Abstract
Purpose
To determine (1) whether a correlation exists between tibial tubercle–posterior cruciate ligament (TT-PCL) and tibial tubercle–trochlear groove (TT-TG) distances in patellar instability patients; (2) reliability when measuring TT-PCL distance; (3) whether TT-PCL distances measured on MRI are equivalent to those on CT; and (4) whether a correlation exists between TT-PCL distance and number of instability events or recurrence of instability following stabilization surgery.
Methods
A systematic review was performed using PRISMA guidelines. Clinical studies investigating the relationships of TT-PCL with TT-TG on CT and/or MRI in patellar instability patients were sought. English language studies with Levels of evidence I–IV were eligible for inclusion.
Results
Four studies (285 subjects [300 knees] with patellar instability [74.2% female; mean age 26.1 ± 8.2 years]; 114 controls [144 knees; 77% female; mean age 23.1 years]) were included. Mean TT-PCL of instability and control groups was 21.1 ± 4.1 and 18.8 ± 4.0 mm (p < 0.0001), respectively. Two studies reported significant positive (strong and moderate) correlations between TT-PCL and TT-TG MRI measurements in instability patients. All four investigations reported excellent interobserver and intraobserver reliability in MRI measurement of TT-PCL distance. No study compared TT-PCL distances on MRI and CT. No study assessed correlation between TT-PCL distance and number of instability events or recurrence of instability after surgery.
Conclusion
A moderate-to-strong positive correlation exists between TT-PCL and TT-TG measurements taken from MRIs of patellar instability patients. There is excellent interobserver and intraobserver reliability when taking TT-PCL measurements using MRI. This review advocates use of a new pathologic TT-PCL threshold of 21 mm.
Level of evidence
Level III, systematic review of Level II–III studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patellar instability can be a challenging problem for athletes and non-athletes alike. Recurrent instability that is recalcitrant to non-operative measures can be treated with surgery including procedures like medial patellofemoral ligament (MPFL) reconstructions and tibial tubercle osteotomies. To determine whether a distal realignment procedure is necessary, the tibial tubercle–trochlear groove (TT-TG) distance is often utilized [13]. This radiographic parameter was originally described by Goutallier et al. [7]. More recently, TT-TG has been measured using computed tomography (CT) as opposed to radiographs [6, 7]. Axial images through the tibial tubercle and trochlear groove are superimposed over each other, and a value greater than or equal to 20 mm between the two points is considered a risk factor for patellar instability. The tibial tubercle–posterior cruciate ligament (TT-PCL) distance is an alternative measurement developed to more accurately describe true lateralization of the tibial tubercle because TT-TG measurements are subject to variation in the face of trochlear dysplasia and varying degrees of knee flexion [13]. Abnormal TT-PCL distance includes values greater than 24 mm; however, the sensitivity and specificity of this value in the assessment of recurrent patellar instability were found to be 0.298 and 0.583, respectively [9]. The first study comparing abnormal TT-PCL and TT-TG distances did not find a strong correlation between the two measures, but this study applied CT-derived TT-TG cut-off values to magnetic resonance imaging (MRI) which are not equivalent [4, 13].
The purpose of this investigation was to perform a systematic review (1) to determine whether a correlation exists between TT-PCL distance and TT-TG distance in the evaluation of patients with patellar instability; (2) to determine whether there is interobserver and intraobserver reliability when measuring TT-PCL distance; (3) to determine whether TT-PCL distances measured on MRI are equivalent to those measured on CT; and (4) to determine whether there is a correlation between TT-PCL distance and the number of patellar instability events or recurrence of patellar instability following soft tissue patellar stabilization surgery. The study hypotheses were: (1) TT-PCL distance would have a positive correlation with TT-TG distance in the evaluation of patients with patellar instability; (2) there would be excellent interobserver and intraobserver reliability when measuring TT-PCL distance; (3) TT-PCL distances measured on MRI would differ from those taken on CT; and (4) TT-PCL distance would have a positive correlation with number of instability events and with recurrence of patellar instability following soft tissue stabilization surgery.
Materials and methods
Identification of literature
A systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 28 July 2016 (registration ID: CRD42016043724). Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed [10]. Electronic searches were conducted separately by two authors (** and ***) on 29 July 2016 and repeated on 30 January 2017. All combinations of search phrases “Tibial Tubercle Posterior Cruciate Ligament”, “Tibial Tuberosity Posterior Cruciate Ligament”, and “TT-PCL” were entered as subject headings for searches in the following databases: MEDLINE, Scopus, SPORTDiscus, and Cochrane Central Register of Controlled Trials. Clinical studies investigating the relationships of TT-PCL with TT-TG on CT and MRI were sought for inclusion.
Selection criteria
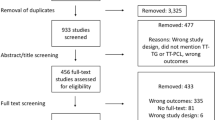
English language diagnostic, therapeutic, or prognostic studies with Levels of evidence I–IV were eligible for inclusion. There was no limit placed on clinical follow-up. Level V evidence, non-English articles, abstracts, and book chapters were excluded. Duplicate studies comprising the same subjects were eligible for inclusion, but the study with the highest level of evidence, greater(est) number of subjects, or longest follow-up that was relevant to the topic of this review was included for final analysis and the other(s) was(ere) excluded. TT-PCL measurements were defined as “the mediolateral distance [parallel to the dorsal tibial condylar line] between the midpoint of the insertion of the patellar tendon and medial border of the PCL” on axial views of the tibia [13]. The most caudal axial MRI view, in which the PCL was visible, was used for the PCL point. TT-TG measurements were defined as the mediolateral distance (parallel to the dorsal femoral condylar line) between the midpoint of the patellar tendon insertion and the deepest point of the trochlear groove on axial images. Studies that used alternate means or modifications in taking TT-PCL and TT-TG measurements were excluded. All titles acquired from the electronic search were screened, and inclusion/exclusion criteria were applied to select relevant articles for the qualitative synthesis (Fig. 1—PRISMA flow chart).
Data extraction and analysis
Two authors (** and ***) reviewed each remaining article independently using the methodology recommended by Harris et al. [8]. Data extracted from these articles included study title, authors, publication date, journal, level of evidence, study type and design, involvement of a single centre versus multicentre, country of origin, conflict of interest reporting, primary/secondary purpose, hypothesis, inclusion/exclusion criteria, years of patient enrolment, outcome measures, number of patients enrolled (including breakdown in number of patellar instability/control patients, male/female patients, and number of knees studied in each of the aforementioned groups, concurrent injuries), mean age, number of providers performing the study, blinding, results, and limitations. Knee analysis data extracted from each article included history of single versus multiple instability events, history of prior knee surgery, presence of arthritis or other knee pathology, TT-PCL and TT-TG measurements, imaging modality used to take each measurement, inter- and intraobserver reliability of measurements, and statistical significance of outcome data from individual studies (Tables 1, 2).
The two reviewers graded quality of study methodology using the “STrengthening the Reporting of OBservational studies in Epidemiology (STROBE)” checklist of items to be contained in an observational study [17] and computed an individual Methodological Index for Non-Randomized Studies (MINORS) score for each article [15]. The MINORS scoring system appraises 8 components for non-comparative studies and 12 components for comparative studies. Components are graded on a scale from 0 to 2 based on reporting and adequacy of methodology for a potential total of 16 and 24 points for non-comparative and comparative studies, respectively. MINORS scores for each article were reported as both raw scores and percentages. Quality of evidence was determined using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system [2]. According to the GRADE system, an initial grade of “low” is applied to observational studies but the final grade could potentially rise to “moderate” or “high” or drop down to “very low” depending on limitations, consistency, directness, and strength of association of data within the article. The overall quality of evidence for the studies included was to be judged by the authors, after the three different methodological scoring systems were employed, on a spectrum of “excellent”, “good”, “fair”, and “poor”.
Homogeneous outcome data between studies would be combined for meta-analysis, and if heterogeneous outcome data existed between studies, then a best-evidence synthesis would be performed [14]. Correlations would be described as positive or negative, and the absolute value of the correlation would be given a strength designation as follows: a value of zero indicates no linear relationship, values ranging from 0.3 to 0.5 would be weak, values ranging from 0.5 to 0.7 would be moderate, and values from 0.7 to 1 would be strong (where a value of 1 would signify a perfect linear relationship between two variables) [11].
Results
Four studies (285 subjects [300 knees] with patellar instability [74.2% female, 25.8% male; mean age 26.1 ± 8.2 years]; 114 control subjects [144 knees; 77% female, 23% male; mean age 23.1 years]) were included for analysis (patient demographics not provided in Daynes et al. study) [1, 5, 9, 13]. All four articles compared TT-TG measurements to TT-PCL measurements (Tables 1, 2). Each article also assessed observer reliability in obtaining TT-PCL distances using MRI. Only one article assessed for differences between measurements taken on CT and MRI [1]. Using MRI, mean TT-PCL of patellar instability (n = 300 knees) and control (n = 144 knees) groups was 21.1 ± 4.1 and 18.8 ± 4.0 mm (p < 0.0001), respectively [1, 5, 9, 13]. Using MRI, mean TT-TG of patellar instability (n = 300 knees) and control (n = 144 knees) groups was 15.1±5.5 and 10.8±4.3 mm (p < 0.0001), respectively [1, 5, 9, 13]. Methodology and quality of evidence of all studies were evaluated using three scoring systems (Table 3). Included studies reported 21.3 out of 22 items suggested by the STROBE checklist for observational studies. Mean MINORS score was 10.5 out of 16 for non-comparative studies and 17 out of 24 for comparative studies. Quality of evidence using the GRADE system resulted in a mean final grade of “low”. Based on the scores from these three separate grading systems, the authors each independently deemed the overall quality of the studies included as “fair” on a spectrum of “excellent”, “good”, “fair”, and “poor”.
Three of the four studies correlated TT-TG measurements taken in each patient to TT-PCL measurements [1, 5, 13]. Daynes et al. reported a significant strong positive correlation between abnormal TT-PCL and TT-TG measurements in patellar instability patients (n = 42 knees) [5]. Seitlinger et al. reported a moderate correlation between the TT-PCL and TT-TG using MRI [13]. Anley et al. reported 25% of patients with an abnormal TT-TG on CT also had an abnormal TT-PCL on MRI [1].
Using MRI, interobserver reliability in TT-PCL measurements was calculated in all four studies, while intraobserver reliability was calculated in only three of the four studies [1, 5, 13]. Average inter- and intraobserver reliability amongst the studies was 0.88 and 0.92, respectively, indicating excellent reliability in TT-PCL measurements.
The difference between measurements taken on CT and MRI was evaluated by Anley et al. [1]. Mean TT-TG distance was 4.2 mm smaller on MRI than on CT (p < 0.05). No study compared TT-PCL distances on MRI and CT.
No study assessed correlation between TT-PCL distance and number of patellar instability events or recurrence of such events after soft tissue patellar stabilization surgery.
Discussion
The most important finding of the present study was the mean TT-PCL distance of 21.1 ± 4.1 mm in patellar instability patients. This systematic review establishes TT-PCL distance as a reliable measurement amongst observers from multiple studies. A moderate-to-strong positive correlation was demonstrated between abnormal TT-PCL and TT-TG distances in patients with patellar instability. The first two study hypotheses were confirmed, while the last two could neither be confirmed nor rejected due to lack of available evidence in the literature.
The overall moderate-to-strong positive correlation found between abnormal TT-PCL and abnormal TT-TG measurements on MRI indicates that different anatomical factors may be at play in causing abnormal measurements for each. The purpose of the original study describing the TT-PCL distance was to introduce a measurement that elucidated true lateralization of the tibial tubercle because TT-TG distance not only varied with knee rotation, but could also be difficult to measure in patients with trochlear dysplasia [13]. The TT-PCL distance could help to differentiate those patients with abnormal TT-TG distances who needed distal realignment procedures from those who did not. Subsequent studies have reaffirmed the notion that an abnormal TT-TG distance is dependent on a variety of anatomical factors, not just isolated lateralization of the tibial tubercle, whereas the TT-PCL distance is the result of tibial tubercle position alone [1, 5, 9]. Furthermore, patients with patellar dislocations have been found to have multiple contributing factors to their instability [16]. This substantiates the idea to use both measurements in concert when evaluating for the underlying anatomical aetiology of a patellar instability event. That being said, perhaps the greatest potential reason that a stronger correlation is not found between the two measurements in this review could be a function of the threshold used to define an abnormal TT-PCL distance. In the original study describing the TT-PCL distance, Seitlinger et al. found 95% of control subjects to have TT-PCL measurements less than 24 mm, a value that they then established as the cut-off for normal [13]. This is in stark contrast to the method by which the cut-off value for abnormal TT-TG distance was determined. While Goutallier et al. described the concept radiographically, it was the work of Dejour et al. that found the mean TT-TG distance on CT scans of patellar instability patients to be 19.8 mm, favouring the use of the pathologic 20 mm cut-off value [6, 7]. Had Seitlinger et al. used the mean TT-PCL distance found in their instability group (21.9 mm) to establish the pathologic threshold as opposed to the value at which 95% of controls fell under (24 mm), then there would have likely been stronger correlations between TT-PCL and TT-TG distances not just in their study but throughout the literature. This supports the use of a new pathologic TT-PCL cut-off value of 21 mm as determined by the mean TT-PCL value for patellar instability patients (21.1 mm) found in this review [1, 5, 9, 13].
One of the postulated benefits of measuring the TT-PCL distance was to eliminate the difficulty and resultant interobserver variability of taking TT-TG measurements in patients with trochlear dysplasia [13]. This study found excellent reliability in taking TT-PCL measurements; however, similar reliability has been found when taking TT-TG measurements [3, 9]. This indicates that although utilization of the TT-PCL measurement may remove the variability in defining the trochlear groove point, it may just as equally increase variability through determination of the PCL point.
Two study hypotheses were not evaluated by any study. One study hypothesis, that TT-PCL distances measured on MRI would differ from those taken on CT, can be inferred to be true based on similar findings when taking TT-TG measurements using both imaging modalities [1, 4]. Anley et al. evaluated TT-TG measurements between the two imaging modalities and attributed the difference found to be due to “variation in MRI protocols, MRI scanners, and the use of different knee coils”. The final study hypothesis, that TT-PCL distance would have a positive correlation with number of instability events and with recurrence of patellar instability following soft tissue stabilization surgery, is perhaps the most clinically relevant hypothesis to surgeons when discussing treatment options and outcomes with patients. Future studies are necessary to further elucidate any potential correlations.
This review is limited by the retrospective nature of the studies included. As such, the studies do not all give the exact detail with which imaging was obtained (like the brand and name of the machines used or the amount of flexion each knee was held in during the examination). Perhaps the largest limitation of these studies has already been mentioned the manner in which the abnormal TT-PCL cut-off value was established. As previously discussed, this review advocates the establishment of a new TT-PCL threshold (21 mm) based on mean MRI measurements of patellar instability patients rather than controls. It is possible that the statistically significant difference between TT-PCL measurements of patellar instability and control patients is not a clinically significant difference, but further research is necessary [12]. Another limitation of this review is that the established CT scan cut-off value for abnormal TT-TG distance (≥ 20 mm) was used interchangeably on MRI despite evidence that on average, CT measurements of such values are 3.8–4.16 mm greater than those found on MRI [1, 4]. This difference in measurements is likely the reason why Anley et al. [1] only found a 25% association between abnormal TT-TG (on CT) and abnormal TT-PCL (on MRI) when the other two studies assessing correlation between the two measurements used the same imaging modality (MRI) and found a moderate-to-strong correlation [5, 13]. To be more accurate, authors comparing TT-TG to TT-PCL using MRI should have adjusted the abnormal TT-TG cut-off for use on MRI and used smaller cut-off values in their studies. Likewise, if the TT-PCL threshold (as determined by MRI) is to be used in a clinical setting, physicians should be cognizant of which imaging modality they are using and know that measurements on MRI and CT are not equal. The overall “fair” study quality is another potential limitation. The methodological quality of the studies included in this review, in terms of meeting criteria on the STROBE checklist, collectively demonstrated around 97% compliance. However, these same studies received a MINORS score of 68.2%. Based on the GRADE system, the average grade for quality of evidence was “low” and this is the expected score for an observational study.
The clinical relevance of this review is that it defines a more accurate pathologic TT-PCL threshold of 21 mm and establishes TT-PCL distance as a measurement that can be reliably obtained amongst different observers. This review suggests TT-PCL distance should be used in tandem with TT-TG distance in the clinical setting when evaluating patients with patellar instability. Also, physicians should be weary of using MRI and CT measurements interchangeably as measurements from these modalities are not equivalent.
Conclusion
A moderate-to-strong positive correlation exists between TT-PCL and TT-TG measurements taken from MRIs of patients with patellar instability. There is excellent inter- and intraobserver reliability when taking TT-PCL measurements using MRI. No study has compared MRI and CT TT-PCL measurements. No study has assessed correlation between TT-PCL distance and number of patellar instability events or recurrence of such events after soft tissue patellar stabilization surgery. The results of this review advocate the use of a new pathologic TT-PCL threshold of 21 mm.
Abbreviations
- TT-PCL:
-
Tibial tubercle–posterior cruciate ligament
- TT-TG:
-
Tibial tubercle–trochlear groove
References
Anley CM, Morris GV, Saithna A et al (2015) Defining the role of the tibial tubercle-trochlear groove and tibial tubercle-posterior cruciate ligament distances in the work-up of patients with patellofemoral disorders. Am J Sports Med 43(6):1348–1353
Atkins D, Best D, Briss PA et al (2004) Grading quality of evidence and strength of recommendations. BMJ 328(7454):1490–1494
Camp CL, Heidenreich MJ, Dahm DL et al (2016) A simple method of measuring tibial tubercle to trochlear groove distance on MRI: description of a novel and reliable technique. Knee Surg Sports Traumatol Arthrosc 24(3):879–884
Camp CL, Stuart MJ, Krych AJ et al (2013) CT and MRI measurements of tibial tubercle–trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med 41(8):1835–1840
Daynes J, Hinckel BB, Farr J (2016) Tibial tuberosity-posterior cruciate ligament distance. J Knee Surg 29(6):471–477
Dejour H, Walch G, Nove-Josserand L et al (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2(1):19–26
Goutallier D, Bernageau J, Lecudonnec B (1978) The measurement of the tibial tuberosity. Patella groove distanced technique and results. Rev Chir Orthop Reparatrice Appar Mot 64(5):423–428
Harris JD, Quatman CE, Manring MM et al (2014) How to write a systematic review. Am J Sports Med 42(11):2761–2768
Heidenreich M, Camp CL, Dahm DL et al (2017) The contribution of the tibial tubercle to patellar instability: analysis of tibial tubercle-trochlear groove (TT-TG) and tibial tubercle–posterior cruciate ligament (TT-PCL) distances. Knee Surg Sports Traumatol Arthrosc 25(8):2347–2351
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Int Med 151(4):264–269
Moore DS, Notz WI, Flinger MA (2013) The basic practice of statistics, 6th edn. WH Freeman and Company, New York
Rossi MJ (2016) Editorial commentary: tibial tubercle-trochlear groove distance as an independent risk factor for noncontact anterior cruciate ligament injury is possible but remains uncertain. Arthroscopy 32(1):69–70
Seitlinger G, Scheurecker G, Högler R et al (2012) Tibial tubercle-posterior cruciate ligament distance a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med 40(5):1119–1125
Slavin RE (1995) Best evidence synthesis: an intelligent alternative to metaanalysis. J Clin Epidemiol 48(1):9–18
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Tompkins MA, Arendt EA (2015) Patellar instability factors in isolated medial patellofemoral ligament reconstructions—what does the literature tell us? A systematic review. Am J Sports Med 43(9):2318–2327
Von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med 45(4):247–251
Author information
Authors and Affiliations
Contributions
NB, DAD, JDH contributed to study conception, design, data acquisition, analysis, interpretation of data, /drafting of the manuscript, critical revision of the manuscript, final approval of the manuscript and agree to be accountable for all aspects of the work. JSL, PCM, DML involved in study conception, design, analysis, interpretation of data, critical revision of the manuscript, final approval of the manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
Authors NB, DAD, JSL, and DML declare no conflict of interest. Author PCM is on the Speaker’s Bureau for company/supplier (Vericel), receives research support from company/supplier (DePuy, A Johnson & Johnson Company; Arthrex; Zimmer), is on the editorial board for Journal of Knee Surgery, Orthobullets.com. Author JDH is on the Editorial board for Arthroscopy: The Journal of Arthroscopic and Related Surgery, Frontiers In Surgery; receives publication royalties from SLACK, Inc; receives research support from Depuy Synthes, Smith & Nephew; is a paid consultant for NIA Magellan, Smith & Nephew; is on committees for AANA Research, AOSSM Self-Assessment, AAOS Osteoarthritis Pain and Function Workgroup.
Funding
No funding was received for this study.
Ethical approval
This manuscript complies with current ethical standards of research. As this was a synthetic analysis of previously published studies, no new subjects were analyzed, this study was exempt from Institutional Review Board.
Rights and permissions
About this article
Cite this article
Boutris, N., Delgado, D.A., Labis, J.S. et al. Current evidence advocates use of a new pathologic tibial tubercle–posterior cruciate ligament distance threshold in patients with patellar instability. Knee Surg Sports Traumatol Arthrosc 26, 2733–2742 (2018). https://doi.org/10.1007/s00167-017-4716-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4716-2