Abstract
Purpose
To determine how the incision technique for hamstring tendon (HT) harvest in anterior cruciate ligament (ACL) reconstruction affects the risk of injury to the IPBSN and clinical outcome.
Methods
A systematic literature search of the MEDLINE/Pubmed, Cochrane Central Register of Controlled Trials (CENTRAL) and EBSCOhost electronic databases and clinicaltrials.gov for unpublished studies was performed to identify comparative studies investigating injury to the IPBSN after HT ACL reconstruction by comparing at least two different incision techniques. Data were extracted for the number of patients with evidence of any neurologic deficit corresponding to injury to the IPBSN, area of sensory deficit, the Lysholm score and patient satisfaction. The mean difference (MD) in study outcome between incision groups was assessed. The relative risk (RR) and the number needed to treat (NNT) were calculated. The Chi-square and Higgins’ I2 tests were applied to test heterogeneity. Data were pooled using a Mantel–Haenszel random-effects model if the statistical heterogeneity was > 50% and a fixed-effects model if the statistical heterogeneity was < 50%. The risk of bias was evaluated according to the Cochrane Database questionnaire and the quality of evidence was graded according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines.
Results
A total of eight studies (three randomized controlled trials (RCTs) and five comparative studies) were included, of which six compared vertical and oblique incisions, one horizontal and vertical incisions, and one compared all three techniques. HT harvest was performed through a vertical incision in 329 patients, through an oblique incision in 195 patients and through a horizontal incision in 151 patients. Considering the meta-analysis of the RCTs, the performance of a vertical incision significantly increased the risk of causing IPBSN deficiency compared with both oblique and horizontal incision [RR 1.65 (CI 1.10–2.49, p = 0.02) and RR 2.45 (CI 1.73–3.47, p < 0.0001), respectively]. A significantly larger area of sensory deficit was found with vertical incisions compared with oblique ones, with an MD of 22.91 cm2 (95% CI 7.73–38.08; p = 0.04). No significant differences were found between the incision techniques in relation to patient-reported outcomes. The same trend was obtained after the performing a meta-analysis of all eight included studies. The quality of evidence in this meta-analysis was determined as “low” to “moderate”, mostly due to inadequate methods of randomization and high heterogeneity among the included studies.
Conclusion
The performance of a vertical incision to harvest HTs for ACL reconstruction significantly increased the risk of iatrogenic injury to the IPBSN compared with both oblique and horizontal incisions.
Level of evidence
Level I–III, meta-analysis of comparative studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) ruptures are among the most common injuries in the young, active population [4, 23]. The surgical reconstruction of the ACL is regarded as the gold standard treatment and it has been shown successfully to return the majority of patients to the desired level of physical activity [14, 15]. The most commonly used graft options for ACL reconstruction are bone-patellar-tendon-bone and hamstring tendons (HTs). Comparable outcomes have been reported between the graft types, but the HT autograft is advocated by some surgeons, since it has been associated with lower rates of donor-site morbidity and postoperative complications [20, 26]. Nevertheless, the HT harvest also involves potential risks, such as damage to the terminal branches of the saphenous nerve [27]. This iatrogenic injury may lead to anterior knee pain or discomfort due to hypo- or dysanesthesia, allodynia or painful neuroma [3]. Immediately after passing the adductor canal, the saphenous nerve divides into two terminal branches—the sartorial branch and the infrapatellar branch. The infrapatellar branch of the saphenous nerve (IPBSN) runs vertically on the medial aspect of the knee along the posterior rim of the sartorius muscle and pierces the fascia lata between the sartorius and gracilis tendons to provide sensory perception of the skin anterior and medial to the knee [1, 8, 27, 31]. However, the anatomy of the IPBSN can vary considerably, with numerous ramifications [11] and a location-dependent position [12].
There is a shortage of studies investigating the potential damage to these neural branches while harvesting HT grafts in ACL reconstruction and the risk may be underestimated. In fact, lesions of the IPBSN have been reported to occur in 12–84% of the patients undergoing ACL reconstruction with an HT graft [3, 9, 13, 27, 29]. The course of the branch at the pes anserinus puts it at substantial risk of damage when an incision is made to harvest HTs [12]. The direction in which the incision is made has, therefore, been the subject of investigation in relation to how the direction might affect the risk of iatrogenic IPBSN injury [10, 13, 16, 17, 22, 25, 28, 30]. However, no consensus has been reached in the attempts to determine the most appropriate incision, which might be relevant in order to reduce the risks of iatrogenic nerve injury and further optimize the outcomes offered by ACL reconstruction procedure.
The purpose of this meta-analysis was to identify how the incision technique applied to HT harvest in ACL reconstruction affects the risk of iatrogenic nerve injury and to compare the outcome between different types of incision technique.
Materials and methods
Search strategy
A meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines [19]. A systematic search of the MEDLINE/Pubmed, Cochrane Central Register of Controlled Trials (CENTRAL) and EBSCOhost electronic databases and clinicaltrials.gov for unpublished studies was performed in February 2017.
The search string was built as follows: “ACL” OR “Anterior Cruciate Ligament” combined through the Boolean operator AND with “saphenous” OR “infrapatellar”. The electronic database search was supplemented by a manual search of the reference lists of included articles and the ePublication lists of the following leading orthopedic and sports medicine journals: American Journal of Sports Medicine, British Journal of Sports Medicine, Knee Surgery Sports Traumatology Arthroscopy, Arthroscopy Journal, Journal of Bone and Joint Surgery American and British versions, International Orthopaedics and The Knee.
Article selection
The eligibility of searched articles was assessed on the basis of prespecified inclusion criteria. Articles published in peer-reviewed journals in all languages were considered. Only randomized controlled trials (RCTs), quasi-RCTs and comparative studies (prospective or retrospective) investigating ACL reconstruction performed with HT autografts were included. Studies comparing at least two of vertical, oblique or horizontal incision techniques were eligible, if additional reporting of the postoperative sensory function of the IPBSN existed. All the criteria had to be fulfilled for the article to be included. Biomechanical, in-vitro studies, review articles, surgical techniques, case reports, letters to the editor, editorials and conference abstracts were excluded. Two authors independently reviewed the title and abstract of each article from the systematic literature search. The full text of the article was obtained and evaluated if eligibility could not be assessed from the first screening. Any disagreements were resolved via a consensus discussion between the two reviewers and the senior author was consulted if the disagreement could not be resolved.
Outcome measurements
The outcome measurements were defined as follows: evidence of any neurologic deficit corresponding to injury to the IPBSN, area of sensory deficit over the skin area innervated by the IPBSN, the Lysholm score and patient satisfaction based on continuous scales.
Data extraction and synthesis
An electronic piloted form for data extraction was created prior to the study. Patient demographic details including gender, age at surgery and concomitant meniscal injuries were extracted. Details of study design such as level of evidence, exclusion criteria, type of randomization, technique for ACL reconstruction, length of the incision, number of operating surgeons, rehabilitation protocol and methods for evaluating and defining IPBSN damage were collected. For the outcome measurements, the number of patients with a sensory deficit, the mean surface of any sensory deficit, the Lysholm score and patient satisfaction were extracted. When multiple follow-up evaluations were performed, only the data corresponding to the final follow-up were extracted.
Assessment of risk of bias and quality of evidence
The risk of bias was evaluated according to the standardized Cochrane Database questionnaire [7]. The selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), reporting bias (selective reporting) and other bias were rated as “high risk”, “low risk” and “unclear risk”. Each item for each study was reported in a table and a summary table reporting the percentage of studies with a specific bias risk was produced. The purpose of the assessment of risk of bias was to provide a descriptive summary of the main sources of potential bias in the included studies. Articles were not excluded on the basis of the assessment.
The overall quality of evidence for each outcome was graded as “high”, “moderate”, “low” and “very low” according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines [2], based on study design, risk of bias, inconsistency, indirectness, imprecision and publication bias.
Statistical analysis
The meta-analysis was performed using RevMan V.5.0.18.33 (the Cochrane Collaboration, Copenhagen, Denmark). Continuous variables were extracted and analyzed as the mean ± standard deviation (SD). If the SD was not reported, the corresponding author was contacted and asked to provide the statistics. In the event of no response, the SD was calculated from the available data, according to a validated formula [5]. If it was not possible to calculate the SD from the available data, the highest SD was used. A first meta-analysis was performed including only RCTs, and a second meta-analysis was performed including all the studies independently of study design. The mean difference (MD) and 95% confidence interval (CI) were calculated for continuous variables. The relative risk (RR) and 95% CI, along with the Relative Risk Reduction (RRR) and the Number Needed to Treat (NNT), were calculated for dichotomous variables. We tested for heterogeneity using the Chi-square and Higgins’ I2 tests [6]. Data were pooled using a Mantel–Haenszel random-effects model if the statistical heterogeneity was > 50% (I2 test); a fixed-effects model was used if the statistical heterogeneity was below 50% [6]. Publication bias was investigated with a funnel plot if more than 10 studies were available for a specific outcome. A p value of < 0.05 was considered statistically significant in all analyses.
Results
Article selection
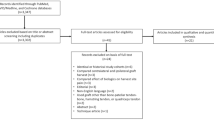
The initial search resulted in a total of 355 articles (Online Appendix 1). After the removal of duplicates, the abstracts of 204 papers were screened. Of these, 25 articles were further assessed by full-text evaluation which resulted in the exclusion of 17 articles due to their not meeting the inclusion criteria, thereby leaving eight articles for inclusion in the final meta-analysis. The investigators were unanimous during the eligibility assessment of screened articles; thus, a consultation with the senior author was not necessary. The selection process and reasons for exclusion are summarized in Fig. 1.
Study characteristics
Of the eight articles included in this meta-analysis, six studies compared vertical and oblique incision, one study compared horizontal and vertical incision and one study compared all three incisions. The harvest of HTs was performed through a vertical incision in 329 patients, through an oblique incision in 195 patients and through a horizontal incision in 151 patients. Seven studies compared patient demographics between groups and did not report any significant differences in age, gender, meniscal lesion or incision length, which varied from 30.7 to 41.0 mm. A random-effect meta-analysis of the two RCTs that compared vertical and oblique incisions and reported the incision length did not reveal any significant difference in incision length (p = 0.25) (Fig. 2a). This result was confirmed by the random-effect meta-analysis of all the five studies that reported this outcome (p = 0.36) (Fig. 2b). Two studies compared vertical and horizontal incisions, of which one did not report any significant differences in incision length and one did not provide the data.
The clinical IPBSN deficit was defined as “hypoesthesia”, “dysesthesia” or “sensory disturbance”. Evaluations were performed using light touch [10, 13, 16], palpation [22], pin prick [25] or blunt needle [28]. One study used patient self-assessment of the IPBSN injury [17] and one study performed an instrumental evaluation of IPBSN deficit with an electrophysiological study of sensory nerve potentials [30] (Tables 1, 2, 3).
Vertical versus oblique incision
Clinical deficit
Three studies [13, 16, 30] did not report significant differences between the two incisions, three studies [17, 25, 28] reported a significantly higher incidence of IPBSN injury in the case of vertical incision and one study [10] did not perform a statistical analysis that was sufficient in order to draw conclusions. When a fixed-effect meta-analysis of the three RCTs was performed, a significant RR of 2.39 (p < 0.0001) was reported when a vertical incision was performed (Fig. 3a), corresponding to an NNT of 4. This trend was confirmed by the random-effect meta-analysis, of all included studies (RR = 1.65, p = 0.02; NNT = 5) (Fig. 3b).
a The random-effect meta-analysis of clinical deficit of the infra-patellar branch of the saphenous nerve (IPBSN) revealed a significantly increased risk ratio (RR) for vertical incision compared with oblique incision in the randomized controlled trials. b The RR for IPBSN injury was increased for vertical incision when meta-analysis of all studies was performed. c The random-effect meta-analysis of the area of deficit revealed a MD in favor of vertical incision
Area of sensory deficit
Three studies [17, 25, 28] (including one RCT) reported a significantly wider area of neurologic deficit in the case of vertical incision, while one study [13] did not report any significant differences. Since only one RCT reported this outcome, a meta-analysis of RCTs was not performed. However, when the random-effect meta-analysis of all studies was performed, a significant MD of 22.91 cm2 (p = 0.04) (Fig. 3c) was reported, with a greater area of sensory deficit in the vertical incision group.
Lysholm score
Two studies evaluated the Lysholm score and did not find any significant difference depending on the incision [13, 30]. Since only one RCT reported this outcome, a meta-analysis was not performed for RCTs. However, when a fixed-effect meta-analysis was performed including both studies, a non-significant MD of 0.13 points was found (ns) (Fig. 4a).
Patient satisfaction
Two studies, both RCTs, conclusively reported no significant difference in subjective satisfaction based on the incision [25, 30]. When a fixed-effect meta-analysis was performed, a non-significant MD of 0.13 points was found (p = 0.94) (Fig. 4b).
Vertical vs horizontal incision
Clinical deficit
Clinical neurologic deficit was evaluated in two studies, both of which reported a significantly higher incidence of IPBSN injury with vertical incision [22, 25]. Since only one RCT reported this outcome, a meta-analysis of RCTs was not performed. However, when a fixed-effect meta-analysis of the comparative studies was performed, a significant RR of 2.45 (p < 0.0001) was reported in the event of vertical incision (Fig. 5), corresponding to an NNT of 4.
Area of sensory deficit
One study evaluated the area of neurologic deficit and found that a vertical incision was associated with a greater area of deficit [25].
Satisfaction
No significant difference in terms of subjective satisfaction was reported by the only study that evaluated this [25].
Oblique vs horizontal incision
One study compared the outcomes after oblique or horizontal incision [25]. However, no significant differences regarding clinical deficit, area of deficit or patient satisfaction were found.
Risk of bias assessment
Of the eight studies included in this meta-analysis, three were RCTs, three were prospective comparative studies and two were retrospective comparative studies. All the studies presented some “high risk” or “unclear risk” of bias (Figs. 6, 7).
The assessors were generally not blinded to patient condition due to the lack of surgical incision concealment with the inevitable increased risk of selection and detection bias. Only one study specified that the assessor of the outcome was not involved in surgery. Patients were not blinded to their condition, but it is likely that their knowledge of a given incision would not have been able to influence the subjective outcomes since no placebo treatment had been administered. The performance bias was, therefore, regarded as “low risk” in most of the studies. Since no patients were lost to follow-up, no studies presented a high risk of attrition bias. Considering this bias, the lack of randomization of several studies and the high heterogeneity, the overall quality of evidence was rated as “low” to “moderate” (Figs. 8, 9).
Discussion
The most important finding of the present study was that the implementation of a vertical incision technique to harvest HTs in ACL reconstruction significantly increased the risk of iatrogenic injury to the IPBSN compared with both oblique and horizontal techniques. The relationship between clinical outcome and incision technique has been modestly investigated in literature, but the direction of the incision does not appear to impact the clinical or patient-reported outcome.
This study comprised eight studies comparing vertical incision with oblique, vertical with horizontal, or all three techniques (Fig. 10). The studies were homogeneous with regard to patient demographics such as age, gender and the presence of combined meniscal lesion. In terms of surgical variables, the length of the incision did not differ between groups and a cortical fixation was used in 75% of the studies [17, 25, 28, 30]. The risk of an iatrogenic injury to the IPBSN due to tendon harvest was almost double-fold increased when a vertical incision was performed rather than an oblique incision and it was consequently estimated that this injury could have been avoided in one of four patients by implementing an oblique incision rather than a vertical one. Moreover, a significantly larger area of sensory deficit was found when using a vertical approach. The vertical incision was also associated with a significantly increased risk of IPBSN injury and a larger area of sensory deficit when compared with a horizontal incision, although this was more sparsely investigated. No differences in terms of deficits related to IPBSN injury were reported between horizontal and oblique incisions [25].
Interestingly, no correlation between the presence of injury to the IPBSN and clinical outcome as reported by Lysholm was found and patient satisfaction was not affected either. This suggests that the present methods for harvesting HTs might actually be clinically equivalent. However, it is important to remember that the patient-reported outcome was investigated in a minority of the studies [13, 30], which somewhat limits the certainty of these results and may underestimate the correlation between the nerve injury and clinical parameters. There might also be an intrinsic insufficiency in detecting concerns related to neurologic injury since the Lysholm questionnaire, which was applied for clinical evaluation in the studies, does not comprise questions specifically related to neurologic symptoms. Nevertheless, given the fact that this meta-analysis highlights a considerably increased risk of IPBSN injury when a vertical incision technique is used and that the choice of one incision over another does not imply any particular costs or difficulties, we suggest that thorough consideration should be taken before performing a vertical incision and that the surgeon should consider other alternatives. Since the implementation of either a horizontal or an oblique incision did not affect the risk of IPBSN injury, the choice between the two remains mainly dependent on the surgeon’s preference. However, the oblique incision is favored because it potentially combines the benefits of both vertical and horizontal incisions by enabling correct exposure of the tendons, permits the localization of an appropriate starting point for tibial tunnel drilling [13, 18] and partly manages to avoid the contact area in the anterior aspect of the leg. Other aspects that should be considered in order to minimize the risk of nerve injury involve correct knee positioning, a small skin incision and careful wound suture [20,21,22, 24].
The present meta-analysis has some limitations that warrant consideration. First, only three RCTs could be included [16, 25, 30]. These RCTs were, however, limited by factors such as an imprecise description of methods for randomization and concealment, with the possible effect of introducing bias. On the other hand, the blinding of the incision would not have been possible in the clinical setting and, although it might introduce a significant source of bias among the investigators, it is most likely that patients lack any knowledge of the possible effects based on incision technique when subjectively evaluating the outcome. Due to the limited number of RCTs, a pure meta-analysis was performed only on a small number of patients and on a subset of outcomes. However, when including also the studies with a comparative study design in a mixed-method meta-analysis, the direction and significance of the results for each outcome were not altered. Moreover, the meta-analysis of purely RCTs showed a more evident effect of vertical incision compared with oblique incision in terms of increased risk of a clinically relevant IPSB injury, which strengthens the findings. Another limitation was that only some of the included studies reported a clear description of the surgical treatment and/or evaluation methods. With regard to the evaluation of nerve injury and the assessment of outcome, the methods varied significantly among studies. A clinical evaluation was commonly performed, whereas only one trial performed an electrophysiological evaluation to assess IPBSN injury objectively [25]. It should be emphasized that the definition and evaluation of injury to the IPBSN was highly heterogeneous among the included studies, which means that the evidence obtained from this meta-analysis should be interpreted with care. Because of the heterogenous definitions of hypoesthesia and the variable evaluation methods, it is unclear if sensory disturbance clinically affects the patient’s outcome. However, an oblique incision technique minimizes the potential risk for an inferior patient satisfaction by decreasing the risk of iatrogenic injury to the IPBSN during hamstring tendon harvest. This should be taken into account in the planning of every procedure using HTs tendons to reduce the potential adverse events related and patient discomfort related to the surgery.
Conclusion
The risk of iatrogenic injury to the IPBSN during HT harvest was significantly greater when a vertical incision was performed rather than an oblique or a horizontal incision. However, the incision technique did not influence clinical outcome or patient satisfaction after ACL reconstruction. Care is recommended during the HT harvest procedure in order to minimize the risk of iatrogenic injury to the IPBSN.
References
Arthornthurasook A, Gaew-Im K (1990) The sartorial nerve: its relationship to the medial aspect of the knee. Am J Sports Med 18:41–42
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406
Figueroa D, Calvo R, Vaisman A, Campero M, Moraga C (2008) Injury to the infrapatellar branch of the saphenous nerve in ACL reconstruction with the hamstrings technique: clinical and electrophysiological study. Knee 15:360–363
Gianotti SM, Marshall SW, Hume PA, Bunt L (2009) Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport 12:622–627
Hedges LV, Vevea JL (1998) Fixed-and random-effects models in meta-analysis. Psychological methods 3:486
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Bmj 327:557–560
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of intervention version 5.1.0. The Cochrane Collaboration. http://handbook.cochrane.org
Hunter LY, Louis DS, Ricciardi JR, O’Connor GA (1979) The saphenous nerve: its course and importance in medial arthrotomy. Am J Sports Med 7:227–230
Jameson S, Emmerson K (2007) Altered sensation over the lower leg following hamstring graft anterior cruciate ligament reconstruction with transverse femoral fixation. Knee 14:314–320
Kaczmarczyk J, Sergiew M, Adamcewicz F, Kruczynski J (2007) Lower limb dysaesthesia after anterior cruciate ligament reconstructions with hamstring tendons. A comparison of vertical versus oblique harvest site incisions. Chir Narzadow Ruchu Ortop Pol 72:247–248
Kalthur SG, Sumalatha S, Nair N, Pandey AK, Sequeria S, Shobha L (2015) Anatomic study of infrapatellar branch of saphenous nerve in male cadavers. Ir J Med Sci 184:201–206
Kerver AL, Leliveld MS, den Hartog D, Verhofstad MH, Kleinrensink GJ (2013) The surgical anatomy of the infrapatellar branch of the saphenous nerve in relation to incisions for anteromedial knee surgery. J Bone Joint Surg Am 95:2119–2125
Kjaergaard J, Fauno LZ, Fauno P (2008) Sensibility loss after ACL reconstruction with hamstring graft. Int J Sports Med 29:507–511
Lai CC, Ardern CL, Feller JA, Webster KE (2017) Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. https://doi.org/10.1136/bjsports-2016-096836
Lefevre N, Klouche S, Mirouse G, Herman S, Gerometta A, Bohu Y (2017) Return to sport after primary and revision anterior cruciate ligament reconstruction: a prospective comparative study of 552 patients from the FAST cohort. Am J Sports Med 45:34–41
Leite ML, Cunha FA, Costa BQ, Andrade RM, Diniz Junior JH, Temponi EF (2016) Relationship between peri-incisional dysesthesia and the vertical and oblique incisions on the hamstrings harvest in anterior cruciate ligament reconstruction. Rev Bras Ortop 51:667–671
Luo H, Yu JK, Ao YF, Yu CL, Peng LB, Lin CY et al (2007) Relationship between different skin incisions and the injury of the infrapatellar branch of the saphenous nerve during anterior cruciate ligament reconstruction. Chin Med J (Engl) 120:1127–1130
Marder RA, Raskind JR, Carroll M (1991) Prospective evaluation of arthroscopically assisted anterior cruciate ligament reconstruction. Patellar tendon versus semitendinosus and gracilis tendons. Am J Sports Med 19:478–484
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Mohtadi NG, Chan DS, Dainty KN, Whelan DB (2011) Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005960.pub2Cd005960
Pagnani MJ, Warner JJ, O’Brien SJ, Warren RF (1993) Anatomic considerations in harvesting the semitendinosus and gracilis tendons and a technique of harvest. Am J Sports Med 21:565–571
Papastergiou SG, Voulgaropoulos H, Mikalef P, Ziogas E, Pappis G, Giannakopoulos I (2006) Injuries to the infrapatellar branch(es) of the saphenous nerve in anterior cruciate ligament reconstruction with four-strand hamstring tendon autograft: vertical versus horizontal incision for harvest. Knee Surg Sports Traumatol Arthrosc 14:789–793
Parkkari J, Pasanen K, Mattila VM, Kannus P, Rimpela A (2008) The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population-based cohort study of 46,500 people with a 9 year follow-up. Br J Sports Med 42:422–426
Portland GH, Martin D, Keene G, Menz T (2005) Injury to the infrapatellar branch of the saphenous nerve in anterior cruciate ligament reconstruction: comparison of horizontal versus vertical harvest site incisions. Arthroscopy 21:281–285
Sabat D, Kumar V (2013) Nerve injury during hamstring graft harvest: a prospective comparative study of three different incisions. Knee Surg Sports Traumatol Arthrosc 21:2089–2095
Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ (2017) Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. https://doi.org/10.1007/s11999-017-5278-9
Sanders B, Rolf R, McClelland W, Xerogeanes J (2007) Prevalence of saphenous nerve injury after autogenous hamstring harvest: an anatomic and clinical study of sartorial branch injury. Arthroscopy 23:956–963
Sipahioglu S, Zehir S, Sarikaya B, Levent A (2017) Injury of the infrapatellar branch of the saphenous nerve due to hamstring graft harvest. J Orthop Surg (Hong Kong) 25:2309499017690995
Spicer DD, Blagg SE, Unwin AJ, Allum RL (2000) Anterior knee symptoms after four-strand hamstring tendon anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 8:286–289
Tavakoli Darestani R, Bagherian Lemraski MM, Hosseinpour M, Kamrani-Rad A (2013) Electrophysiological assessment of injury to the infra-patellar branch(es) of the saphenous nerve during anterior cruciate ligament reconstruction using medial hamstring auto-grafts: vertical versus oblique harvest site incisions. Arch Trauma Res 2:118–123
Warren LF, Marshall JL (1979) The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am 61:56–62
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Grassi, A., Perdisa, F., Samuelsson, K. et al. Association between incision technique for hamstring tendon harvest in anterior cruciate ligament reconstruction and the risk of injury to the infra-patellar branch of the saphenous nerve: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 26, 2410–2423 (2018). https://doi.org/10.1007/s00167-018-4858-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4858-x