frequent after hamstring autografts compared to patellar tendon grafts in a French population. We investigated the influence of the type of surgery on the frequency of graft failure and time to return to competition after an initial ligament reconstruction in a population of athletes, most of whom were performing at a competitive level. We have also evaluated the risk factors for failure across different types of sport.
Materials and methods
Athletes who had undergone an ACL autograft reconstruction and who received rehabilitation care at the European Center for Sports Rehabilitation (CERS; Capbreton, France) were screened for participation in this prospective cohort study. Initially, data from the screened population were entered in a computerized database, including complete surgical, medical, and sports-related data and patients were informed of the study. To be eligible, patients had to have undergone a classic surgical graft involving the patellar or hamstring tendon. Patellar tendon autografts required a transplant of the patellar tendon (bone–patellar tendon–bone), and two tunnels (a femoral and a tibial tunnel), and hamstring autografts required two hamstring muscles (semitendinosus and gracilis), folded over, with a single bundle and two tunnels (a femoral and a tibial tunnel). Patients undergoing any other surgery type were not included: hamstring autografts using only the semitendinosus, hamstring autografts with double bundle and four anatomic tunnels, and autografts with the tensor fasciae latae muscle or other specific surgeries. Patients with a history of ipsilateral and/or contralateral ACL rupture, osteotomy, chondroplasty, an associated complex ligament injury, or a ligament reconstruction combined with anterolateral ligament reconstruction were not included. Sports were analyzed according to discipline and were grouped according to the Arpège classification [5].
For patients playing competitively, the sports level was classified as regional, national, and international participation, while patients playing non-competitively were classified as recreational athletes, such as a sports teacher, coach or monitor.
Rehabilitation was based on post-operative recovery for articular extension at 0° and articular flexion at more than 120°, quadriceps contraction against gravity, and techniques for walking without assistance from 3 to 6 weeks post-surgery. A brace was worn for 3–6 weeks according to the surgeon’s decision. Cardiovascular activity on a bicycle, step machine, or rowing machine was introduced progressively and swimming (crawl) was also introduced during this period. A return to running was introduced around the third or fourth month based on the surgeon’s decision. An isokinetic evaluation of quadriceps and hamstring force was performed during the sixth month after the surgery. Approval to return to the original activity was decided by the surgeon.
After verification of the eligibility criteria, included patients were contacted by telephone during the second year after surgery. In the absence of a response with the first attempt, no further contact was made. Patients who did not answer the call were considered as lost-to follow-up. Data regarding repeat or contralateral ruptures, return to competitive sport, and the time to each of these events were collected. The study was approved by a scientific ethics committee (Goupement de Cooperation Sanitaire Ramsay Générale de Santé pour l’Enseignement et la Recherche, Paris, IRB N. COS-RGDS-2015-09-018).
Statistical analyses
This was an observational, exploratory and exhaustive cohort. The sample size was maximized, according to the center population, to optimize the chance of detecting differences and prognostic factors. Two groups in the included population were defined by the type of autograft performed (patellar tendon vs hamstring). Patient characteristics (sex, age at the time of surgery, type and level of sport practiced) of the two groups were compared. A comparison of patients who answered the phone and those who dropped out patients was performed to confirm the validity of our test population. Multivariate logistic regression analyses were performed to evaluate the impact of the surgical technique on the outcome of the frequency of graft failure (primary endpoint), with adjustment for baseline patient characteristics. A Cox multivariate model accounting for the same factors was performed on the time to graft failure to establish the robustness of the results in terms of the primary endpoint. The rate of return to competition after the first surgery at the time of the response to the questionnaire, a secondary endpoint, was evaluated using a multivariate logistic regression model adjusted for the same variables as for the primary endpoint. The alpha risk was fixed at 5%. Statistical analyses were performed with SAS® for Windows (Version 9.4, SAS Institute Inc., Cary, NC, USA).
Results
A total of 4076 athletes who had an ACL autograft reconstruction between 2011 and 2014 and who received rehabilitation care at the European Center for Sports Rehabilitation were screened (Fig. 1). At total of 46 French LCA specialist surgeons operated the patients. Among the 4076 screened patients, 1652 were not included according to the inclusion criteria (Fig. 1). Ultimately 2424 patients were eligible, 1831 with a hamstring autograft and 593 with a patellar tendon autograft. These 2424 patients were subsequently contacted by phone during the second year after surgery. Of them, 988 (40.7%) answered the first call, all of whom agreed to participate in the study follow-up and respond to the questions. Among them, 33 patients (3.3%) had experienced a contralateral ACL rupture since their initial surgery. Data from these patients were thus excluded from further analyses. There were no significant differences between the baseline characteristics of the patients analyzed (N = 955) and non-analyzed population (N = 1469) in terms of type and level of sport, age, and sex (Table 1). The mean time between the initial surgery and the response to the questionnaire was 19.6 months (± 4.2).
Responses from 955 athletes were thus analyzed, 713 with a hamstring autograft and 242 with a patellar tendon autograft (Table 2). The distribution in terms of sex was similar for the two surgery types. Mean age was 26.2 years in the hamstring autograft group and 26.4 years in the patellar tendon autograft group. The most common sport practiced was rugby (hamstring: 35.1%; patellar tendon: 37.2%), followed by soccer, handball and skiing.
Overall the two surgery groups (hamstring vs patellar tendon autografts) were considered comparable, with no significant differences in terms of sex, age, type and level of sports practiced.
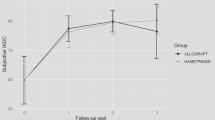
Influence of baseline factors on the outcome of a graft failure
A total of 51 graft failure (5.3% of patients) were reported for the totality of the two groups, 6.5% (N = 46) for the hamstring group and 2.1% (N = 5) for the patellar tendon autograft group (Table 3). The mean time to the graft failure was 10.7 (± 4.0) and 17.4 months (± 4.4), respectively. The multivariate logistic regression showed that the hamstring surgery group was significantly more at risk of graft failure than the patellar tendon autograft, when adjusted for age, sex, type and level of sport, in terms of both the frequency of graft failure [adjusted odds ratio (OR) = 3.637, 95% CI= (1.552 ; 10.662), p = 0.007; Table 4] as well as time to the event [adjusted hazard ratio (HR) = 3.500, 95% CI = (1.529 ; 10.107), p = 0.008; Table 5].
The mean age of athletes with a repeat rupture was 22.9 years for hamstring autografts and 21.0 years for patellar tendon autografts, whereas the mean age of athletes without repeat rupture was 26.5 years for both types of surgery (Table 6). When considering age by category (≤ 25 and > 25 years), the adjusted OR was 3.894 [95% CI 1.887 ; 8.719]; reflecting a significant impact on the likelihood of graft failure in terms of age category, with a worse outcome for individuals aged under 25 years (p < 0.001), when adjusted for other potentially relevant variables (Table 4).
The patient’s level of sport correlated with a non-significant trend for both incidence of graft failure (n.s.) and time to graft failure (n.s.), adjusted for relevant variables (Tables 4, 5). As shown in Table 7, the rate graft failure was higher with increasing level of sport (recreational athletes 2.8%, regional player 4.2%, national player 7.2%, and international player 14.2%).
Sex was not significantly associated with the occurrence of a repeat rupture, when adjusted for other relevant variables (Table 4). According to the Arpège classification for type of sport, the risk of graft failure for all surgical techniques combined decreased with contact, pivoting or not (Table 8), although the type of sport did not have a significant influence on risk of graft failure (n.s.; Tables 4, 9).
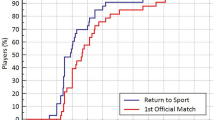
Finally after the initial surgery, 70.8% of competitive athletes returned to competitive sport after a hamstring autograft compared to 77.8% after a patellar tendon autograft (Table 10), which was not significant (n.s.).
Discussion
The most important finding of the study was that the frequency of graft failure after hamstring autografts (6.5%) was significantly higher than for patellar tendon autografts (2.1%), despite a non-significant rate of return to competitive sports. In an earlier study [17], we reported that graft failure after a hamstring autograft was not significantly more frequent than after patellar tendon autografts despite the very different percentages of graft failure, 12.7% for hamstring vs 6.1% for patellar tendon. The main difference between the two series is the sample size, with the current study reporting on 955 athletes compared to 298 subjects in the earlier study. In the published literature, the majority of comparative studies report similar results to our earlier study, showing a trend towards more frequent graft failure following hamstring autografts; however, in almost all cases these differences were not significant [2, 3, 14, 23, 24, 29, 35]. But more recently, several Scandinavian series [11, 22, 26] reported a significant difference as we report here in this study. Again, the principal difference between these older and more recent series resides in the much larger populations reported. In 2014, Rahr-Wagner reported a 5-year risk of graft failure of 4.45% for hamstring autografts vs 3.03% for patellar tendon autografts in 13 647 Danish patients [26], reflecting a 1.90 increased relative risk of graft failure with hamstring autografts. In Norway, Persson et al. also reported a higher risk for graft failure with hamstring autografts after 2-years follow-up compared to after patellar tendon autografts (2.8 vs. 0.7%) in a study of 12,643 patients followed up between 2004 and 2012 [22]. After 5-years, the re-rupture rate was 5.1% for hamstring autografts and 2.1% for patellar tendon autografts. Gifstad et al. [11] grouped databases covering data from 2004 to 2011 for Sweden, Denmark and Norway, allowing combined follow-up of 45,998 ACL ruptures. They demonstrated a lower risk of surgical revisions after patellar tendon autografts with a relative risk of 0.63. After 2 years, the risk of repeat surgery was estimated to be 1% for patellar tendon autografts and 2.3% for hamstring autografts. However, it is important to note that the populations in the studies by Persson et al. [22] and Rahr-Wagner [26] overlap with that of Giftad et al. [11], who grouped the databases of the three Scandinavian countries for almost identical periods of analysis (2004–2011). Overall, it remains pertinent to confirm their results in a series from non-Scandinavian population such as the French population presented here.
Graft failure occurred after a shorter period of time for hamstring autografts compared to patellar tendon autografts (10.7 vs 17.4 months on average, respectively), which was coherent with the literature [19]. It is typical to see a certain fragility associated with the hamstring graft compared to patellar tendon autografts [12, 38] as well as a weakness in terms of the means of fixation, compared to the bone-tendon system of patellar tendon autografts. This translates into a greater hamstring laxity reported in several studies [3, 12, 38], as confirmed by Pinczewski et al. who reported a correlation between laxity and graft failure [24]. However, certain fixation systems appear to be more resistant (endobuttons, screw associated with a staple, etc.) and improve residual laxity [3, 20, 21, 25]. In the future it will be interesting to prospectively analyze large series in terms of the different fixations systems. It may also be important to explore other types of hamstring grafts which appear to be more resistant. Less graft failure is seen with double bundles (p = 0.019) than with single bundles [34], and with hamstring grafts combined with anterolateral ligament reconstruction (p = 0.034) than without [33].
We have demonstrated that age was a risk factor for repeat ACL ruptures. Shelbourne et al. has previously evoked the influence of age on graft failure [31, 32], and Gifstad et al. also reported a decrease in risk with increasing 5-year age categories from 15 years of age up to more than 45 years [11]. Persson et al. found significant differences in terms of risk for 3 age groups (15–19 years, 20–29 years, > 30 years) the risk decreasing with increasing age [22]. Contrary to reports on initial ruptures [4, 13, 16, 27, 30], sex appeared to have no influence on repeat rupture, which has been reported elsewhere in the literature [11, 15, 22, 29, 31, 32, 36].
In terms of methodology, this study has some susceptibility towards biases, notably in terms of selection biases, as is the case for all observational cohort studies. The fact that the patients have different surgeons is a potential source of bias, and it may be worthwhile to include this factor in future analyses. Nonetheless, any associated bias was limited given that patients were included in this study country-wide, along with the fact that there were a high number of participating surgeons, all of whom are specialists in knee reconstruction. Although randomization was not performed at inclusion, the large population, comparable baseline characteristics, and adjusted analyses, reduced potential biases. Finally, the methodology used did not allow for collection of data for the percentage of grafts in lost-to follow-up patients. Nonetheless, it should be noted that the population which did respond to the questions was not significantly different to the population which did not in terms of sex, age, type and level of sport. Furthermore, the statistical analysis was adjusted for factors potentially associated with a given event of interest. As the adjusted comparisons take into account confounding factors, they are thus interpretable.
For this study, a telephone questionnaire was performed an average of 19 months after the autograft. Although this post-operative delay was shorter than other studies, our methodology was very similar to that of Wright et al. and Shelbourne et al. Nonetheless, our 40.7% response rate for the questionnaire was much lower than the 86% reported by Wright et al.or the 78% for Shelbourne et al. [31, 32, 36]. This may be explained by the fact that we contacted patients uniquely by telephone and without multiple follow-up calls to request questionnaire completion. The effect of this potential bias appears to be limited as the population which did respond to the questions was not significantly different to that which did not in terms of sex, age, type and level of sport. The fact the two populations were similar allowed us to obtain a sample providing more pertinent results. Furthermore, our population was reflected a large series of athletes, most of whom practice competitively, with most reports tending to be for sports as leisure activities. The impact of the different sports practiced along with their relationship to graft failure and the level of the sports practiced was identified. This study challenges current thinking that hamstring autografts are equivalent to patellar tendon autografts. Improved fixation systems for hamstring autografts, and more in-depth evaluation of double bundles or grafts combined with anterolateral ligament reconstruction will be valuable in the future. In routine clinical practice, careful rehabilitation practices are essential to decrease the rate of graft rupture with hamstring graft.
Conclusion
The rate of graft failure after a hamstring autograft was statistically higher compared to after a patellar tendon autograft, with graft failure being more frequent in a setting where return to competitive practice was not significantly different. Young athletes aged less than 25 years have a higher risk of repeat ruptures when adjusted for other potential factors, although sex does not impact risk.
References
Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F (2004) Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Jt Surg Am 86–A:2143–2155
Barrett GR, Noojin FK, Hartzog CW, Nash CR (2002) Reconstruction of the anterior cruciate ligament in females. Arthroscopy 18:46–54
Biau DJ (2006) Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ 332:995–1001
Bjordal JM, Arnøy F, Hannestad B, Strand T (1997) Epidemiology of anterior cruciate ligament injuries in soccer. Am J Sports Med 25:341–345
Christel P, Djian P, Darman Z, Witvoët J (1993) Results of Marshall-MacIntosh reconstruction according to 3 scoring systems (ARPEGE, Lysholm, IKDC). 90 cases reviewed with at least a one-year follow-up. Rev Chir Orthop Reparat Appar Mot 79:473–483
Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA (1999) Arthroscopic reconstruction of the anterior cruciate ligament A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med 27:444–454
Feller JA, Webster KE (2003) A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 31:564–573
Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR (2003) Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med 31:2–11
Gabler CM, Jacobs CA, Howard JS, Mattacola CG, Johnson DL (2016) Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: a systematic review, meta-analysis, and meta-regression. Am J Sports Med 44:1069–1079
Gianotti SM, Marshall SW, Hume PA, Bunt L (2009) Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport 12:622–627
Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO (2014) Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary acl reconstructions in Scandinavia. Am J Sports Med 42:2319–2328
Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC (2005) Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthrosc J Arthrosc Relat Surg 21:791–803
Harmon KG, Dick R (1998) The relationship of skill level to anterior cruciate ligament injury. Clin J Sport Med Off J Can Acad Sport Med 8:260–265
Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI (2007) A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and gracilis tendon graft. Am J Sports Med 35:729–739
Laboute E, Legall F, Rochcongar P (2008) Épidémiologie des ruptures du ligament croisé antérieur du genou chez la joueuse de football de haut niveau: à propos de 66 cas. J Traumatol Sport 25:67–74
Laboute E, Savalli L, Lefesvre T, Puig P, Trouve P (2008) Intérêt d’une rééducation spécialisée à distance d’une chirurgie du ligament croisé antérieur chez le sportif de haut niveau. Rev Chir Orthopédique Réparatrice Appar Mot 94:533–540
Laboute E, Savalli L, Puig P, Trouve P, Sabot G, Monnier G, Dubroca B (2010) Analysis of return to competition and repeat rupture for 298 anterior cruciate ligament reconstructions with patellar or hamstring tendon autograft in sportspeople. Ann Phys Rehabil Med 53:598–614
Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J (2007) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med 35:740–748
Maletis GB, Inacio MCS, Desmond JL, Funahashi TT (2013) Reconstruction of the anterior cruciate ligament. Bone Joint J 95:623–628
Milano G, Mulas PD, Ziranu F, Deriu L, Fabbriciani C (2007) Comparison of femoral fixation methods for anterior cruciate ligament reconstruction with patellar tendon graft: a mechanical analysis in porcine knees. Knee Surg Sports Traumatol Arthrosc 15:733–738
Milano G, Mulas PD, Ziranu F, Piras S, Manunta A, Fabbriciani C (2006) Comparison between different femoral fixation devices for ACL reconstruction with doubled hamstring tendon graft: a biomechanical analysis. Arthroscopy 22:660–668
Persson A, Fjeldsgaard K, Gjertsen J-E, Kjellsen AB, Engebretsen L, Hole RM, Fevang JM (2014) increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the norwegian cruciate ligament registry, 2004–2012. Am J Sports Med 42:285–291
Pinczewski LA, Deehan DJ, Salmon LJ, Russell VJ, Clingeleffer A (2002) A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 30:523–536
Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J (2007) A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft. Am J Sports Med 35:564–574
Poolman RW, Farrokhyar F, Bhandari M (2007) Hamstring tendon autograft better than bone patellar-tendon bone autograft in ACL reconstruction: a cumulative meta-analysis and clinically relevant sensitivity analysis applied to a previously published analysis. Acta Orthop 78:350–354
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M (2014) Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the danish registry of knee ligament reconstruction. Am J Sports Med 42:278–284
Rochcongar P, Laboute E, Jan J, Carling C (2009) Ruptures of the anterior cruciate ligament in soccer. Int J Sports Med 30:372–378
Roe J (2005) A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med 33:1337–1345
Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K (2005) Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 21:948–957
Savalli L, Hernandez MI, Laboute E, Trouvé P, Puig PL (2008) Reconstruction du LCA chez le sportif de compétition. Évaluation, à court terme, après reprise du sport. J Traumatol Sport 25:192–198
Shelbourne KD, Gray T (1997) Anterior Cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation a two-to nine-year followup. Am J Sports Med 25:786–795
Shelbourne KD, Gray T, Haro M (2009) Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 37:246–251
Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M (2017) Anterolateral ligament reconstruction is associated with significantly reduced ACL Graft Rupture rates at a minimum follow-up of 2 years: A prospective comparative study of 502 patients from the SANTI Study Group. Am J Sports Med 45:1547–1557
Svantesson E, Sundemo D, Hamrin Senorski E, Alentorn-Geli E, Musahl V, Fu FH, Desai N, Stålman A, Samuelsson K (2017) Double-bundle anterior cruciate ligament reconstruction is superior to single-bundle reconstruction in terms of revision frequency: a study of 22,460 patients from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 25:3884–3891
Wagner M (2005) Hamstring Tendon Versus Patellar Tendon Anterior Cruciate Ligament Reconstruction Using Biodegradable Interference Fit Fixation: A Prospective Matched-Group Analysis. Am J Sports Med 33:1327–1336
Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, Marx RG, McCarty EC, Parker RD, Wolcott M, Wolf BR, Spindler KP (2007) Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a Prospective MOON Cohort Study. Am J Sports Med 35:1131–1134
Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q (2015) A meta-analysis of bone–patellar tendon–bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee 22:100–110
Yunes M, Richmond JC, Engels EA, Pinczewski LA (2001) Patellar versus hamstring tendons in anterior cruciate ligament reconstruction. Arthroscopy 17:248–257
Funding
No outside funding or grants directly related to the research presented in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This cohort study was conducted according to the WMA Declaration of Helsinki.
Informed consent
No written consent is necessary for phone’s questions.
Rights and permissions
About this article
Cite this article
Laboute, E., James-Belin, E., Puig, P.L. et al. Graft failure is more frequent after hamstring than patellar tendon autograft. Knee Surg Sports Traumatol Arthrosc 26, 3537–3546 (2018). https://doi.org/10.1007/s00167-018-4982-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4982-7