Abstract
Purpose
This 3-year prospective study assessed risk factors for noncontact anterior cruciate ligament (ACL) injuries in female Japanese high school basketball players. Players suffering noncontact ACL injuries were assumed to demonstrate poorer hip abductor, knee flexor, and knee extensor muscle strength, as well as static balance, than those without injuries.
Methods
One hundred and ninety-five new female high school basketball players underwent baseline examinations for various parameters during their first year of high school. After the baseline data were collected, all ACL injuries occurring over the subsequent 3 years were recorded. The assessment parameters between the noncontact ACL injury group and the control group were compared.
Results
Of the 195 players, 24 were excluded due to pre-existing injuries present during the initial examination, quitting the basketball club during the follow-up period, or missing data. The remaining 171 players were observed for 3 years; unilateral noncontact ACL injuries were occurred in 12 players. Significantly lower general joint laxity and greater hip abductor strength were observed in the ACL injury group than in the control group. Body mass index (BMI) and hip abductor strength were significantly greater in the ACL injury group than in the control group, based on logistic regression analysis.
Conclusions
Greater BMI and hip abductor muscle strength were independent risk factors for noncontact ACL injuries in female Japanese high school basketball players. Although performing complete screens may be difficult, attention should be given to ACL injuries, particularly in highly competitive players with strong muscles.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Noncontact anterior cruciate ligament (ACL) injuries are prevalent among female high school athletes who play pivot sports that require rapid direction changes. Female athletes’ risk of ACL injuries is higher than that of male athletes [9, 28, 41]. Although surgical treatment for ACL injuries has improved and good clinical outcomes have been reported [25], this sports injury is still serious and its treatment poses some problems (e.g., long recovery time and association with meniscal tears and chondral injuries) [5, 17]. In addition, ACL injuries not only cause loss of time from sports, but also have long-term health consequences, such as a sequentially increased risk for early development of knee osteoarthritis and lower limb dysfunction [1, 26, 29]. Thus, the prevention of ACL injuries is important.
Identifying and understanding the risk factors for ACL injuries are important components of the development of an effective prevention program. Thus, many studies examining the risk factors for and prevention of ACL injuries have been conducted [3, 21, 37]. These studies found that noncontact ACL injuries are likely multifactorial and are related to a combination of neuromuscular, biomechanical, anatomical, hormonal, and psychological factors [12, 18, 32]. In particular, motion patterns related to core balance, muscle strength, and body mass index (BMI), which are modifiable factors, as well as anatomical characteristics, such as general joint laxity (GJL), intercondylar notch, slope of the tibial plateaus, and femoral anteversion, which are not modifiable, play important roles in the aetiology of ACL injuries [6, 11, 24, 33].
Several studies have reported evidence that poor trunk and hip motion patterns and knee valgus are related to an increased incidence of ACL injuries [8, 42, 43]. Furthermore, disorders of these motion patterns may also be influenced by diminished lower limb muscle strength, such as of the hamstring, quadriceps, and hip abductor muscles; thus, muscle strength may be related to the incidence of ACL injuries [13, 27]. Moreover, poor static balance was reported to be associated with noncontact ACL injuries [7]. On one hand, GJL in females (5 of 9 subjects) resulted in a 2.8 times greater risk of ACL injuries in a prospective cohort study [39], and BMI was reported to be associated with decreased intercondylar notches and ACL injuries [6]. Furthermore, greater femoral anteversion and navicular drop predicted greater hip internal rotation and knee external rotation and valgus, which are associated with noncontact ACL injuries [24]. However, most studies on the risk factors for ACL injuries have been performed in Western countries. Nevertheless, there are marked skeletal, muscular strength, and cultural differences between Western and Asian individuals, and the same risk factors are unlikely to similarly apply to individuals from the different cultures. Therefore, there is a need to identify the relevant risk factors and to prepare effective prevention programs for Asian individuals.
To our knowledge, there have not been any cohort studies evaluating the risk factors for noncontact ACL injuries in female Japanese high school basketball players. The purpose of this prospective study was to assess the risk factors for noncontact ACL injuries in this population. The main hypothesis of the study was that female high school basketball players suffering noncontact ACL injuries have worse hip abductor, knee flexor, and knee extensor muscle strength, as well as static balance, compared with uninjured players.
Materials and methods
This 3-year prospective study was designed to assess the risk factors for noncontact ACL injuries in female Japanese high school athletes. Between 2009 and 2011, 195 15-year-old female participants were included in this study. They belonged to high school basketball clubs that were ranked among the top 4 in each prefecture. Athletes who had sustained any lower extremity injuries in the past or had any history of knee surgery were excluded from study participation. Baseline detailed examinations for various parameters were documented during each athlete’s first year of high school.
The players were followed for 3 seasons, from high school entrance to graduation. All participants underwent baseline examinations in April of 2009, 2010, or 2011. After the baseline data had been collected, all ACL injuries occurring over the subsequent 3 years were recorded. None of the teams or participants took part in any special prevention programs during this prospective study. To record all ACL injuries, as well as to understand their playing activities, we contacted the injured players and/or their coaches by directly going to the schools, placing phone calls, and/or e-mailing at least once a month. All ACL injuries were verified at a medical institution by physical examination, magnetic resonance imaging, and arthroscopy.
Baseline examination
A comprehensive test was performed to assess anatomical, neuromuscular, and static balance. All assessment parameters were measured at the Kanazawa University Hospital. The anatomical assessment parameters included height, body weight, BMI, anterior knee laxity, GJL, femoral anteversion, and navicular drop. The muscle strength assessment parameters were knee flexion and extension, hip abduction muscle strength, and the hamstring to quadriceps (H/Q) ratio. Balance assessment parameters were locus length per time and the environmental area that indicates static balance ability.
Both the left and right sides were assessed for each parameter, except for height, body weight, BMI, and balance. Anatomical assessment parameters were measured by experienced orthopedic surgeons. Muscle strength and balance parameters were measured by experienced physical therapists. All anterior knee laxity assessments were performed by one orthopedic surgeon (JN) using a KT-1000 (MED Metric, San Diego, CA, USA) at a pull-out force of 67 N; the differences between the left and right sides were determined. GJL was assessed using the method reported by Beighton et al. [2]. Participants were scored on a numeric (0–9) scale, with 1 point being allocated for the ability to perform each of 5 joint laxity tests. The evaluated joints included the trunk, both little fingers, thumbs, elbows, and knees, for a total of 9 joints. A larger number indicated a higher GJL. Femoral anteversion was assessed using Craig’s test [30]: the patient was placed in the prone position with the knee at 90° flexion. The patient’s hip joint was passively rotated medially and laterally, while palpating the greater trochanter prominence until the outward most point was identified on the lateral aspect of the hip. Furthermore, the angle of the hip was measured, using a goniometer, to determine the amount of anteversion, using the long axis of the tibia. It was measured by 2 orthopedic surgeons: 1 rotated the subject’s hip and the other performed the goniometer measurements. To evaluate the navicular drop, the most protuberant part of the navicular bone was marked, and the difference between the sitting and standing positions was measured [31]. The maximal knee flexion and extension muscle strength were tested using a MYORET (Kawasaki Heavy Industries, Tokyo, Japan), with an angular velocity of 60°/s. Participants warmed up for 10 min on a bicycle ergometer before undergoing the measurements. Subsequently, each participant sat in a chair with 90° hip flexion, while the trunk, pelvis, and lower unmeasured leg were immobilized with a belt. The movement center of the lever arm was matched, as accurately as possible, to the lateral joint line of the knee, and an arm’s-length reach was kept between the center of motion and the middle of the lower leg. Resistance pads were fixed to the proximal and distal tibiae, such that they were equidistant from the arm tip. The range of motion of the knee was set as the maximum extension angle from the maximum flexion angle in a chair-seated position, and extension/flexion movement of the knee was performed thrice, within the set range, after an initial practice round. During the measurement, each participant placed her hands across her chest to avoid providing support from the arms or torso. Assessment values from each measurement round were averaged to generate a final maximum muscle strength value. To standardise maximal muscle strength, the measured values were normalized to the subject’s body weight.
The maximal isometric hip abductor strength was measured using a handheld dynamometer (µTAS F-1®: ANIMA, Tokyo, Japan). Each participant was placed in a supine position on the examination table, the leg was extended, and the hip was maintained in the neutral position in the coronal and sagittal planes. In addition, the contralateral thigh was fixed to the table with a strap, which served as the measurement start position. While assessing the hip abductor, each participant placed her hands across her chest to avoid providing support from the arms or torso. The dynamometer was placed 2 cm proximal to the lateral malleolus and resistance was applied in a fixed position for at least 2 s, until maximal contraction had been measured. Another examiner held the shoulder and pelvis, contralateral to the measurement limb. The measurement was performed twice on each side after an initial practice round, with the peak force taken as the final value. A 2-min break was provided between each measurement. Finally, peak force measurements were normalized to the subject’s body weight and lower limb length.
Static balance was measured with a Gravicorder (ANIMA, Tokyo, Japan). Postural sway was measured for 30 s, using a 20-Hz sampling frequency, during two-leg standing, with the subject’s eyes open. During the measurement, participants stood barefoot, with their feet placed on the centre of measurement at a reference point on the examination platform. With their eyes open, participants fixed their gaze on a visual point placed 1 m in front of them, at eye level, such that no moving objects could enter their visual field. The locus length per time, which indicated attitude control ability, and the environmental area that indicated equilibrium ability were measured. The measurements were carried out twice with a 1-min rest between measurements. Because the second measurement has been reported to be more accurate than the first measurement, using this procedure [4, 16], data from the second measurement were used for analysis, in this study.
This study was approved by the Ethical Committee of the Graduate School of Medical Sciences, Kanazawa University (approval # 1050). Participants and their parents and coaches were given a thorough explanation of the study design and voluntarily provided written informed consent.
Statistical analyses
The data were analysed using the Statistical Package for the Social Sciences for Windows, (version 23.0; IBM, Armonk, NY, USA). The muscle assessment parameters were measured on the affected side in the ACL injury group, and randomly on the left side or right side in the control group. The assessment parameters between the ACL injury group and the control group were first compared using Student’s t test, and the muscle strength parameters were measured from the injured side in the ACL injury group and randomly from the left side or right side in the control group; parameters with P values less than 0.2 were considered independent variables using logistic regression analysis (simultaneous). The level of significance for all statistical analyses was set at α = 0.05 (values of P < 0.05 were considered statistically significant). A prior power analysis for sample size was performed; for an effect size of 0.76, power of 0.8, and an α level of 0.05; a total of 154 individuals were required.
Results
ACL injury incidence
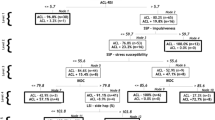
Of the 195 players, 24 were excluded, because 5 had pre-existing injuries present at the initial examination (2 ankle sprains, 2 low back pain, and 1 muscle injury), 15 quit the basketball club during the follow-up period, and 4 had missing data. Two contact ACL injuries and 1 player with bilateral injuries were also excluded from the study. Hence, this prospective cohort study included 168 players, with 12 injuries (12 players) in the noncontact ACL injury group and 156 players in the control (no ACL injuries) group (Fig. 1). The participants’ mean age (months) at baseline is shown in Table 1. The mean age (months) at the time of injury was 194.5 ± 6.0, and the average time between the baseline measurement and injury was 14.5 ± 6.0 months. All noncontact ACL injuries occurred in regular players who were typically in the starting line-up during competitions. The cohort’s annual incident ratio for noncontact ACL injuries was 2.4%.
Assessment parameters
Upon anatomical assessment, only GJL was significantly lower in the ACL injury group than in the control group, according to Student’s t test (Table 1; P = 0.04). In terms of muscle strength and balance assessment, only the hip abductor strength was significantly greater in the ACL injury group than in the control group, according to Student’s t test (Table 2; P = 0.04). In the assessments, the P values for BMI, GJL, knee flexor and extensor strength, hip abductor strength, and locus length per time were less than 0.2; thus, these were considered independent variables in the logistic regression analysis.
The odds ratio, representing the possibility of noncontact ACL injury, 95% confidence interval (CI), and the P value for the 6 assessment parameters were calculated using logistic regression analysis. The results showed that BMI and hip abductor strength were significantly greater in the ACL injury group than in the control group (Table 3; BMI: P = 0.009, 95% CI 1.101–1.952; hip abductor strength: P = 0.03, 95% CI 1.35–320.35).
Discussion
The main findings of this 3-year prospective cohort study of female Japanese high school basketball players were that, contrary to our hypothesis, greater BMI and hip abductor strength were independent risk factors for noncontact ACL injuries.
Of the anatomical parameters assessed in our study, greater BMI was detected as an independent risk factor for noncontact ACL injuries in the logistic regression analysis, similar to the findings of the previous reports [6, 40]. In a case–control study assessing the risk factors for ACL injury, Vacek et al. [40] reported that a higher BMI and increased anterior–posterior knee laxity were predictive of ACL injuries in female athletes. A greater BMI may be related to increased knee joint compression forces, which may lead to ACL injuries during sporting activities [10, 20].
In terms of knee flexor and extensor muscle strength, it has been reported that the relative level of specific muscle activation patterns of the hamstring and quadriceps muscles is important for sagittal and coronal plane joint stability [19]. Although hamstring muscle weakness and a lower H/Q ratio may be considered to lead to ACL injuries [22], a low H/Q ratio is not directly related to ACL injuries [35, 39]; thus, there is no consensus on the matter. In our study, knee flexor and extensor muscle strengths were not significantly different between the 2 groups. Furthermore, contrary to past reports, knee flexor and extensor muscle strength tended to be greater in the ACL injury group.
As for the hip abductor, reduced hip abductor and external rotation strengths were shown to be independent risk factors for ACL injuries in a previous prospective study [15], in contrast to the present findings. The mechanism underlying ACL injuries due to weak hip abductors may be that weakness in the hip abductor predisposes the individual to greater hip adduction and internal rotation, causing increased knee valgus motion and knee abduction movements [8, 38]. On the other hand, a large cohort study that included a large number (n = 867) of elite handball and football players was recently reported by Steffen et al. [35]. No statistically significant association between hip abduction strength and increased ACL injury risk was found in their study. As a potential mechanism, greater hip abductor muscle strength was considered to lead to ACL injury, as stated in the literature. During sporting activities, athletes who have greater hip abductor strength may counterbalance this greater muscle strength and be predisposed to hip adduction; furthermore, knee valgus motion may occur. The relationship of lower limb muscle strength with noncontact ACL injuries and their prevention is difficult to conclude from the findings of the present and previous studies.
Based on the results of our own and previous studies on the relationship between lower limb muscle strength and ACL injuries, strengthening lower limb muscles may not be essential for preventing ACL injuries [35, 39]. Moreover, attention should also be given to other body parts, e.g., the inferior foot muscles. The whole body motion pattern and the dynamic valgus of the knee are influenced by the lower limb muscles, as Hewett et al. [11] stated. In our prevention training study, using positron emission tomography [23], inferior foot muscle motion was increased. Strengthening this muscle is considered to improve dynamic valgus motion and prevent noncontact ACL injuries.
Regarding the association between noncontact ACL injuries and static balance, although static balance was not significantly different between the 2 groups in our study, the locus length per time tended to be worse in the ACL injury group. Steffen et al. [36] reported results similar to ours, using postural control. The reproducibility of the selected variables was reportedly poor and, therefore, could not detect an association between postural control and ACL injuries. Previously, poor balancing ability has been reported to be a risk factor for ACL injuries, and balance training is considered to be necessary for young athletes [14].
In female athletes, greater GJL has been reported to be a risk factor for noncontact ACL injury [40]. In our study, GJL was significantly lower in the noncontact ACL injury group than in the control group. However, it was not an independent risk factor according to the logistic regression analysis. GJL was somewhat related to noncontact ACL injuries, but it was not a significant independent factor, and was also affected by other factors.
The competitive ability of each athlete, and whether or not they were regular players, was considered to have significantly influenced our findings relative to BMI and hip abductor strength being significant independent risk factors for noncontact ACL injuries. In addition, since the number of games played is greater for regular players than for those who play less regularly, the playing time, including games and practices, was also longer. Thus, the chance of encountering situations that may result in ACL injuries, such as cutting and landing motions, may be increased. In support of this speculation, the previous studies have reported that competitive athletes with longer playing times were exposed to more situations that tend to cause ACL injuries [34].
In our study as well as in the previous reports, ACL injuries were shown to be caused by many factors. Thus, it has been considered that ACL injuries cannot be prevented by muscular strength and balance training, alone. Hence, to produce effective ACL prevention programs, it will be necessary to conduct comprehensive studies evaluating multiple factors among highly competitive athletes.
One of the strengths of our study is its prospective design. In addition, the risk factors for noncontact ACL injuries have not been previously investigated in a Japanese cohort. The high incidence of ACL injuries, large sample size, high follow-up rate, and direct arthroscopic confirmation of complete ACL tears were other advantages of this study.
There are some limitations to this study. First, the baseline examinations were only performed at the time of high school admission. Assessments of changes in anatomical parameters, as well as changes in lower limb muscle strength and balance, were not performed during the 3-year period after admission. The parameters were also not assessed when noncontact ACL injuries occurred, and the assessment test was only performed once per participant; therefore, the reliability of the test could not be evaluated. In addition, the playing time, including practice vs. game times, was not recorded; therefore, exposure data were not included in our risk factor analysis. Finally, although the anatomical parameters of lower limb muscle strength and static balance were assessed, the influence of many other factors related to ACL injuries, such as knee kinematics, hormonal balance, and psychology, were not included.
Although greater BMI and hip abductor strength are independent risk factors for noncontact ACL injuries in our results, a completely targeted screening was difficult to perform, because noncontact ACL injuries are influenced by various factors. Therefore, prevention of these injuries, for all athletes, is considered to be important at the moment. Nevertheless, this study suggests that highly competitive athletes with strong muscles and high BMIs require increased attention due to the possibility of developing noncontact ACL injuries. Future studies that focus on highly competitive athletes and involve the evaluations of multiple factors, at least annually, are required.
Conclusions
Greater BMI and hip abduction muscle strength were detected as independent risk factors for noncontact ACL injuries in female Japanese high school basketball players. Although complete screens may be difficult, attention should be given to ACL injuries, particularly in highly competitive players with strong muscles.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- GJL:
-
General joint laxity
- H/Q:
-
Hamstring/quadriceps
References
Ajuied A, Wong F, Smith C, Norris M, Earnshaw P, Back D, Davies A (2014) Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med 42:2242–2252
Beighton P, Solomon L, Soskolne CL (1973) Articular mobility in an African population. Ann Rheum Dis 32:413–418
Bisciotti GN, Chamari K, Cena E, Carimati G, Volpi P (2016) ACL injury in football: a literature overview of the prevention program. Muscles Ligaments Tendons J 6:473–479
Demura S, Yamaji S, Noda M, Kitabayashi T, Nagasawa Y (2001) Examination of parameters evaluating the center of foot pressure in static standing posture from viewpoints of trial-to-trial reliability and interrelation4ships among parameters. Equilib Res 60:44–55
Dunn KL, Lam KC, Valovich McLeod TC (2016) Early operative versus delayed or nonoperative treatment of anterior cruciate ligament injuries in pediatric patients. J Athl Train 51:425–427
Evans KN, Kilcoyne KG, Dickens JF, Rue JP, Giuliani J, Gwinn D, Wilckens JH (2012) Predisposing risk factors for non-contact ACL injuries in military subjects. Knee Surg Sports Traumatol Arthrosc 20:1554–1559
Fernandes TL, Felix EC, Bessa F, Luna NM, Sugimoto D, Greve JM, Hernandez AJ (2016) Evaluation of static and dynamic balance in athletes with anterior cruciate ligament injury—a controlled study. Clinics (Sao Paulo) 71:425–429
Frank B, Bell DR, Norcross MF, Blackburn JT, Goerger BM, Padua DA (2013) Trunk and hip biomechanics influence anterior cruciate loading mechanisms in physically active participants. Am J Sports Med 41:2676–2683
Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ (2016) Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med 44:2716–2723
Hashemi J, Breighner R, Chandrashekar N, Hardy DM, Chaudhari AM, Shultz SJ, Slauterbeck JR, Beynnon BD (2011) Hip extension, knee flexion paradox: a new mechanism for non-contact ACL injury. J Biomech 44:577–585
Hewett TE, Ford KR, Hoogenboom BJ, Myer GD (2010) Understanding and preventing acl injuries: current biomechanical and epidemiologic considerations—update 2010. N Am J Sports Phys Ther 5:234–251
Hewett TE, Myer GD, Ford KR (2006) Anterior cruciate ligament injuries in female athletes part 1, mechanisms and risk factors. Am J Sports Med 34:299–311
Hewett TE, Myer GD, Ford KR, Heidt RS Jr, Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P (2005) Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 33:492–501
Hutchinson AB, Yao P, Hutchinson MR (2016) Single-leg balance and core motor control in children: when does the risk for ACL injury occurs? BMJ Open Sport Exerc Med 2:e000135
Khayambashi K, Ghoddosi N, Straub RK, Powers CM (2016) Hip muscle strength predicts noncontact anterior cruciate ligament injury in male and female athletes: a prospective study. Am J Sports Med 44:355–361
Kitabayashi T, Demura S, Noda M (2003) Examination of the factor structure of center of foot pressure movement and cross-validity. J Physiol Anthropol Appl Human Sci 22:265–272
Kluczynski MA, Marzo JM, Bisson LJ (2013) Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: a prospective study. Am J Sports Med 41:2759–2765
Kosaka M, Nakase J, Numata H, Oshima T, Takata Y, Moriyama S, Oda T, Shima Y, Kitaoka K, Tsuchiya H (2016) Psychological traits regarding competitiveness are related to the incidence of anterior cruciate ligament injury in high school female athletes. Knee 23:681–685
Lloyd DG, Buchanan TS, Besier TF (2005) Neuromuscular biomechanical modeling to understand knee ligament loading. Med Sci Sports Exerc 37:1939–1947
Markolf KL, Jackson SR, Foster B, McAllister DR (2014) ACL forces and knee kinematics produced by axial tibial compression during a passive flexion-extension cycle. J Orthop Res 32:89–95
Martinez JC, Mazerolle SM, Denegar CR, Joseph MF, Pagnotta KD, Trojian TH, DiStefano LJ (2017) Female adolescent athletes’ attitudes and perspectives on injury prevention programs. J Sci Med Sports 20:146–151
Myer GD, Ford KR, Barber Foss KD, Liu C, Nick TG, Hewett TE (2009) The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med 19:3–8
Nakase J, Inaki A, Mochizuki T, Toratani T, Kosaka M, Ohashi Y, Taki J, Yahata T, Kinuya S, Tsuchiya H (2013) Whole body muscle activity during the FIFA 11 + program evaluated by positron emission tomography. PLoS One 8:e73898
Nguyen AD, Shultz SJ, Schmitz RJ, Luecht RM, Perrin DH (2011) A preliminary multifactorial approach describing the relationships among lower extremity alignment, hip muscle activation, and lower extremity joint excursion. J Athl Train 46:246–256
Nwachukwu BU, Anthony SG, Lin KM, Wang T, Altchek DW, Allen AA (2017) Return to play and performance after anterior cruciate ligament reconstruction in the National Basketball Association: surgeon case series and literature review. Phys Sportsmed 45:303–308
Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38:2201–2210
Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE (2010) Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 38:1968–1978
Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K (2007) A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy 23:1320–1325
Risberg MA, Oiestad BE, Gunderson R, Aune AK, Engebretsen L, Culvenor A, Holm I (2016) Changes in knee osteoarthritis, symptoms, and function after anterior cruciate ligament reconstruction: a 20-year prospective follow-up study. Am J Sports Med 44:1215–1224
Ruwe PA, Gage JR, Ozonoff MB, DeLuca PA (1992) Clinical determination of femoral anteversion. A comparison with established techniques. J Bone Jt Surg Am 74:820–830
Shultz SJ, Carcia CR, Gansneder BM, Perrin DH (2006) The independent and interactive effects of navicular drop and quadriceps angle on neuromuscular responses to a weight-bearing perturbation. J Athl Train 41:251–259
Shultz SJ, Schmitz RJ, Nguyen AD, Chaudhari AM, Padua DA, McLean SG, Sigward SM (2010) ACL research retreat V: an update on ACL injury risk and prevention, March 25–27, 2010, Greensboro, NC. J Athl Train 45:499–508
Smith HC, Vacek P, Johnson RJ, Slauterbeck JR, Hashemi J, Shultz S, Beynnon BD (2012) Risk factors for anterior cruciate ligament injury: a review of the literature—part 1: neuromuscular and anatomic risk. Sports Health 4:69–78
Soligard T, Grindem H, Bahr R, Andersen TE (2010) Are skilled players at greater risk of injury in female youth football? Br J Sports Med 44:1118–1123
Steffen K, Nilstad A, Kristianslund EK, Myklebust G, Bahr R, Krosshaug T (2016) Association between lower extremity muscle strength and noncontact ACL injuries. Med Sci Sports Exerc 48:2082–2089
Steffen K, Nilstad A, Krosshaug T, Pasanen K, Killingmo A, Bahr R (2017) No association between static and dynamic postural control and ACL injury risk among female elite handball and football players: a prospective study of 838 players. Br J Sports Med 51:253–259
Taylor JB, Waxman JP, Richter SJ, Shultz SJ (2015) Evaluation of the effectiveness of anterior cruciate ligament injury prevention programme training components: a systematic review and meta-analysis. Br J Sports Med 49:79–87
Thorborg K, Bandholm T, Hölmich P (2013) Hip- and knee-strength assessments using a hand-held dynamometer with external belt-fixation are inter-tester reliable. Knee Surg Sports Traumatol Arthrosc 21:550–555
Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC (2003) Risk factors associated with noncontact injury of the anterior cruciate ligament. a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med 31:831–842
Vacek PM, Slauterbeck JR, Tourville TW, Sturnick DR, Holterman LA, Smith HC, Shultz SJ, Johnson RJ, Tourville KJ, Beynnon BD (2016) Multivariate analysis of the risk factors for first-time noncontact ACL injury in high school and college athletes: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med 44:1492–1501
Waldén M, Hägglund M, Werner J, Ekstrand J (2011) The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee Surg Sports Traumatol Arthrosc 19:3–10
Willson JD, Ireland ML, Davis I (2006) Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc 38:945–952
Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J (2007) Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med 35:1123–1130
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Ethical approval
This study was approved by the Ethical Committee of the Graduate School of Medical Sciences, Kanazawa University (approval # 1050).
Informed consent
All participants and their parents coaches were given a thorough explanation of the study design and voluntarily provided written informed consent.
Rights and permissions
About this article
Cite this article
Shimozaki, K., Nakase, J., Takata, Y. et al. Greater body mass index and hip abduction muscle strength predict noncontact anterior cruciate ligament injury in female Japanese high school basketball players. Knee Surg Sports Traumatol Arthrosc 26, 3004–3011 (2018). https://doi.org/10.1007/s00167-018-4888-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4888-4