Abstract
Purposes
The focus in the evaluation of total knee arthroplasty has shifted from objective measures of implant position and knee function, to patient-reported outcome measures (PROMs). The relation between these two measures was investigated and the possibility of prediction of the patient satisfaction level was evaluated by defining thresholds for improvement of (1) range of motion (ROM), (2) 6-min walk test (6MWT), (3) sit-to-stand test (STS) and (4) quadriceps force after TKA?
Methods
Fifty-seven patients were prospectively tested at preoperative and 6 months postoperative intervals. The ROM, 6MWT, STS-test and quadriceps force were evaluated. Two clusters were created based on the postoperative KOOS, OKS and the satisfaction subscore of the new KSS, cluster 1 consisted of patients with good to excellent PROMs, cluster 2 of patients with poorer PROMs. Patients in each cluster were more similar to each other than to those in the other cluster. Receiver operating characteristic (ROC)-curve analysis was used to identify thresholds for the functional outcomes that established cluster allocation. Multiple logistic regression was used to define a model to predict cluster allocation.
Results
Patients with high postoperative PROMs (cluster 1 allocation) showed higher postoperative functional outcomes (p < 0.05). Thresholds for the improvement of ROM (≥ 5°, OR 6.3, 95% CI 1.23–31.84), 6MWT (≥ 50 m, OR 8.2, 95% CI 1.61–42.18) STS (≥ 1.05 s, OR 3, 95% CI 0.56–16.07) and normalized Q4 force (≥ 1.5 N/BMI, OR 2.5, 95% CI 0.49–12.89) were found to be predictors of cluster allocation. A model to predict the cluster allocation contained gender, ROM improvement and 6MWT improvement (sensitivity 91.1%, specificity 75%).
Conclusions
Thresholds for improvement of functional parameters can predict the patient satisfaction cluster. Patients, who are male, improve on the 6-min walk test with 50 m or more and have an increased range of motion of 5° or more, compared to the preoperative situation, are 6–8 times more likely of being satisfied after TKA. These tests are easy to use in clinical practice and can predict the level of patient satisfaction after TKA.
Level of evidence
Level II, prognostic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, patient-reported outcome measures (PROMs) receive significantly more attention as a tool to measure the outcome of total knee arthroplasty (TKA) [1]. This patient-centric philosophy uses patient satisfaction as a metric of quality of patient care as opposed to the traditional, physical outcome measurements. The relation between these subjective and objective measurement tools would seem self-evident, but earlier results have been inconclusive [2,3,4,5].
The mean impetus for this paradigm shift is the understanding that concerns and priorities of patients and surgeons may differ [5, 6]. Despite good scores in the traditional outcome measurement tools developed in the eighties [7,8,9,10], only 68–93% of the patients report satisfaction after TKA [6, 11,12,13,14,15,16]. Considering this discrepancy, the current research project is focused at pinning the underlying causes of dissatisfaction. Whilst PROMs are deemed relevant by policy makers, registries and general public, the relation between PROMs and objectively measured functional tests remains to be demonstrated by the orthopaedic community.
The aim of this paper is twofold; (1) can we analyze whether the functional outcomes are different between patients with high and low PROMs after TKA, and (2) if so, can the PROMs be predicted by the improvement of (1) the range of motion, (2) the quadriceps force, (3) the sit-to-stand test (STS), (4) the 6-min walk test (6MWT). This research investigates the relation between these objective outcomes and subjective ‘patient satisfaction’ by setting thresholds for these functional tests. This would help to establish the necessary improvement in physical outcome necessary to achieve patient satisfaction after TKA.
Materials and methods
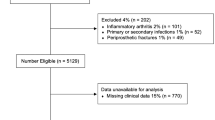
After obtaining institutional review board approval (EC number B670201419601), informed consent was obtained from 77 patients planned for primary TKA at our center. These patients were subsequently evaluated preoperatively and followed prospectively. Twenty patients refused to come back for the postoperative testing at 6 months for personal reasons. Fifty-seven patients (37 female, 20 male) were evaluated preoperatively and at 6 months postoperatively. Mean age of the patients was 64 years (SD 9.0) with a mean BMI of 31 (SD 5.7).
Variables and outcome measures
Maximum flexion and flexion contracture were measured by a single investigator using a goniometer to the nearest 5°, with the patient in supine position. ROM was calculated by subtracting flexion contracture from maximum flexion. Jakobsen et al. demonstrated that even a change of knee joint ROM less than 5° could be detected by experienced testers using a standardized protocol, with very good intra-tester reliability (ICC 0.89–0.97) and inter-tester reliability (ICC 0.92–0.96) [17].
Quadriceps and hamstring force were measured using maximum voluntary isometric contraction. This was tested with a hand-held dynamometer (Microfed Handheld Dynamometer®, HHD) by a single investigator [18]. Quadriceps force was measured with the patient sitting down holding their leg in 60° of flexion. The handheld dynamometer was placed on the distal anterior third of the lower leg. Subsequently, the patient was asked to sustain maximal force during extension. The hamstring force was measured in a prone position. The leg was positioned in 30° flexion, whilst the handheld dynamometer was placed on the distal posterior third of the lower leg. Three trials were performed on each side, and the maximum voluntary force generated normalized to the participant’s weight was used to quantify quadriceps and hamstrings strength.
To evaluate the sit-to-stand (STS) test, patients were requested to sit on a standard chair without armrests. Their feet were placed comfortably on the floor with knees flexed slightly more than 90°. Patients were then asked to stand up to a fully upright standing position five times as quickly as possible without using their hands (arms folded across the chest). Timing with a stopwatch started on “start” (after a countdown from 3) and ended on the fifth stand. This test is easy to perform in clinical practice and has shown excellent intra- and interrater reliability (ICC 0.89) in patients with hip or knee OA. It was also found to accurately predict disability across populations [19].
The procedure for the 6MWT was based on published guidelines [6]. A 40-m long section of the hallway was demarcated for this test. The participant was instructed to walk as far as possible for 6 min, up and down the demarcated path, pivoting to turn at the end of each lap. Timing commenced as the participant stepped over the start line. Standardized encouragement was given to the patient after each minute. The patient was instructed to stop at 6 min, or earlier if they were unable to complete 6 min, and to maintain their position whilst the assessor measured the final partial lap with a validated measurement tool. High repeatability of this test has been established in knee osteoarthritis patients (ICC 0.94) [20].
Three different PROM tools were used. (1) The knee injury and osteoarthritis outcome score (KOOS) consists of 42 knee-related items, with each item scored from 0 to 4. Five subscales of symptoms, pain, activities of daily living (ADL), sports and quality of life (QOL) are converted to 100 points. Decreasing scores indicate worsening of knee symptoms [9, 21]. Since a low completion rate of the sports subscale was found in our study, this subscale was excluded from the analysis. (2) The satisfaction subscore of the 2011 Knee Society Score (KSS) consists of five questions (40 points). The higher the score, the better the outcome [22, 23]. (3) The Oxford Knee Score (OKS).consists of twelve questions assessed on a Likert scale with values from 0 to 4, a summative score is then calculated, where 48 is the best possible score (least symptomatic) and 0 is the worst possible score (most symptomatic) [21] The Oxford Knee Score was only evaluated at 6 months postoperative.
Dutch translations of all these scores have been validated [8, 21, 23] for use in Dutch speaking countries or regions including Flanders where this study was conducted.
Statistical analysis
Statistical analysis was performed using SAS 9.4 (SAS Institute Inc, Cary, NC, USA) and SPSS version 22 (IBM Corp., Chicago, IL, USA).
A uniform agglomerative to-step cluster methodology was applied to identify groups of patients with the same characteristics. The input variables were the PROMs KOOS [Pain, Symptoms, ADL and QOL, OKS and KSS (Satisfaction)]. The number of clusters was specified to be 2 using Schwarz’s Bayesian Critera (BIC).
Overall goodness-of-fit of clusters was evaluated using the silhouette coefficient. Silhouette measure of less than 0.2 was classified as poor, between 0.2 and 0.5 as fair and more than 0.5 as good solution quality, of which a good solution quality (0.6) was found in this study [24]. Predictor importance (PI) was shown to be the highest for KSS Satisfaction (PI = 1.00), then KOOS Symptoms (PI = 0.75), KOOS Pain (PI = 0.66), KOOS QOL (PI = 0.62) and KOOS ADL (PI = 0.28). Patients in each cluster were more similar to each other than to patients in the other cluster.
After cluster definition, independent T tests were used to compare the between-group differences and paired T tests were used to evaluate the within-group differences.
ROC-curve analysis was used to identify thresholds for the functional outcomes that identified patient satisfaction group according to the aforementioned PROMs.
The Youden’s index (which is the point where Sensitivity + Specificity-1 is the highest) was used to define the cut-off. Maximizing this index allowed us to find an optimal cut-off point independently from the prevalence. These cut-off values were used to dichotomize the improvement in functional outcomes. The dichotomized parameters were then used to determine a multiple logistic regression model that can predict the odds-ratio of being in the cluster with high PROMs (cluster 1).
Since the nature of these exhaustive studies generally leads to study groups that are relatively small, comparable studies were evaluated. After evaluating the sample size of comparable studies, a group of minimum 50 patients was aimed for [5, 25, 26].
Results
Two-step cluster analysis based on the postoperative KOOS, OKS and KSS satisfaction subscore led to the formation of two clusters. Cluster 1 contained 45 patients with high PROM scores, whilst cluster 2 contained 12 patients with low to medium PROM scores (silhouette coefficient = 0.6). The cluster specific demographic information, functional scores and postoperative PROMs are listed in Tables 1, 2 and 3.
Preoperatively, the normalized quadriceps force and the KOOS ADL subscore were significantly higher in cluster 1 (cluster with high PROM scores). All other preoperative functional tests and preoperative PROMs were similar between the two clusters (Tables 2, 3).
Postoperatively, all PROM subscores as well as all functional outcomes, except 6MWT, were significantly higher in cluster 1 (Tables 2, 3).
A significant improvement in PROM scores and functional outcome scores was found in cluster 1, but not in cluster 2 (Tables 2, 3).
Cut-off values for each functional outcome improvement were based on the Youden point of the ROC curve (Table 4; Fig. 1). These cut-off values were used to dichotomize the functional outcomes and odds ratios were evaluated (Table 4). Backward logistic regression with all dichotomized functional outcomes allowed us to retain a significant model containing ROM and 6MWT improvement. While simple logistic regression of the demographics showed near missed significance for gender, this variable was added to the model, with the chance of being in the cluster with high PROMs being higher for male patients (OR 8.0, CI 0.95–67.69, p = 0.055, AUC 0.67).
The final multiple logistic regression model consisted of gender, improvement of ROM ≥ 5° and improvement of 6MWT ≥ 50 m. This model was statistically significant (p < 0.01) with a sensitivity of 91.1% and a specificity of 75%. Odds ratios were 10.85 (95% CI 1.69–69.56) for improvement of 6MWT, 2.56 (95% CI 0.38–17.06) for ROM and 13.17 (95% CI 1.06–163.83) for gender (Fig. 2).
Discussion
The most important finding of the present study was the establishment of cut-off values for improvement of ROM and 6MWT enabling us to predict the classification into clusters based on PROMs. This is, to our knowledge, the first study using cluster analysis to group different PROMs into clusters that represent satisfaction levels. While this is a common technique in psychology, genetics, microbiology and marketing, it may be applied to subjective outcomes after TKA, as these represent certain patient profiles [27, 28]. The clusters proposed in this study represent one group of patients with good to excellent PROMs and another group with poorer results. Patients in each cluster are more similar to each other than to those in the other cluster. While significant between-cluster differences for all PROMs are found, this implies a good execution of the two-step cluster analysis [29].
This between-cluster difference was also observed for all postoperative functional outcomes. The cluster with the high PROM scores consistently included the patients with better ROM and quadriceps force, further walking distance and faster execution of the STS test. Furthermore, patients in this cluster experienced a significant improvement for all PROMs and functional outcomes, compared to the patients in cluster 2. Considering these differences, a relation between the PROMs and the functional outcomes can be postulated, especially with regard to the difference in improvement between the clusters.
Besides the postoperative difference between the clusters, patients in the cluster with high postoperative PROMs also exhibited significant stronger quadriceps strength and a higher KOOS ADL subscore preoperatively. However, a different gender distribution between the clusters may play a role with only one male in the cluster with low PROMs. Previous studies have reported that men undergoing TKA have significantly higher physical function scores than women [20, 30, 31]. Additionally, higher preoperative quadriceps force was shown to result in decreased postoperative pain, and improved quality of life [32]. Therefore pre- and postoperative quadriceps training should probably be recommended to improve patient satisfaction.
Since the two clusters exhibited a distinct difference in functional improvement between the pre- and postoperative setting, we investigated whether cut-off values would be appropriate to predict the cluster allocation.
Considering the 6MWT, patients who improved 50 ms or more were more than 8 times more likely of having high PROMs and thus being satisfied with the result of their TKA surgery. This cut-off value is similar to the results of Naylor et al. who described the threshold of improvement for the 6MWT, at 26 weeks post TKA, between 26 and 55 m [33]. While they used a 7-point transition scale of improvement, we used the aforementioned clusters to define the threshold. Ko et al. analyzed the absolute walking distance and found that the WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) was significantly predicted by the 6MWT [23]. In our study, the absolute walking distance did not differ between the two clusters. Therefore, we recommend focusing on the improvement in walking distance, as this reflects the postoperative progression.
Patients with a postoperative increase in ROM of 5° or more were six times more likely to be classified in the ‘satisfied cluster’. While patients in this cluster gained 12°on average, the ROM in the ‘less satisfied cluster’ barely increased by 2°. We acknowledge that it is difficult to accurately measure these small increments in ROM, but Jakobsen et al. demonstrated that a change in knee joint ROM of less than 5° can be detected by experienced testers using a standardized protocol, with very good intra-tester reliability (ICC 0.89–0.97) and inter-tester reliability (ICC 0.92–0.96) [17].
The influence of ROM on patient satisfaction after TKA, which is indicated in our results, is in contradiction with the study by Miner et al. [4]. They observed that patient satisfaction and quality of life are driven by the overall functional status and not influenced by the ROM of the index knee. Again, our findings suggest the improvement of ROM is the important factor associated with satisfaction.
Even though improvement in the STS test was not withheld as significant predictor, the ‘satisfied cluster’ has a significant faster STS performance time but also a significant improvement compared to the ‘less satisfied cluster’. The cut-off value for the improvement of the STS test of 1.05 s is associated with a three times higher likelihood of high PROM score cluster allocation. Until now, clear STS-test cut-off values for TKA patients have not been defined. Estimated values for normal performance for community-dwelling elderly, older than 60, are found to be 11.4–14.8 s [34]. While all patients in this study were community-dwelling, the recorded STS values were slower (cluster 1: 15 s and cluster 2: 20 s on average). The relatively short follow-up of 6 months may account for this finding.
Another important parameter correlated with functional performance [35, 36] is the normalized quadriceps force. Although it was not a significant predictor of cluster allocation, an increase of 1.5N/BMI or more, represented an odds ratio for high PROM scores of 2.5. Better quadriceps strength has been observed to increase the walking distance in the 6MWT and improve the STS-test time [25, 35, 37]. As these functional parameters are interrelated, the 6MWT may illustrate the quadriceps force.
Whilst the thresholds for increase in ROM and 6MWT were established as significant predictors, they were also retained by the backward logistic regression model. Since an unequal gender distribution was observed, the model was adjusted for gender. The final model with a sensitivity of 91% and a specificity of 75% was, therefore, considered a clinically relevant prediction tool. Male patients improving by more than 50 ms on the 6MWT and by more than 5° ROM were 6–8 times more likely to be classified in the ‘satisfied cluster’.
There are some limitations to the present study. First, the follow-up of 6 months is relatively short and further improvement could occur later on. However, a steep clinical improvement is usually only noticed between 3 and 6 months after TKA, followed by a significantly slower, more gradual improvement up to 2 years postoperatively [38].
A second limitation is related to the floor- and ceiling effects of the PROMs. Ceiling effects of the KOOS pain subscale have been reported to be 15% at 6 months and 22% at 12 months [39]. Since ceiling effects occur when a majority of the patients reach the top scores, further improvements in outcome may remain undetected. However, as the cut-off for floor and/or ceiling effects should not exceed 15%, the use of the KOOS at 6-months does not pose a problem [19]. Previous studies showed no occurrences of floor nor ceiling effects of the KSS at 6 months after TKA [40], which make the KSS satisfaction a strong evaluation tool for outcome after TKA. A third limitation is the relatively small sample size. Although there were statistically significant differences within the data, larger patient groups would permit more substantial comparisons. However, the nature of these exhaustive studies generally leads to relatively small study groups as reflected in the significant number of drop-outs after the initial testing. Nevertheless, the sample size of this research was comparable to other published studies evaluating functional outcomes [5, 25, 26]. Finally, we did not correct the model for age. However, Bourne et al. could only demonstrate a weak correlation for poorer satisfaction with advancing age. Robertson et al. did not find any correlation between satisfaction and age [2].
The new cut-off values for improvement of ROM and 6MWT established in this study, could be helpful in clinical practice. It could be interesting to use these tests and their cut-off values as markers for patient satisfaction. In patients who are not likely to achieve the cut-off for satisfaction, rehabilitation should be intensified. This could help patients to reach their functional goals and hopefully lead to a higher satisfaction with the TKA. Whilst a correlation between functional outcomes and PROMs seems intuitive, earlier results have been inconclusive [2,3,4,5]. This study, however, provides new cut-off values which provide a useful addition to the PROMs in the evaluation of TKA patient populations.
Conclusions
The current study established cut-off values for the improvement of ROM and 6MWT 6 months after TKA, predicting the classification into clusters based on PROMs. To increase the likelihood of being satisfied, patients should be able to walk 50 m further during the 6MWT and increase their ROM by 5° or more as compared to the preoperative situation. This model has a sensitivity of 91% and a specificity of 75%, and can easily be applied in clinical practice.
References
Rolfson O, Bohm E, Franklin P, Lyman S, Denissen G, Dawson J, Dunn J, Eresian Chenok K, Dunbar M, Overgaard S, Garellick G, Lübbeke A (2016) Patient-reported outcome measures in arthroplasty registries Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty Registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop 87(Suppl 1):9–23
Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW (1996) Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplast 11:831–840
Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y (2013) Postoperative alignment and ROM affect patient satisfaction after TKA knee. Clin Orthop Relat Res 471:127–133
Miner AL, Lingard EA, Wright EA, Sledge CB, Katz JN (2003) Knee range of motion after total knee arthroplasty: How important is this as an outcome measure? J Arthroplast 18:286–294
Vissers MM, de Groot IB, Reijman M, Bussmann JB, Stam HJ, Verhaar J (2010) Functional capacity and actual daily activity do not contribute to patient satisfaction after total knee arthroplasty. BMC Musculoskelet Disord 11:121
Bullens PHJ, van Loon CJM, de Waal Malefijt MC, Laan RFJM., Veth RPH (2001) Patient satisfaction after total knee arthroplasty. J Arthroplast 16:740–747
Insall J, Tria AJ, Scott WN (1973) The total condylar knee prosthesis: the first 5 years. Clin Orthop Relat Res 145:68–77
Insall JN, Kelly M (1986) The total condylar prosthesis. Clin Orthop Relat Res 205:43–48
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Vince KG, Insall JN, Kelly MA (1989) The total condylar prosthesis. 10- to 12-year results of a cemented knee replacement. J Bone Joint Surg Br 71:793–797
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Lee WC, Kwan YH, Chong HC, Yeo SJ (2017) The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc 25(11):3354–3359
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Van Onsem S, Van Der Straeten C, Arnout N, Deprez P, Van Damme G, Victor J (2016) A new prediction model for patient satisfaction after total knee arthroplasty. J Arthroplast 31:2660–2667
Scott CEH, Howie CR, MacDonald D, Biant LC (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br 92:1253–1258
Stone OD, Duckworth AD, Curran DP, Ballantyne JA, Brenkel IJ (2017) Severe arthritis predicts greater improvements in function following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(8):2573–2579
Jakobsen TL, Christensen M, Christensen SS, Olsen M, Bandholm T (2010) Reliability of knee joint range of motion and circumference measurements after total knee arthroplasty: does tester experience matter? Physiother Res Int 15:126–134
Wadsworth CT, Krishnan R, Sear M, Harrold J, Nielsen DH (1987) Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys Ther 67:1342–1347
Dowsey M, Choong FM (2013) The utility of outcome measures in total knee replacement surgery. Int J Rheumatol 2013:506–518
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY (2004) Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Jt Surg Am 86–A:963–974
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69
Haverkamp D, Breugem SJM, Sierevelt IN, Blankevoort L, van Dijk CN (2005) Translation and validation of the Dutch version of the Oxford 12-item knee questionnaire for knee arthroplasty. Acta Orthop 76:347–352
Ko V, Naylor JM, Harris IA, Crosbie J, Yeo AET (2013) The six-minute walk test is an excellent predictor of functional ambulation after total knee arthroplasty. BMC Musculoskelet Disord 14:145
Mooi E, Sarstedt M (2011) A concise guide to market research: the process, data and methods using IBM SPSS statistics. Int J Mark Res 53:563–564
Alnahdi AH, Zeni JA, Snyder-Mackler L (2016) Quadriceps strength asymmetry predicts loading asymmetry during sit-to-stand task in patients with unilateral total knee arthroplasty. Knee Surgery Sport Traumatol Arthrosc 24:2587–2594
Stevens-Lapsley JE, Balter JE, Kohrt WM, Eckhoff DG (2010) Quadriceps and hamstrings muscle dysfunction after total knee arthroplasty. Clin Orthop Relat Res 468:2460–2468
Cattell RB (1943) The description of personality. I. Foundations of trait measurement. Psychol Rev 50:559–594
Haldar P, Pavord ID, Shaw DE, Berry MA, Thomas M, Brightling CE, Wardlaw AJ, Green RH (2008) Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med 178:218–224
Reutter A (2003) TwoStep cluster analysis. IBM Software, Bus Anal SPSS, pp 1–5
Fitzgerald JD, Orav EJ, Lee TH, Marcantonio ER, Poss R, Goldman L, Mangione CM (2004) Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum 51:100–109
Nashi N, Hong CC, Krishna L (2014) Residual knee pain and functional outcome following total knee arthroplasty in osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 23(6):1841–1847
Tungtrongjit Y, Weingkum P, Saunkool P (2012) The effect of preoperative quadriceps exercise on functional outcome after total knee arthroplasty. J Med Assoc Thai 95(Suppl 1):S58–S66
Naylor JM, Mills K, Buhagiar M, Fortunato R, Wright R (2016) Minimal important improvement thresholds for the six-minute walk test in a knee arthroplasty cohort: triangulation of anchor- and distribution-based methods. BMC Musculoskelet Disord 17:390
Bohannon RW (2006) Reference values for the five-repetition sit-to-stand test: a descriptive meta-analysis of data from elders. Percept Mot Skills 103:215–222
Mizner RL, Billing S (2005) Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther 35(7):424–436
Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L (2008) Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech 23:320–328
Farquhar SJ, Reisman DS, Snyder-Mackler L (2008) Persistence of altered movement patterns during a sit-to-stand task 1 year following unilateral total knee arthroplasty. Phys Ther 88:567–579
Jones CA, Voaklander DC, Suarez-Alma ME (2003) Determinants of function after total knee arthroplasty. Phys Ther 83:696–706
Dowsey MM, Spelman T, Choong PFM (2016) Development of a prognostic nomogram for predicting the probability of nonresponse to total knee arthroplasty 1 year after surgery. J Arthroplasty 31(8):1654–1660
Van Der Straeten C, Witvrouw E, Willems T, Bellemans J, Victor J (2013) Translation and validation of the Dutch New Knee Society Scoring System©. Clin Orthop Relat Res 471:3565–3571
Acknowledgements
The authors wish to acknowledge Prof. T. Willems and the Department of Rehabilitation Sciences and Physiotherapy, Ghent University for the technical support and providing the handheld dynamometer.
Funding
The article was funded by FWO (Grant no. 12N5117N) and BOF (Grant no. 01AN00513).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Ethical Approval was obtained with the Belgian Registration-number B670201419601.
Informed Consent
All patients completed an informed consent before the testing was performed.
Additional information
Investigation performed at Ghent University Hospital, Belgium.
Rights and permissions
About this article
Cite this article
Van Onsem, S., Verstraete, M., Dhont, S. et al. Improved walking distance and range of motion predict patient satisfaction after TKA. Knee Surg Sports Traumatol Arthrosc 26, 3272–3279 (2018). https://doi.org/10.1007/s00167-018-4856-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4856-z