Abstract
Purpose
Patient-specific instrumentation (PSI) is a technique to plan and position the prosthesis components in unicompartmental knee arthroplasty (UKA) surgery. This study assesses whether the definitive component position in the frontal, sagittal and axial plane is according to the preoperative plan, based on the hypothesis that PSI is accurate.
Methods
Twenty-six patients who had PSI Oxford UKA surgery were included prospectively. The component position in vivo was determined with a postoperative CT-scan and compared with the planned component position using MRI-based digital 3D imaging. Adjustments to the preoperative plan and implanted component sizes during surgery were recorded.
Results
Intraoperatively, no femoral adjustments were performed; 12 tibial re-resections were necessary. The median absolute deviation from the plan in degrees (range) in the frontal, sagittal and axial plane was 1.8° (− 1.5°–6.5°), 2.0° (− 6.5°–8.0°) and 1.0° (− 1.5°–5.0°) for the femoral component, and 2.5° (− 1.0°–6.0°), 3.0° (− 1.0°–5.0°) and 5.0° (− 6.5°–12.5°) for the tibial component. The femoral component is positioned 0.5 (− 1°–2.5°) mm more lateral and 0.8 (− 1.0°–2.5°) mm more anterior. The tibial component is positioned 2.0 (− 5.0–0.0) mm more lateral and 1.3 (− 3.0–6.0) mm more distal. The femoral and tibial default plans were changed four times (15.4%) and nine times (34.6%), respectively, before approval by the surgeon.
Conclusion
PSI in Oxford UKA surgery is reliable and accurately translates the preoperative plan into the in vivo situation, except for the tibial rotational position. The preoperative planning is a crucial step in avoiding re-resections that can cause angular deviations in prosthesis position, especially in tibial component rotational position. It is advised to avoid re-resections and to consider this while planning the PSI procedure.
Level of evidence
Prospective comparative study Level II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) is a surgical procedure with good survival rates [5, 12,13, 14]. Currently, several techniques for outlining the prosthesis exist. New techniques that try to optimise the surgical procedure and the accuracy of prosthesis alignment are still being introduced [7, 9]. Precision in implant placement restores biomechanics of the knee joint and proves to increase the survival of the prosthesis [19]. A recent development is the use of patient-specific instruments (PSI) to determine the appropriate three-dimensional resections of femur and tibia, in preparation of prosthesis placement [11, 15]. In total knee arthroplasty (TKA), a direct comparison study shows that these PSI guides act accurately [1]. Another recent study compares the preoperative plan with the postoperative position based on CT images. However, no studies have been conducted to assess the accurateness of preoperative planning in UKA surgery, and therefore, directly compare the preoperative plan with the achieved position of UKA prostheses in vivo by CT images [6, 18, 20, 21]. The purpose of the present study is to determine whether there is a significant difference between the alignment of the femoral and tibial components as calculated preoperatively and the actually achieved alignment postoperatively calculated by CT images.
The present study analysed the Signature™ (Zimmer-Biomet, Warsaw, IN, USA) system that was used together with the Oxford unicompartmental knee prosthesis (Zimmer-Biomet Ltd, Bridgend, UK). In this study, it was hypothesised that there is no significant difference between the preoperative plan and the actual position of the prosthesis components in vivo by comparing the MRI-based preoperative plan with CT images after surgery.
Materials and methods
Twenty-five patients with a painful and disabled knee joint resulting from unicompartmental medial osteoarthritis were included between September 2013 and May 2014. The included patients fulfilled the criteria for primary Oxford UKA surgery [2], had a body-mass-index (BMI) < 39.0 and were able and willing to follow instructions and return for the postoperative CT-scan. Several patients (n = 0) were excluded from the cohort because of the following reasons: pregnancy (n = 0), former major knee surgery (e.g. correction osteotomy; n = 0), metal near the knee joint (MRI scan not possible; n = 1) and patients not able or willing to undergo an MRI scan or CT-scan (n = 10). After obtaining informed consent, 26 knees in 25 patients were consecutively recruited. Patient demographics can be found in Table 1.
Surgery was performed by one single surgeon (NK) with extensive experience in conventional as well as PSI-based cementless Oxford UKA surgery.
Preoperative MRI scanning of the hip, knee and ankle was performed 6 weeks prior to surgery according to the standard signature scanning protocol. A digital, virtual plan of the operation was then sent to the surgeon. The surgeon was able to adjust the digital plan based on his expertise. All changes in the preoperative planning made by the surgeon regarding size and position of the implant were recorded. All plans were evaluated and approved by the operating surgeon. After the digital plan was approved, guides for intraoperative use were created using a rapid prototype engineering technique (Materialize N.V., Leuven, Belgium). The whole cohort underwent the same surgical procedure using these guides intraoperatively, the practical form and fit of the guides were recorded as potential change to this plan during surgery.
To define the difference between the component position in the preoperative digital plan and the actually achieved postoperative position, a digital plan based on the preoperative MRI scan was compared with the postoperative full-leg CT-scan. Because direct comparison between the preoperative MRI scan and the postoperative CT-scan is difficult and may be inaccurate, an additional preoperative full-leg CT-scan (using the same scanning protocol as the postoperative full leg CT-scan) was made to serve as an intermediate step in the analysis. Consecutively, the preoperative MRI images were matched to the preoperative CT images; digital 3D models were generated for the femur and tibia using software from Materialise NV (Materialise NV, Leuven, Belgium). This type of 3D registration renders the results independent of scan orientation and leg position during scanning. After surgery, 3D reconstruction images of the postoperative CT-scan were superimposed over the preoperative CT images with planned resections and prosthesis placement (Figs. 1, 2). Because both CT scans were made using the exact same scanning protocol, an accurate comparison was made between the preoperatively planned resection surfaces and prosthesis placement and the achieved resection surfaces and the actual position of the prosthesis in vivo. Accuracy of the measurements is within 0.1° [1, 4, 8].
The angular component position and absolute deviations of the preoperative planned angular component position in three planes were determined. The same was done for the translational component position.
Deviations (in degrees) from the preoperative approved planning in all three anatomical planes for femoral and tibial components were compared with the post-operative achieved alignment of each component with the use of a 6-week postoperative long-leg low-dose CT-scan and shape-match measurement technique [1, 8]. The preoperative planned position for the femoral component was 0° varus relative to the mechanical frontal axis of the femur, 10.0° of flexion relative to the mechanical sagittal axis of the femur and 3.0° of external rotation relative to the transepicondylar axis. The planned position of the tibial component was 0° of varus relative to the frontal tibial mechanical axis, 3.0° of posterior slope relative to the sagittal tibial mechanical axis and 0° of external rotation relative to the line perpendicular to the line through the centre of the medial and lateral tibial plateau. For the femoral component, the accepted deviations from the planned position according to the prosthesis manufacturer are − 10.0 to + 10.0° in the frontal plane, − 10.0 to + 5.0 in the sagittal plane and − 5.0 to + 5.0 in the axial plane. For the tibial component, the accepted deviations from the planned position according to the prosthesis manufacturer are − 5.0 to + 5.0° in the frontal plane, − 5.0 to + 5.0 in the sagittal plane and − 5.0 to + 5.0 in the axial plane.
Positive values indicate varus, femoral flexion, posterior tibial slope and external rotation, whereas negative values indicate valgus, femoral extension/anterior tibial slope and internal rotation deviations relative to the preoperatively calculated position. For the translation component, positive values indicate anterior translation, lateral translation and distal translation, whereas negative values indicate posterior translation, medial translation and proximal translation. The accepted deviations from the planned position were set arbitrary from + 2.0 to − 2.0 mm since there is no literature available on this topic. The actual size of the inserted femoral components and tibial components were compared with the preoperative planned sizes. To evaluate the translational accuracy of the guides, extra resections performed intraoperatively were used to recalculate the position of the primary cut, which was determined by the guide.
This prospective cohort study was conducted in compliance with the Helsinki Declaration of 2000 and was approved by the local institutional review board [METC Atrium-Orbis Zuyd, Heerlen, the Netherlands (log no. 12-T-92)]. The study protocol was registered online at the Dutch Trial Register (http://www.trialregister.nl, Nr. NTR4194) and conducted in accordance with the guidelines for Good Clinical Practice (GCP).
Statistical analysis
Statistical analysis was conducted using SPSS (IBM SPSS Statistics, Version 23. Armonk, NY: IBM Corp.).
The postoperative range for the alignment of the mechanical axis of the leg in the frontal plane was based on previous studies; maximal 3.0° of valgus to 3.0° of varus was acceptable with a standard deviation of 10.0° [10]. Based on alpha 0.05 and a difference of 6.0 ± 10.0, a total of 26 UKA surgeries were required to achieve a power of 0.9. The distribution of variables was considered non-parametric and hypotheses were tested using the Wilcoxon signed ranks test, the non-parametric equivalent of the Students T test. Median (range) and proportions (%) were determined for the differences between preoperative planning and postoperative values for all three anatomical planes. Significance levels were set at P ≤ 0.05.
Results
All femoral guides and all but one (96%) tibial guide fitted well onto the native anatomy of the individual patients and no conversions to traditional techniques had to be performed. The tibial guide that could not be placed in the 100% fit position was then held in the best possible position by pushing the guide laterally on the pressure point of the guide at the time of pin drilling. No complications were encountered when drilling the guide pins and fixing the resection blocks.
No extra posterior femoral resections were necessary. In six patients, an additional proximal tibial resection of 2.0 mm was performed. In three patients, an additional tibial resection towards lateral was performed (twice 1.0 mm and once 2.0 mm). A combination of these two additional resections was performed twice (once 2.0 mm extra tibia with 1.0 mm extra towards lateral and once 2.0 mm extra tibia with 2.0 mm towards lateral). Finally, in one patient (the patient in which the tibial guide did not fit well) an additional 2.0 mm of proximal tibia was resected and the slope was increased. In this patient, the tibial resection block was repositioned using the conventional technique. In five of 12 patients (42%) with an additional intra-operative tibial resection, the tibial implant size differed from the preoperative approved plan.
Except for two patients, wherein a bearing thickness of four and five was used, a bearing thickness of three was used.
Results of the angular measurements for the femoral and tibial component are summarized in Tables 2 and 3. Except for the femoral component in the sagittal plane and the tibial component in the axial plane, angular positions were not significantly different than planned. For the femoral component, the ideal alignment was reached in 25 patients (Table 2). For the tibial component, the ideal alignment was reached in 13 patients (Table 3). Results of the translational measurements of the femoral and tibial component are summarized in Tables 4 and 5. All translational positions were not significantly different than planned. The amount and percentage of identical sized approved templates and templates provided by the manufacturer compared to the implant size can be found in Table 6.
Discussion
The most important finding of the present study was that the actual prosthesis component position is according to the preoperative plan and that the guides accurately translate the preoperative plan into the in vivo situation except for the tibial rotational position.
A significant difference between actual position and planned position was present for the sagittal plane of the femoral component and for the axial plane of the tibial component. For the femoral component, this statistical difference may be explained by the large range. Despite this larger range, no outliers are present and all components are within the accepted limits.
The femoral guide worked well, in particular, since the contact area is large and a perfect fit was easily found. For the tibial guide the contact area is smaller and attention should be addressed to lateral osteophytes of the medial femoral condyle since they can push the guide into external rotation and out of the perfect fit position. This phenomenon was also seen in another study, concerning revision surgery from UKA to TKA using PSI [17]. Another factor that may influence tibial component rotation is a re-resection of the lateral wall in patients where medial overhang of the plateau is present, because these re-resections are not performed with a slotted device. To prevent this re-cut, it is important to plan the tibial component in a rather lateral position. The third factor that may explain tibial rotation is that the definitive rotational position is not only determined by the lateral cut but also by the cut for the keel, which is made through the test plateau. The optimal position of this test plateau is not always parallel with the lateral cut, but depends on the medial tibial contour as well. This can explain the rotational difference between the planned and definitive tibial component position. The statistical difference for the tibial rotational component between postoperative position and planned position thus cannot be attributed solely to the guide.
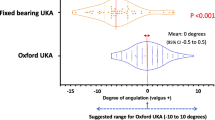
In the literature, it is reported that when using PSI the tibial component is positioned in a mean 6.5–11.9° of external rotation with extremes up to 32.0° of external rotation [7, 18]. The exact impact of the rotational component of the tibia is not yet fully understood and may depend on the type of implant [6, 18, 20, 21].
Since the bearing size depends on intra-operative ligament balancing and the definitive axial position of the tibial component, the size of the bearing was not preoperatively planned. The Y-axis position of the femoral component also depends on ligament balancing and was, therefore, determined intra-operatively using the spigot and spherical mill. Finally, the Z-axis position of the tibial component is not planned but determined during surgery by placing the test plateau more anterior or posterior in the best position.
The horizontal cut for the tibial component also determines the size of the bearing. To reach the required space to insert a bearing with minimal thickness of 3.0 mm, we had to perform a horizontal re-resection of the proximal tibia of 2.0 extra mm in eight patients. With these re-resections, the final prosthesis components were placed in the proper position. The re-resections indicate that these tibial components were not planned in the perfect position to provide sufficient space for a bearing of three. To prevent distal recuts that can cause angular deviations, it is important to plan the tibial component in a rather distal position. These re-resections explain the need to change the tibial component size in our patients.
The one patient in whom the guide did not fit well stresses the importance of the expertise and training of the surgeon. While the PSI technique could be of value in less experienced surgeons, the general applicability is a point of discussion. Most research is performed with high-volume surgeons, who may adapt faster to a new technique [3].
Besides the presence of femoral osteophytes, another possible reason for an ill-fitting guide can be soft tissue that is not removed properly and then interferes with guide contact points. Since the time between MRI planning and actual operation was not more than 2 months, a progression of anatomic deformity is not likely. A final influence on guide fitting is the segmentation of the MRI images. In this process of segmentation, each pixel on the image is identified as bone, cartilage or soft tissue. This process is performed by a human engineer and not by a computer. Theoretically, errors made during this process can explain a bad guide fit. In retrospect, this was not the case since re-evaluation of the segmentation in individual patients was performed and found to be correct. As mentioned before, the longevity of the prosthesis increases when the biomechanics of the joint are restored. This study shows that, except for the tibial rotation, the prosthesis is placed according to the preoperative plan. In this study, financial advantages are not researched; however, previous research shows that an improved operation room efficacy could possibly reduce costs [16]. Furthermore, supply and demand could be more accurately predicted with the PSI technique, allowing to reduce the stock need and reduce less over date prosthesis components [16].
The results are promising; however, there were several limitations to the present study. The study included only a limited number of patients all operated by one surgeon. Larger patient series will be needed to confirm these preliminary results. In addition, this was not a randomised controlled trial. Third, all prosthesis and accompanying instruments were from the same manufacturer, and therefore, our results may not be widely applicable. Furthermore, more research is needed on the financial aspect of the PSI technique.
Conclusion
PSI in Oxford UKA surgery is reliable and it accurately translates the preoperative plan into the in vivo situation. The preoperative planning is a crucial step in avoiding re-resections that can cause angular deviations in prosthesis position in vivo. It is advised to prevent re-resections and to consider this while planning your PSI procedure.
References
Boonen B, Schotanus MG, Kerens B, Hulsmans FJ, Tuinebreijer WE, Kort NP (2015) Patient-specific positioning guides for total knee arthroplasty: no significant difference between final component alignment and pre-operative digital plan except for tibial rotation. Knee Surg Sports Traumatol Arthrosc 25(9):2809–2817
Goodfellow J, O’Connor J, Dodd C, Murray D (2006) Unicompartmental arthroplasty with the Oxford Knee. Oxford University Press, Oxford, p 190
Hamilton WG, Parks NL, Saxena A (2011) Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty 28:96–100
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J B Jt Surg Br 93:629–633
Hooper N, Snell D, Hooper G, Maxwell R, Frampton C (2015) The 5-year radiological results of the uncemented Oxford medial compartment knee arthroplasty. B Jt J 97–B:1358–1363
Iriberri I, Aragón JF (2014) Alignment of the tibial component of the unicompartmental knee arthroplasty, assessed in the axial view by CT-scan: does it influence the outcome? Knee 21(6):1269–1274
Jenny JY, Boeri C (2003) Unicompartmental knee prosthesis implantation with a non-image-based navigation system: rationale, technique, case-control comparative study with a conventional instrumented implantation. Knee Surg Sports Traumatol Arthrosc 11:40–45
Jonkergouw F, Allé F, Chellaoui K, Vander Sloten J, Vangeneugden D (2016) Three-dimensional measurement technique to assess implant position and orientation after total knee arthroplasty. Med Eng Phys 38(12):1513–1517
Jung KA, Kim SJ, Lee SC, Hwang SH, Ahn NK (2010) Accuracy of implantation during computer-assisted minimally invasive Oxford unicompartmental knee arthroplasty: a comparison with a conventional instrumented technique. Knee 17:387–391
Kendrick BJ, Kaptein BL, Valstar ER, Gill HS, Jackson WF, Dodd CA, Price AJ, Murray DW (2015) Cemented versus cementless Oxford unicompartmental knee arthroplasty using radiostereometric analysis: a randomised controlled trial. B Jt J 97–B:185–191
Kerens B, Schotanus MG, Boonen B, Kort NP (2015) No radiographic difference between patient-specific guiding and conventional Oxford UKA surgery. Knee Surg Sports Traumatol Arthrosc 23:1324–1329
Liow MH, Tsai TY, Dimitriou D, Li G, Kwon YM (2016) Does 3-dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty 31(10):2167–2172
Lisowski LA, van den Bekerom MP, Pilot P, van Dijk CN, Lisowski AE (2010) Oxford phase 3 unicompartmental knee arthroplasty: medium-term results of a minimally invasive surgical procedure. Knee Surg Sports Traumatol Arthrosc 19:277–284
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2015) The clinical outcome of minimally invasive phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. B Jt J 97–B:1493–1500
Renson L, Poilvache P, Van den Wyngaert H (2014) Improved alignment and operating room efficiency with patient-specific instrumentation for TKA. Knee 21:1216–1220
Schotanus MGM, Schoenmakers DAL, Sollie R, Kort NP (2015) Patient-specific instruments for total knee 247 arthroplasty can accurately predict the component size as used peroperative. Knee Surg Sports Traumatol Artrosc. https://doi.org/10.1007/s0016701643451
Schotanus MGM, Thijs E, Boonen B et al (2017) Revision of partial knee to total knee arthroplasty with use of patient-specific instruments results in acceptable femoral rotation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4674-8
Servien E, Fary C, Lustig S et al (2011) Tibial component rotation assessment using CT-scan in medial and lateral unicompartmental knee arthroplasty. Orthop Traumatol Surg Res 97(3):272–275
Trong MLD, Diezi C, Goerres G, Helmy N (2015) Improved positioning of the tibial component in unicompartmental knee arthroplasty with patient-specific cutting blocks. Knee Surg Sports Traumatol Artrosc 23:1993–1998
Tsai TY, Dimitriou D, Liow MH, Rubash HE, Li G, Kwon YM (2016) Three-dimensional imaging analysis of unicompartmental knee arthroplasty evaluated in standing position: component alignment and in vivo articular. Contact J Arthroplasty 31(5):1096–1101
van Leeuwen JA, Röhrl SM (2016) Patient-specific positioning guides do not consistently achieve the planned implant position in UKA. Knee Surg Sports Traumatol Arthrosc 3:752–758
Acknowledgements
The authors would like to thank Drs. M. Keulen, M.D., from the Dell Medical School at the University of Texas in Austin, USA, who served as external reader, and for his comments that greatly improved the manuscript.
Author information
Authors and Affiliations
Contributions
BK participated in the design of the study, acquisition of data and writing of the manuscript. AL participated in the design of the study and helped to draft the manuscript. MS participated in the design of the study and acquisition of data and helped to draft the manuscript. BB participated in the design of the study and helped to draft the manuscript. WT participated in the statistical analysis and helped to draft the manuscript. BJ participated in the design of the study and helped to draft the manuscript. PE participated in the design of the study and helped to draft the manuscript. NK participated in the design of the study and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
One author (NK) is a paid consultant for Zimmer-Biomet. The other authors have no conflict of interest to be reported.
Funding
No funding has been received for this study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kerens, B., Leenders, A.M., Schotanus, M.G.M. et al. Patient-specific instrumentation in Oxford unicompartmental knee arthroplasty is reliable and accurate except for the tibial rotation. Knee Surg Sports Traumatol Arthrosc 26, 1823–1830 (2018). https://doi.org/10.1007/s00167-017-4826-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4826-x